Standard therapy for symptomatic patients with paroxysmal and persistent AF <is percutaneous endocardial catheter ablation for 1 year if medical treatment is unsuccessful. Initial experience in Switzerland with hybrid ablation, a combination of percutaneous endocardial and thoracoscopic epicardial radiofrequency ablation, now indicates that it is a feasible and safe treatment option. The current results from Inselspital are very promising, but still limited in their significance.
Percutaneous endocardial catheter ablation is the standard therapy for symptomatic patients with paroxysmal and persistent atrial fibrillation (AF) <1 year of unsuccessful medical therapy. But what can we offer to patients who have long-standing persistent symptomatic VCF? What are the options for patients who have received multiple, unsuccessful catheter ablations? Does surgery offer a possible answer?
The Cox-Maze operation, although highly effective (see previous report), was and is technically difficult and requires a heart-lung machine because the operation must be performed on an open, arrested heart. Thus, it is difficult to justify such a maximally invasive procedure for VCF. In order to be able to use the good results of the Cox-Maze operation in a further developed sensible therapy, minimally invasive approaches have recently been pushed. Nowadays, complete epicardial pulmonary vein isolation on the beating heart can be achieved by thoracoscopic procedures with low risk. However, the more minimally invasive we become, the more we lose the ability to perform all of the original fragmentations and lesions of the successful Cox-Maze operation, thus accepting that the efficiency of the intervention will decrease.
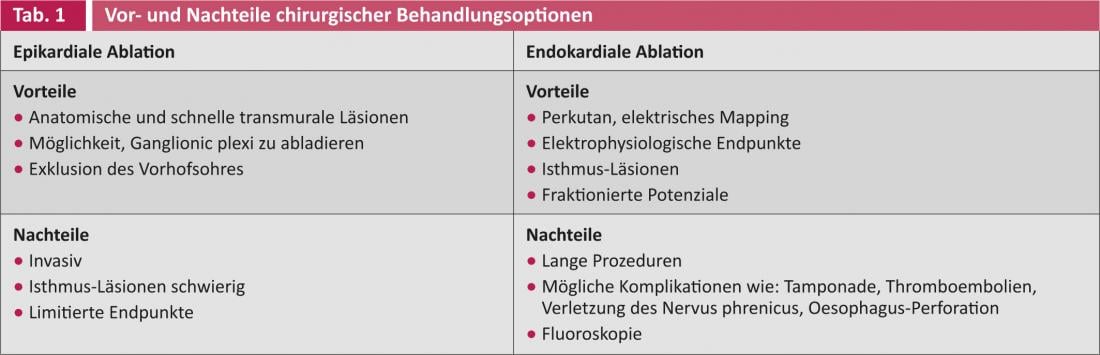
Thus, the consideration of combining both methods, surgical minimally invasive (epicardial) and catheter-based (endocardial), to potentiate the advantages of both methods while minimizing the disadvantages, suggests itself (Table 1).
Tailored treatment thanks to interdisciplinary collaboration
Under the premise of combining the two treatment options to obtain positive symbioses of the respective advantages and disadvantages, and with current knowledge and state-of-the-art electrophysiological mapping systems, it should be possible to design a tailored treatment for each patient by an interdisciplinary team. We were able to successfully establish this program throughout Switzerland for the first time in May 2010 at the Inselspital in Bern.
The goals of hybrid ablation of the VHF are:
- Success rates must be better than those of isolated endocardial or epicardial ablation with a lower complication rate.
- It is said to be faster to perform than isolated endocardial ablation.
- The chest must not be opened (i.e., completely endoscopic).
Consequently, it is an intervention that can be performed in the electrophysiology laboratory(Fig. 1). The condition is a GMP class A laboratory.
Fig. 1: Setting in the electrophysiology laboratory during epicardial ablation.
Intervention
The patient is under general anesthesia with double lumen intubation. The positioning of the patient is shown in Figure 2: Three intercostal throcars are inserted right thoracically to allow insertion of the optic and two instruments (Fig. 2 b).
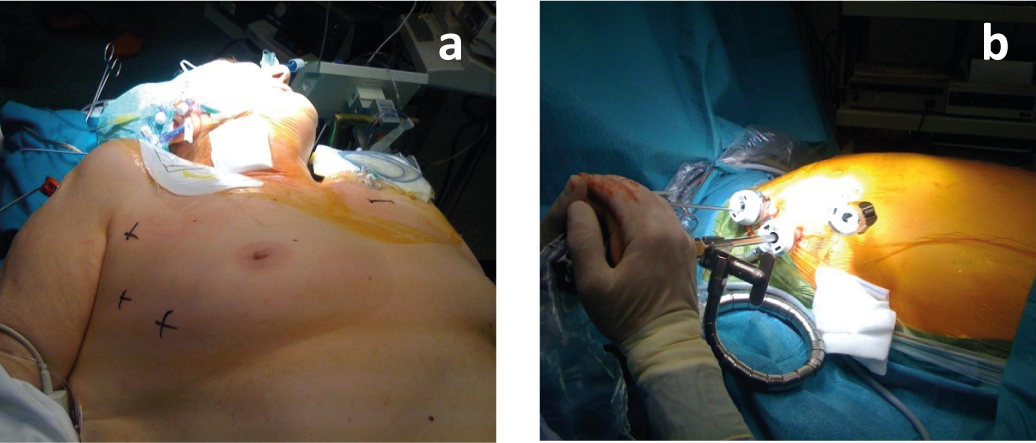
Fig. 2: a) Positioning of the patient during double lumen intubation;
b) Insertion of three right thoracic intercostal throcaries to allow insertion of the optic and two instruments.
