Primary Consultation: The 42-year-old patient presented to our clinic on an emergency basis in early February 2016 for progressive gait unsteadiness, slowing, cognitive impairment, and nocturnal incontinence. There were no previous medical history, especially no immunosuppressive diseases. Clinically, there was a markedly slowed, somnolent patient with broad-based, unsteady gait without focal neurologic deficit in a cachectic nutritional state.
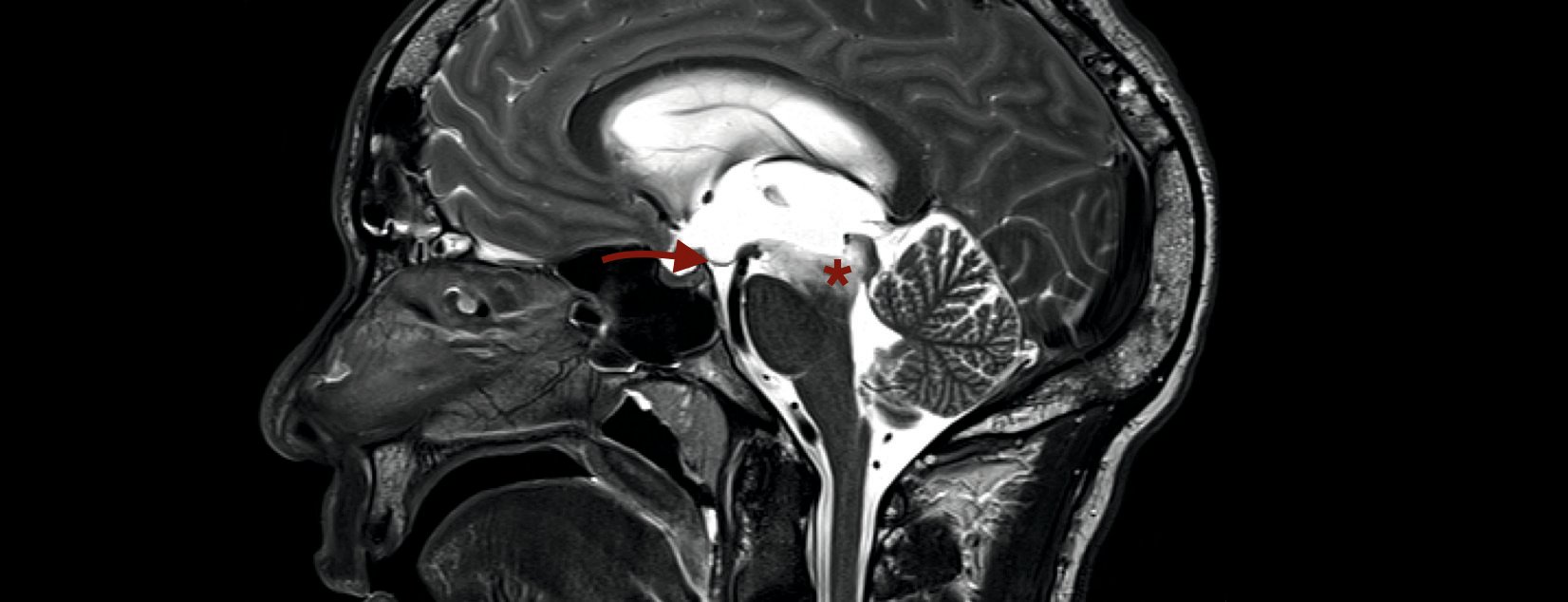
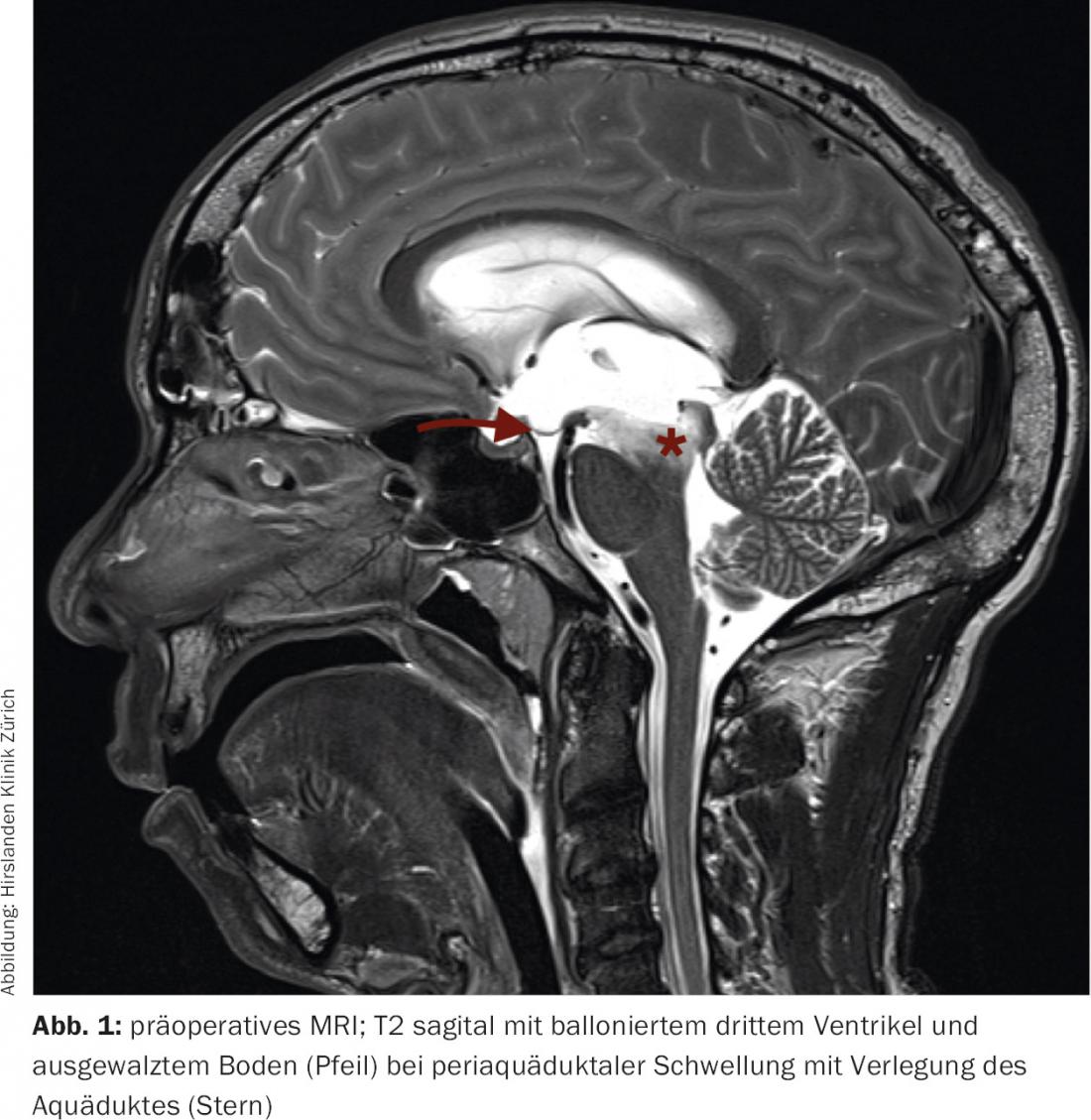
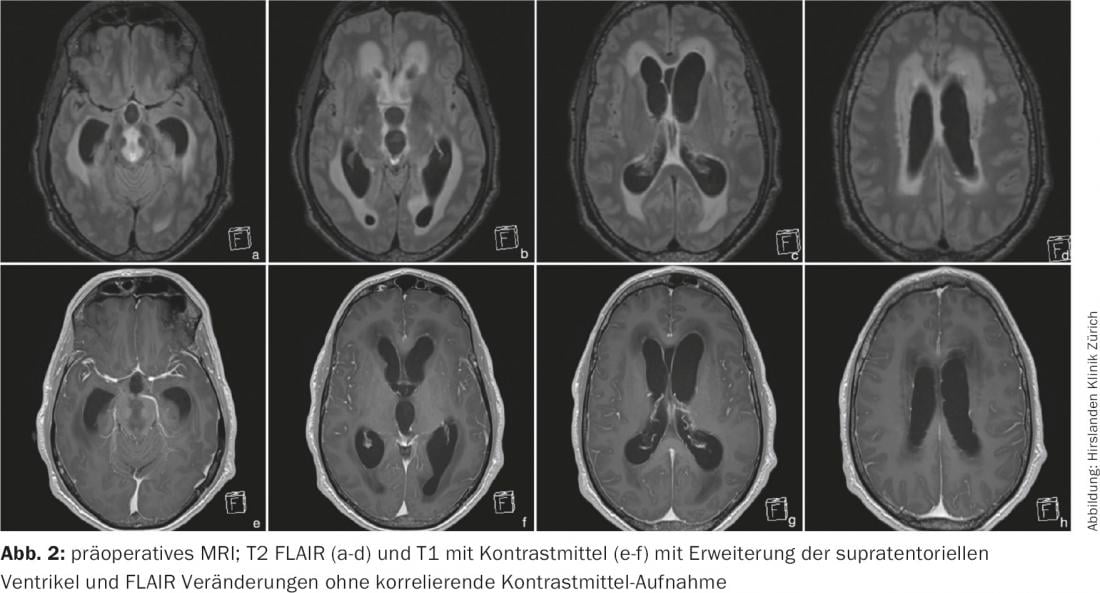
