At this year’s Medidays, a keynote lecture was devoted to hyperlipidemia and hypertension. In the area of the former condition, PCSK9 inhibitors, among others, are making a splash. Prof. Dr. med. Edouard Battegay, Zurich, gave an overview of current therapeutic options. Combination therapies are often used in the course of hypertension treatment. What is the best way to combine the active ingredients and what is important with regard to the duration of action or the effect? nocturnal blood pressure lowering to consider? PD Dr. med. Lukas Zimmerli, Olten, went into these questions in more detail.
Prof. Dr. med. Edouard Battegay, Zurich, spoke about the therapy of hyperlipidemia. Some selected aspects of his presentation are taken up below.
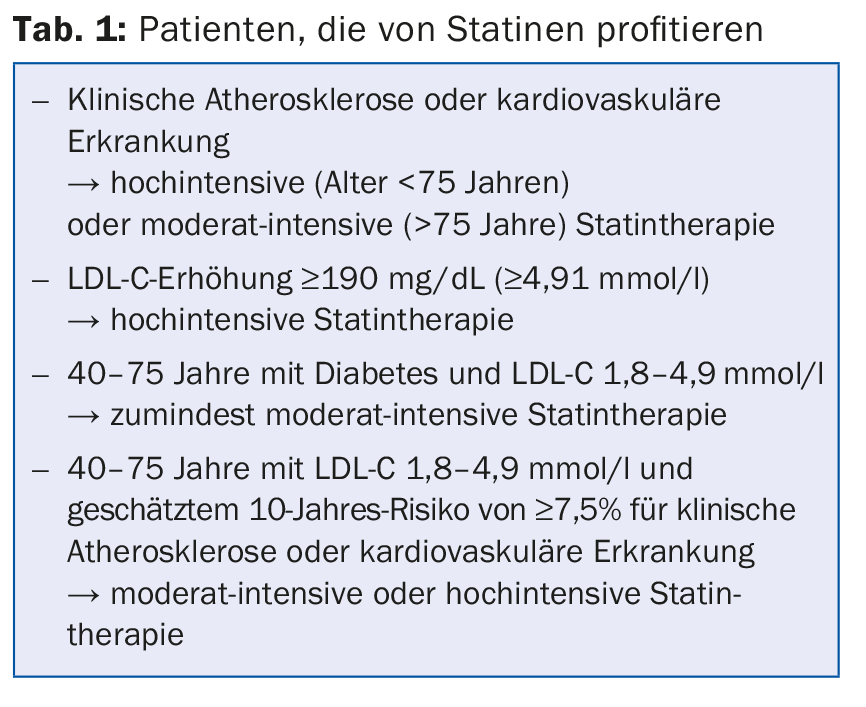
Priority for dyslipidemia is lifestyle modifications. In addition, statins are considered the therapy of choice. In secondary prevention, they reduce both cardiovascular and all-cause mortality. In primary prevention, statins significantly reduce cardiovascular mortality, but consistent results in reducing all-cause mortality are lacking. A review of the inconsistent data from meta-analyses reveals a modest relative risk reduction in all-cause mortality in the order of about 10% with statin treatment. Baseline risk is critical to the benefit (and cost-effectiveness) of therapy: the higher the cardiovascular risk, the greater the benefit. At low risk, lifestyle changes are a priority in any case. Table 1 summarizes which patients particularly benefit from statingabe.
An alternative to high-dose statin therapy is the combination of ezetimibe and a statin. Studies have shown that simvastatin and ezetimibe together provide potent LDL-C lowering. IMPROVE-IT [1], the largest and longest study in this field, had demonstrated a significant reduction in the combined primary endpoint using data from 18,144 participants hospitalized for acute coronary syndrome within the preceding 10 days and a follow-up of approximately 7 years (simvastatin 40 mg/ezetimibe 10 mg vs. simvastatin 40 mg: HR 0.936, p=0.016, NNT=50). This consisted of cardiovascular death, myocardial infarction, documented unstable angina with rehospitalization, coronary revascularization (≥30 days after randomization), or stroke.
PCSK9 inhibitors – promising data situation
A new principle for LDL lowering are the so-called PCSK9 inhibitors. These show a great effect with few side effects at the same time. Normally, the LDL receptor on the surface of liver cells is recycled and returned to the cell surface approximately 100 times. PCSK9 is a protein that inhibits LDL receptor reverse transport and thus its effectiveness, and instead promotes its degradation. Inhibitors of the protein prevent this degradation and increase the number of LDL receptors and thus the uptake of LDL-C from the blood into the liver.
