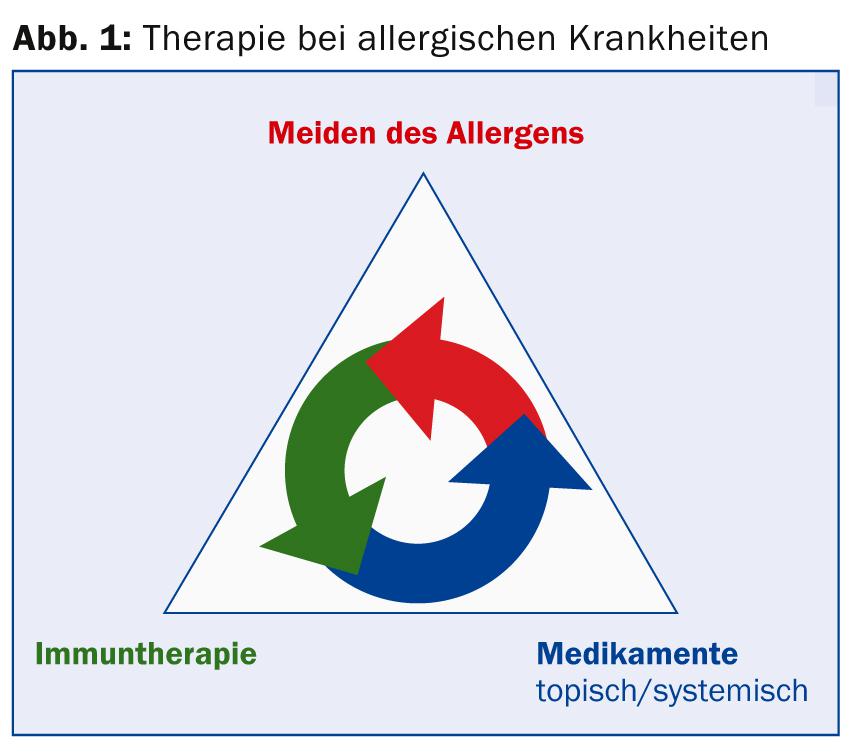
The therapy concept for allergic diseases is based on three principles: Allergen abstinence or elimination is optimal, but it is time-consuming and in individual cases can be expensive. Pharmacotherapy is symptomatic and can be used in combination. Finally, immunotherapy is a causal, relatively expensive approach that is carried out over three to five years and whose efficacy has been demonstrated several times in large controlled trials. The latter was the topic at the 3rd DermAcademy in Basel. Furthermore, nutritional aspects of acne were discussed.
(ag) According to Prof. Dr. med. Andreas J. Bircher, Senior Physician Allergology, University Hospital Basel, specific immunotherapy (SIT) is a kind of “allergy vaccination” that can be applied either subcutaneously (SCIT), sublingually (SLIT), or experimentally intranodally or topically-epidermally. It is one of the three pillars in the therapeutic concept for allergic diseases (Fig. 1).
What are the major allergens in pollen?
In the field of polysensitization, cross-sensitization can be distinguished from co-sensitization. Bet v1 is a major allergen for co-sensitizations (PR 10 proteins), whereas Bet v2 is for cross-sensitizations (profilins).
The requirements for immunotherapy are:
- ubiquitous, non-preventable allergens
- clear evidence of sensitization
- Evidence of clinical relevance.
Suitable allergens for high-dose extracts with main allergens are in the case of pollen grasses rye, birch, alder, hazel, ash, beech, oak, mugwort, plantain as well as ragweed, in the case of mites D. pteronyssinus and D. farinae, in the case of animal epithelia the cat as well as in the case of hymenoptera venoms the bee and wasp venom.
Regarding extracts and composition, a maximum of two to three different allergen extracts and a mixture of only cross-reactive, not different seasonal or perennial allergens should be used. Also to be avoided are mixtures of mites and animal hair/molds as well as pollen and molds (enzymatic degradation). One should aim for a high content of major allergens and administer several extracts separately into each upper arm.
When can immunotherapy be used?