Magnetic resonance imaging of the skull revealed a massive widening of the supratentorial CSF spaces in the sense of triventricular hydrocephalus occlusus (Fig. 1) . The CSF was protein-rich according to MR criteria. Periventricularly and in the brainstem, diffuse FLAIR-hyperintense and T1-hypointense changes were seen without contrast uptake (Fig. 2). In cases of triventricular hydrocephalus of unclear etiology and periaqueductal changes, the indication for endoscopic ventriculostomy with simultaneous specimen biopsy was given.
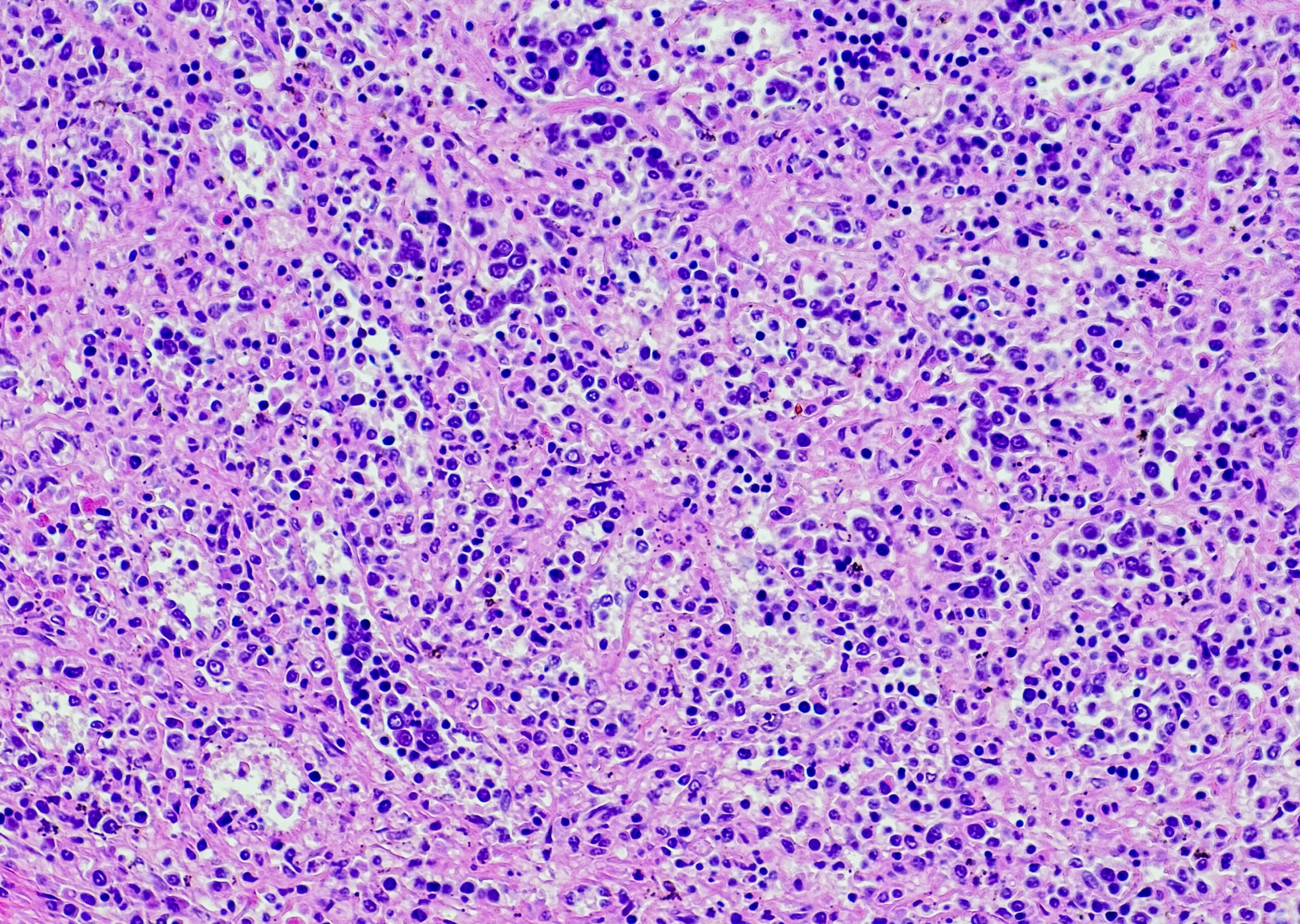