The pericardium is then opened under direct vision by video endoscopy and a uni- or bipolar electrode is placed on the beating heart to perform the so-called box lesion by radiofrequency ablation to isolate all pulmonary veins (Fig. 3).
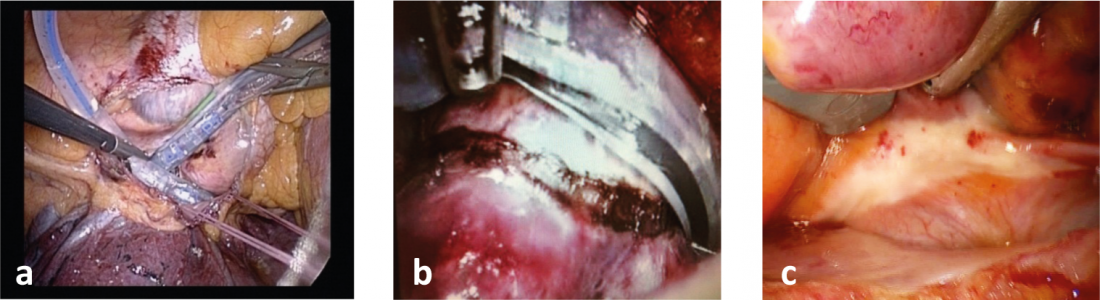
Fig. 3: a) Intraoperative image of epicardial ablation catheter placement; b) Intraoperative image of fresh ablation lesion;c) The ablation scar a few months postoperatively.
After subsequent heparin administration, the electrophysiologist takes over the intervention and after insertion of the catheter electrodes through the groin into the left atrium, the electrical isolation of the surgical ablation is verified. If necessary, electrical gaps are completed by catheterization(Fig. 4).
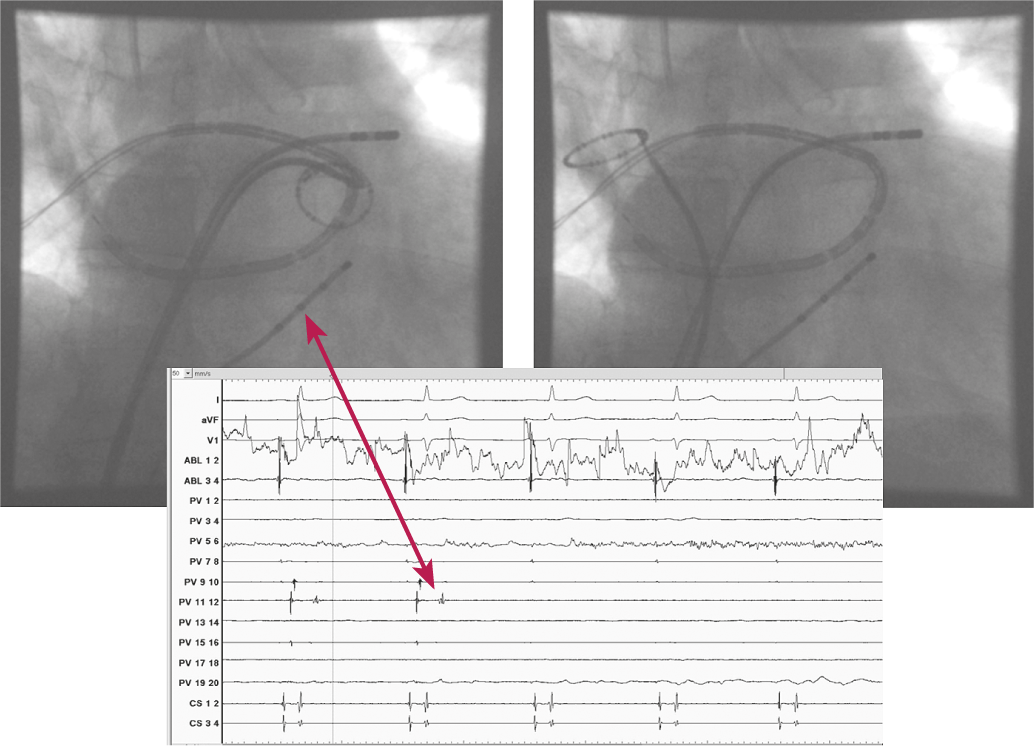
Fig. 4: Insertion of the catheter electrodes through the left groin into the left atrium.
We have so far treated seven patients (average age 51 years) with this method at the Inselspital in Bern. Table 2 shows the preoperative characteristics. To date, patients with long-standing persistent VCF who have failed to respond to medical and catheter therapy have been the primary candidates.