Last year, CARDIOVASC 5/2014 reported on the ODYSSEY study program, which attracted attention at ESC 2014. In this study, the PCSK9 inhibitor alirocumab was investigated. A long-term study [2] belonging to this program with 2341 participants (high cardiovascular risk and LDL-C ≥70 mg/dL or 1.8 mmol/l) now showed that patients receiving alirocumab in addition to existing therapy achieved an average LDL-C reduction of 61% after 24 weeks, while placebo patients (statin or combination therapy only) shared a 0.8% increase (p<0,001). Furthermore, the treatment effect persisted: The difference remained significant for 78 weeks. The safety profile was also favorable, with a post-hoc analysis showing a significant reduction in the rate of major cardiovascular events with alirocumab (1.7% vs. 3.3% with placebo or statin/combination therapy alone).
In a meta-analysis published in July, PCSK9 inhibitors reduced both all-cause and cardiovascular mortality overall [3]. And what happened to the HDL increase? “HDL elevation is only successful with lifestyle modifications. Drug approaches have so far been without clinical success. Unfortunately, CETP inhibition did not produce convincing results,” said Prof. Battegay.
Hypertension: As a rule, combination therapy is necessary
Figure 1 provides an overview of the selection of substances. Monotherapy is indicated for mild/moderate risk and systolic blood pressure of 140-159 and/or diastolic of 90-99 mmHg. This may still be used at ≥160 (systolic) or ≥100 mmHg (diastolic) as an alternative to combination therapy. For high or very high risk and the former blood pressure levels, both monotherapy and combination therapy are possible, whereas for higher blood pressure, combination therapy is certainly indicated.
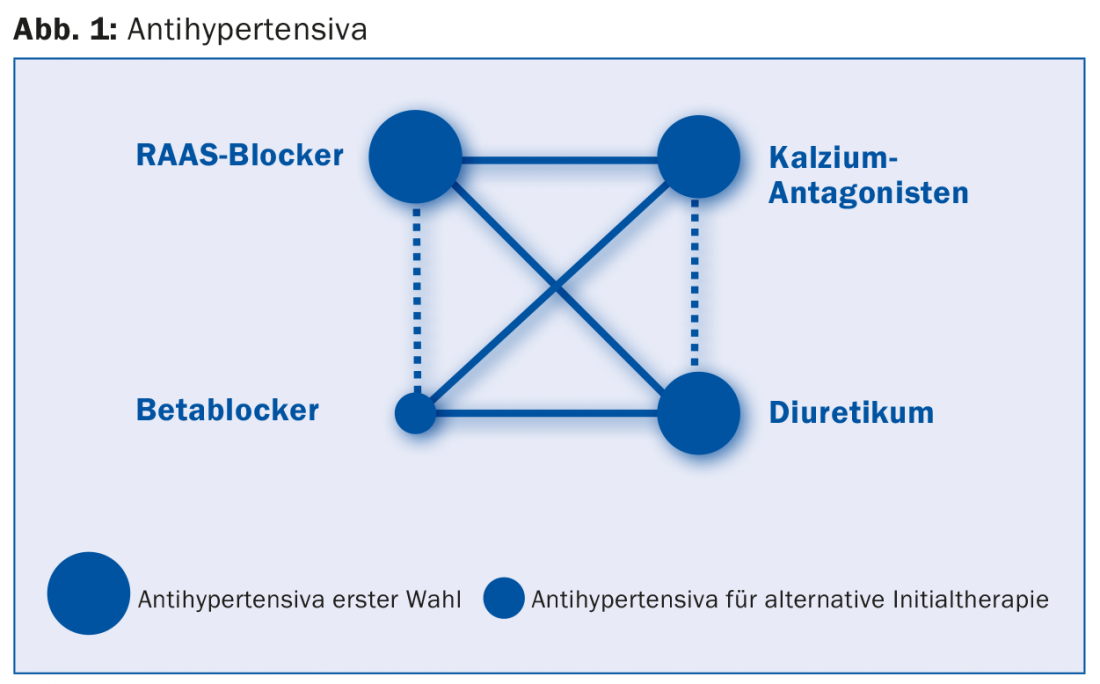
In case of resistance to therapy with a RAAS blocker, a diuretic, and a calcium antagonist, the administration of a beta-blocker, an alpha-blocker, or a centrally acting sympatholytic can be evaluated in addition. Contraindications and drug interactions must of course always be taken into account. In addition, low-dose diuretics should be used because of the threat of hypokalemia.
“Since monotherapy alone is often not sufficient, the question of which combination therapy is indicated usually arises soon in the course of therapy,” says Dr. Zimmerli. “As a two-drug combination, should we use A (ACE inhibitor or ARB) + C (calcium antagonist) or rather A + D (diuretic)?” According to a randomized double-blind trial [4] of 11 506 high-risk patients, the A/C combination is clearly superior to the A/D combination: In the composite primary endpoint consisting of cardiovascular death and various cardiovascular events, benazepril/amlodipine showed a 20% risk reduction compared with benazepril/hydrochlorothiazide (HR 0.80; 95% CI 0.72-0.90; p<0,001).