Inpatient treatment: endoscopic third ventriculostomy was performed without complications. Here, the floor of the third ventricle is perforated in front of the copora mammilaria to achieve CSF circulation into the basal cisterns bypassing the aqueduct. Intraoperatively, there was a diffuse change in the ependyma (Fig. 3) . Samples were taken for histopathological examination and cerebrospinal fluid for micriobiological processing. Postoperatively, the decrease in vigilance and gait unsteadiness were rapidly regressed, and no new neurological deficits occurred. On the seventh postoperative day, the patient could be discharged home in a significantly improved general condition.
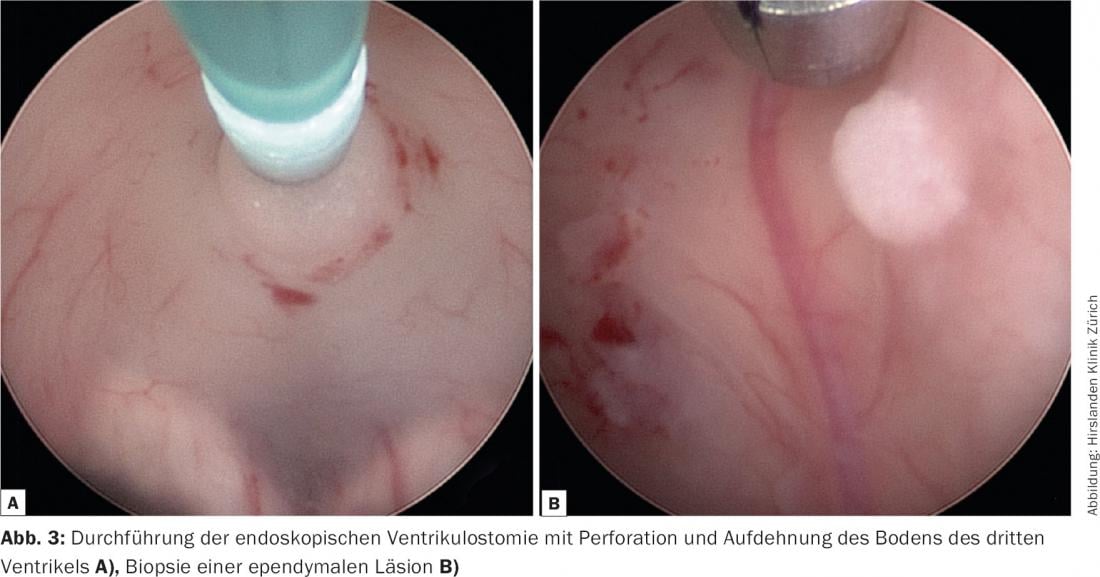
Definitive histology of ependymal, periventricular, and cortical biopsies was able to exclude tumor. There were only nonspecific changes with reactively altered brain tissue and marginal CD8-positive T and plasma cells. Fungi, acid-fast rods, toxoplasma, CMV or SV40 could not be detected. Analysis of the CSF also failed to detect infection or malignant cells. The cell count (29/μl, norm: <3) and lactate (3.2 mmol/l, norm: 1.1-2.4) were slightly elevated, with otherwise normal CSF findings. The preoperative HIV test was positive.