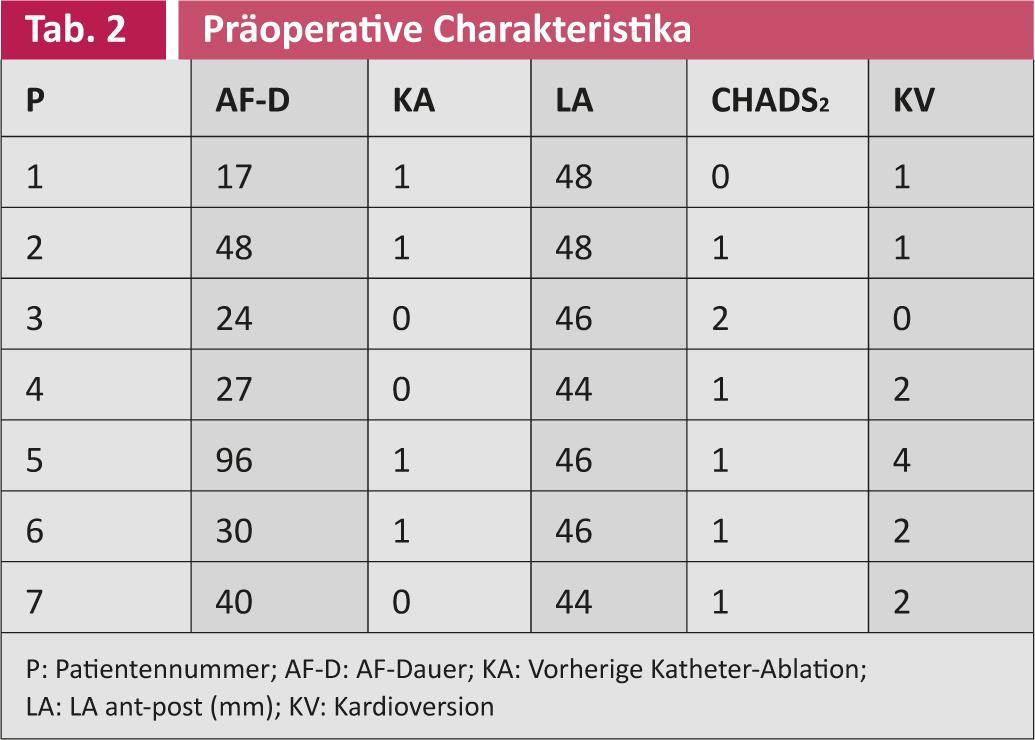
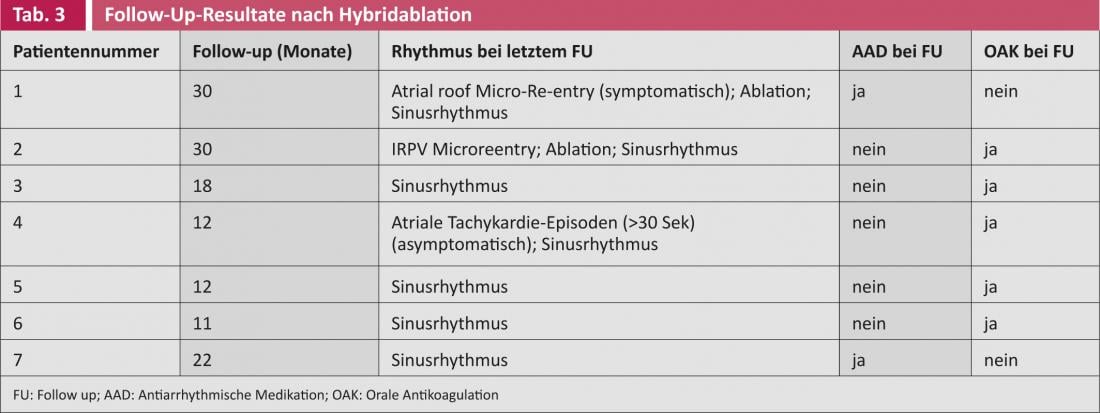
There were no intraprocedural complications. All patients were extubated immediately after the intervention. The median operative time was 240 minutes (120-395 minutes). The total average radiation exposure was 19.4 minutes (11.4-59.6 minutes). No patient received foreign blood products, and the average length of hospital stay was six days. Follow-up results are shown in Table 3. All patients are in sinus rhythm. Two patients required additional catheter ablation after two years because of localized atrial arrhythmia, but not because of VHFs.
Conclusion
- Combined thoracoscopic epicardial and catheter endocardial atrial ablation in patients with long-standing persistent VHF is feasible and safe.
- This procedure requires close collaboration between anesthesiology, electrophysiology, and cardiac surgery.
- Current experience is promising but limited.
The exchange between electrophysiologists/cardiologists and cardiac surgeons, as well as their combined efforts in the treatment of VCF, promotes the understanding of this pathology and its therapeutic options, thus contributing to the successful treatment of patients.
PD Alberto Weber, MD