The second question that arises is: ACE inhibitor or ARB? According to a 2012 meta-analysis [5], ACE inhibitors show a significantly greater reduction in all-cause mortality (HR 0.9, p=0.004 vs. HR 0.99; p=0.683 among ARBs). A 2015 number-needed-to-treat analysis reached similar conclusions [6]: ACE inhibitors but not ARBs reduce all-cause and cardiovascular mortality.
A possible third question concerns the difference between thiazide and thiazide-like diuretics. To date, there is no evidence of benefit from low-dose thiazide vs. placebo. In comparison with other agents, low-dose thiazide was inferior (see the ANBP2, ASCOT, and ACCOMPLISH studies). In contrast, there is good evidence of cardiovascular benefit for higher-dose thiazides and for the thiazide-like diuretics chlortalidone and indapamide.
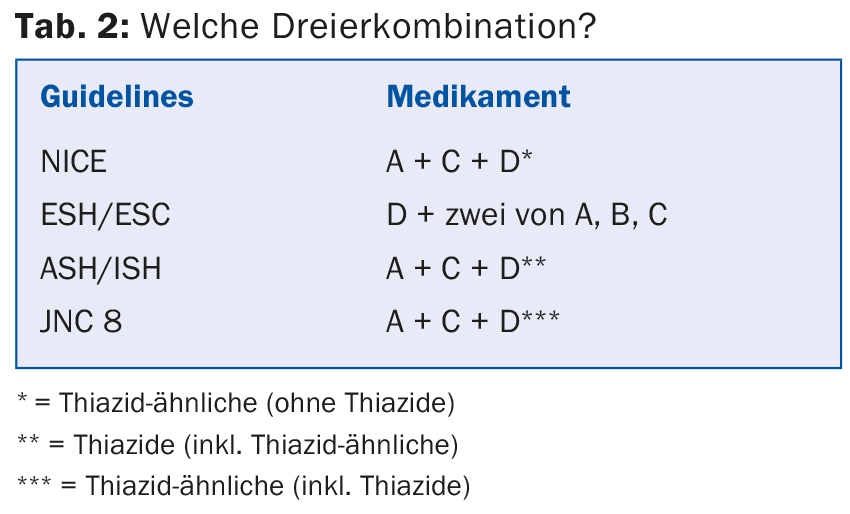
Which triple combination?
The guidelines give slightly different recommendations (Table 2) . It is clear that fixed-combination drugs are promising: they increase compliance and may also have a favorable effect on blood pressure control and side effects [7].
In any case, care should be taken to ensure a sufficiently long duration of action (especially with once-daily dosing) [8]. Regarding chronopharmacotherapy, patients with refractory hypertension may particularly benefit from taking antihypertensives in the evening. Finally, nocturnal blood pressure reduction is of particular importance for cardiovascular prognosis.
RAAS blockers: higher efficacy when taken in the evening due to increased activity of the RAAS in the early morning hours.
Calcium antagonists: enhanced reduction in nocturnal blood pressure, significantly less peripheral edema.
Beta-blockers: ideally given during the day (sympathetic nervous system especially active during the day, less relevant at night).
Diabetics taking more than one antihypertensive should be given one or more agents in the evening. This results in improved 24-hour blood pressure control and reduced cardiovascular morbidity as well as mortality [9].
Source: Medidays, August 31 to September 4, 2015, Zurich
Literature:
- Cannon CP, et al: Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med 2015 Jun 18; 372(25): 2387-2397.
- Robinson JG, et al: Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med 2015 Apr 16; 372(16): 1489-1499.
- Navarese EP, et al: Effects of Proprotein Convertase Subtilisin/Kexin Type 9 Antibodies in Adults With Hypercholesterolemia: A Systematic Review and Meta-analysis. Ann Intern Med 2015 Jul 7; 163(1): 40-51.
- Jamerson K, et al: Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008 Dec 4; 359(23): 2417-2428.
- van Vark LC, et al: Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of renin-angiotensin-aldosterone system inhibitors involving 158,998 patients. Eur Heart J 2012 Aug; 33(16): 2088-2097.
- Brugts JJ, et al: Impact of renin-angiotensin system inhibitors on mortality and major cardiovascular endpoints in hypertension: A number-needed-to-treat analysis. Int J Cardiol 2015 Feb 15; 181: 425-429.
- Gupta AK, Arshad S, Poulter NR: Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010 Feb; 55(2): 399-407.
- Flack JM, Nasser SA: Benefits of once-daily therapies in the treatment of hypertension. Vasc Health Risk Manag 2011; 7: 777-787.
- Hermida RC, et al: Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care 2011 Jun; 34(6): 1270-1276.
GP PRACTICE 2015; 10(11): 38-40