Follow-up: After receiving resistance testing, antiretroviral therapy with Atripla was started in early March 2016. The therapy is well tolerated by the patient.
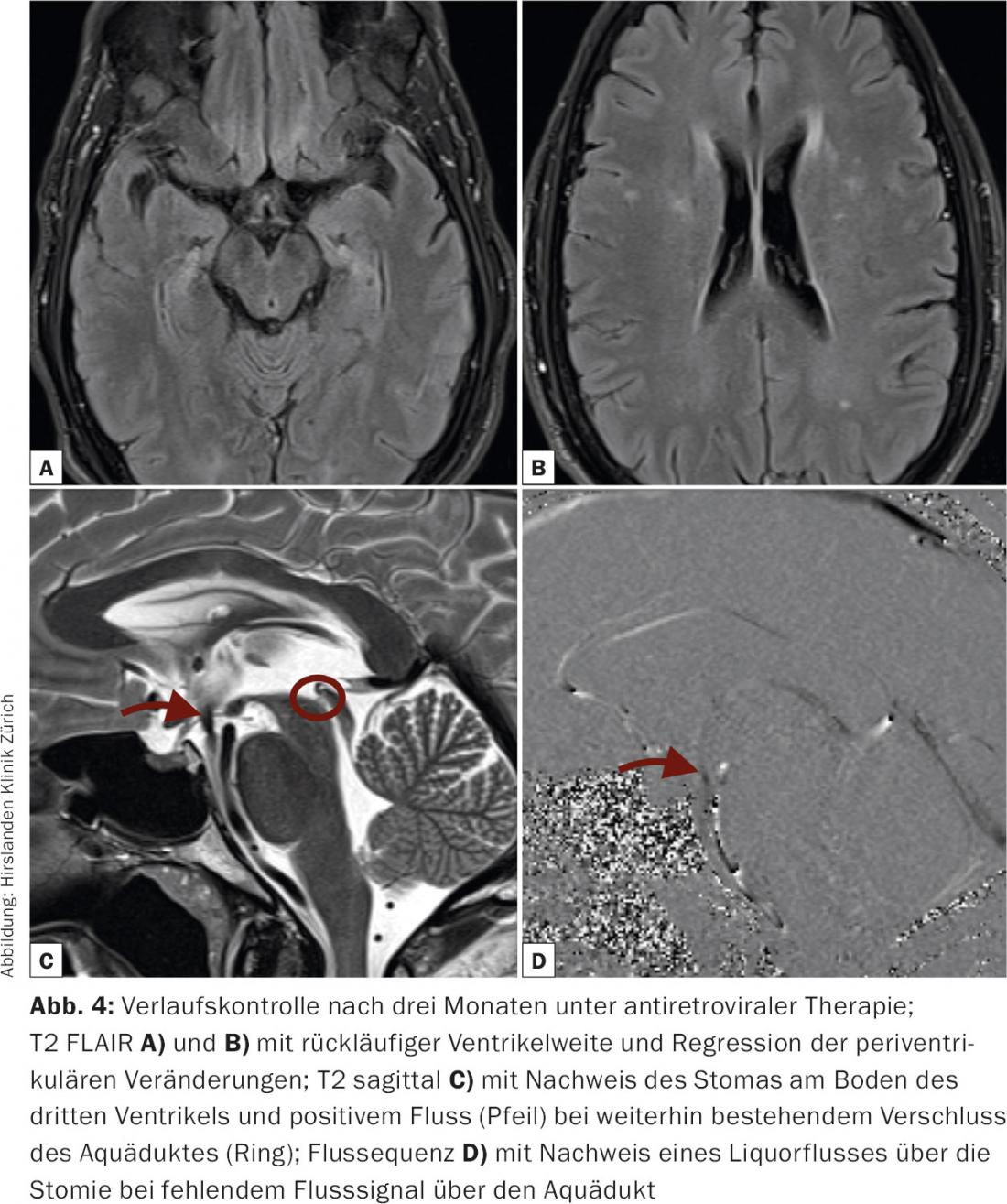
At clinical and imaging follow-up three months after surgery, the patient is awake, fully oriented, and without focal neurologic deficit. Subjectively, the memory impairment was also regressive.
MRI follow-up shows a normally wide ventricular system. The periventricular changes have completely regressed. There are also no more abnormalities in the brainstem, periaqueductally. Only in the aqueduct itself is there evidence of bonding. The stoma at the base of the third ventricle is open with a strong flow signal (Fig. 4).
Discussion: Cerebral changes in HIV-positive patients are common, especially due to opportunistic infections. However, it has been shown that primary HIV infection is also associated with CNS infiltration [1–3].
Before the introduction of effective antiretroviral therapy, brain atrophy with hydrocephalus evacuo was observed in advanced disease [4]. After opportunistic infections, especially after meningitis caused by toxoplasmosis or cryptococci, hydrocephalus malresorptivus is possible. Occlusive hydrocephalus is less common, but may also occur in the setting of localized space-occupying lesions (lymphoma, tuberculoma, etc.) [2,5]. However, occlusive hydrocephalus without concomitant opportunistic infection is extremely uncommon.
Acute hydrocephalus occlusus, regardless of etiology, is a life-threatening condition that should be treated as soon as possible by a neurosurgical team.
In acute vigilance reduction, relief by external ventricular drainage is possible. However, endoscopic third ventriculostomy offers a durable solution to treat CSF circulatory dysfunction, especially if, as in this case, the aqueduct remains closed at a later time. In addition, there is the possibility of histological confirmation of unclear intracerebral changes. Histological confirmation is obligatory, especially in the case of concomitant HIV infection, since the many concomitant diseases cannot be reliably diagnosed by imaging alone [2]. CSF examinations are also often inadequately informative, as the CSF may be sterile with only nonspecific changes during immunosuppression [2].
Shunt placement is also a treatment option for hydrocephalus, but primarily only in cases of malresorptive etiology. Histological confirmation of conspicuous lesions is not possible. In addition, postinfectious or tumor disease presents the possibility of dissemination and an increased risk of shunt occlusion.
Although in this case the histologic findings are rather nonspecific for HIV encephalopathy, the imaging findings with the corresponding FLAIR changes can often be seen with HIV involvement of the CNS. In particular, the regression of changes in follow-up under antiretroviral therapy in this case argue for primary CNS involvement by the underlying disease.
Literature:
- Zayyad, Z., & Spudich, S. (2015). Neuropathogenesis of HIV: from initial neuroinvasion to HIV-associated neurocognitive disorder (HAND). Curr HIV/AIDS Rep, 12(1), 16-24, doi:10.1007/s11904-014-0255-3.
- Henderson, D., Sims-Williams, H. P., Wilhelm, T., Sims-Williams, H., Bhagani, S., & Thorne, L. (2016). Neurosurgery and human immunodeficiency virus in the era of combination antiretroviral therapy: a review. J Neurosurg, 1-11, doi:10.3171/2016.1.JNS151194.
- Bhigjee, A. I., Naidoo, K., Patel, V. B., & Govender, D. (1999). Intracranial mass lesions in HIV-positive patients–the KwaZulu/Natal experience. Neuroscience AIDS Research Group. S Afr Med J, 89(12), 1284-1288.
- Thompson, P. M., & Jahanshad, N. (2015). Novel Neuroimaging Methods to Understand How HIV Affects the Brain. Curr HIV/AIDS Rep, 12(2), 289-298, doi:10.1007/s11904-015-0268-6.
- Basavaprabhu, A., Soundarya, M., Deepak, M., & Satish, R. (2012). CNS toxoplasmosis presenting with obstructive hydrocephalus in patients of retroviral disease – a case series. Med J Malaysia, 67(2), 214-216.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(4): 34-36.