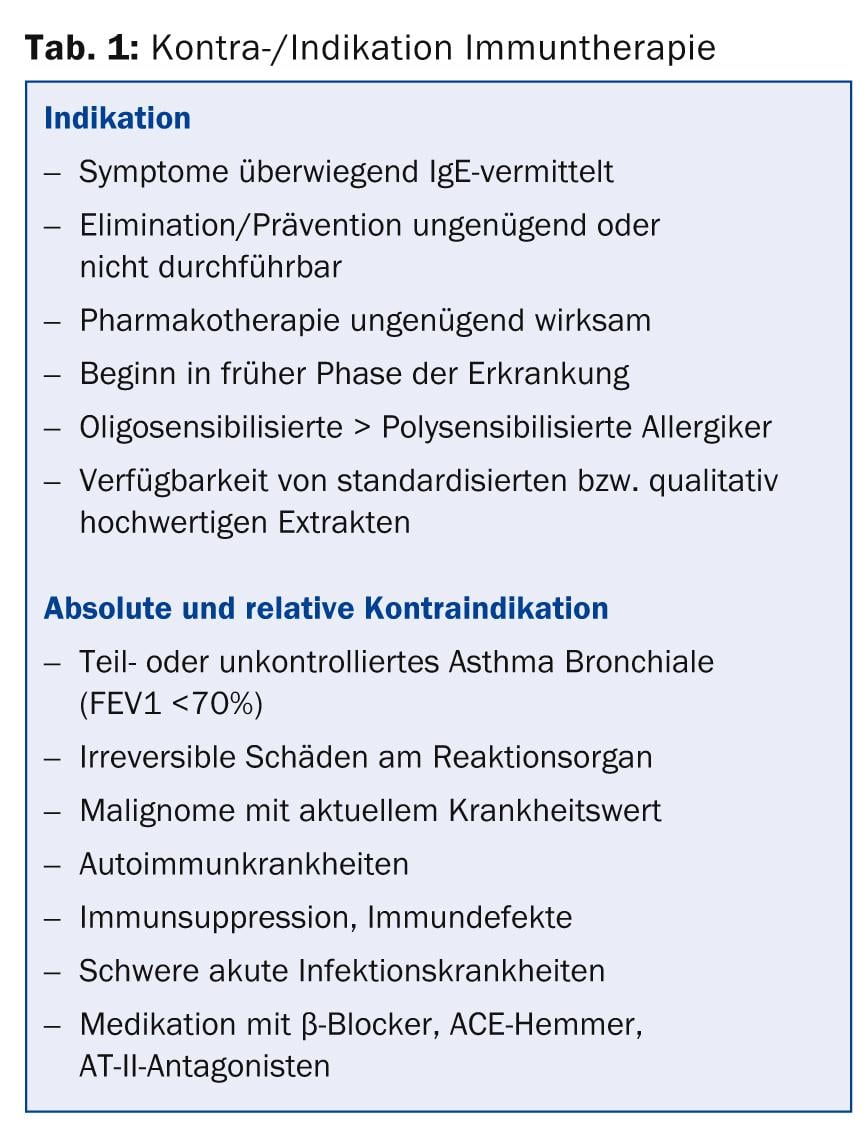
For the success of the subcutaneous form, it is crucial that the pollen allergy is dominant and that there is a narrow allergen spectrum and a short duration of disease. Also predictors of success are reversible lower airway involvement, young age, and year-round treatment. “The indication (Tab. 1) should be established by a trained physician or a specialist in the field of allergology. The relevant allergens must be documented and the allergen extracts selected (allergen composition),” advises Prof. Bircher.
The choice of method is crucial: Which application method should be used (subcutaneous, sublingual)? Do you follow preseasonal, cosaisonal, or perennial schedules? Do you choose slow, cluster or fast procedures (Ultrarush for bee and wasp venom allergy)?
Phases and schemes
The initiation phase lasts a few weeks to months, and the maintenance phase lasts three to five years. SCIT can be performed using the following schemes:
- Pre-seasonal: Short (6-8 injections) or long (12-18 injections).
- Perennial constant: initiation (12-18 injections), maintenance (1×/month).
- Perennial reduced: Maintenance (1×/month), Co-seasonal dose reduction (frequently recommended according to Prof. Bircher).
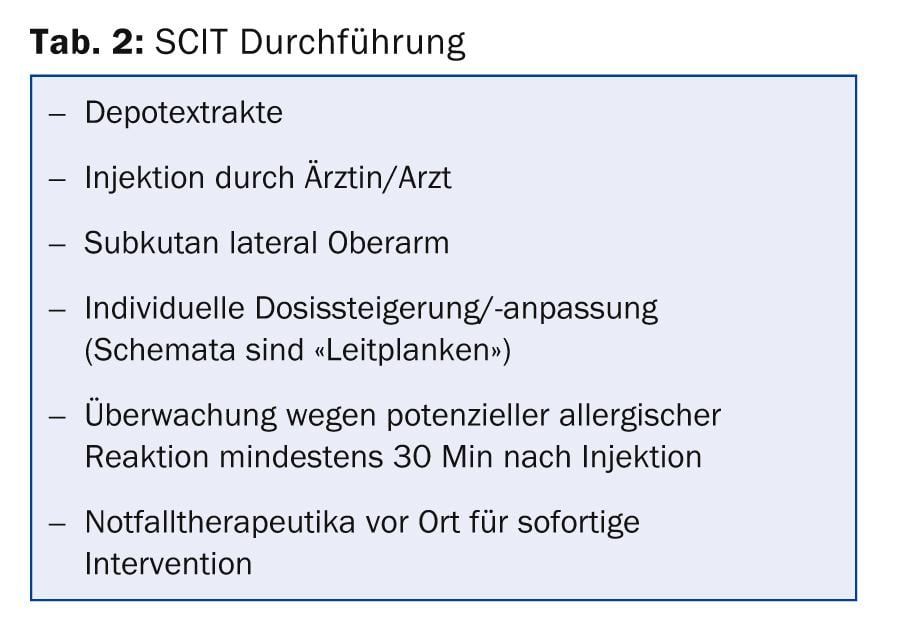
“In any case, one must always ask the patient about allergic and general symptoms or the tolerance of the last injection. Also important: Are new medications being taken, did vaccinations take place? There should be at least one week between an SCIT injection and a live vaccination that can be scheduled. Immediately necessary vaccinations can be given at any time, and SCIT can be continued according to the specialist information or after two weeks with the last administered dose. Augmentation factors such as alcohol, physical exertion, intensive sports, sauna, etc. should be avoided shortly before the injection and for the rest of the day,” explained Prof. Bircher regarding the implementation of SCIT (Tab. 2). “For infections, remember the following: Do not desensitize during the acute phase of the infection. If this results in a longer interval, the dose should be adjusted if necessary. In addition, in the case of infection exacerbation of bronchial asthma, it is imperative to strive for rapid stabilization before resuming desensitization.” Pregnancy is a contraindication to initiation of immunotherapy.
Special features of SLIT
SLIT must always be paused in the case of febrile infections, especially in the respiratory tract (asthma), and interrupted in the case of acute injuries or inflammations in the mouth/throat, major surgical interventions in the oral cavity, acute gastroenteritis, an asthma exacerbation and vaccinations. If two extracts are used, the application should take place at different times of the day.
Nutritional aspects of acne
“The Paleolithic, and with it the savage lifestyle, ended about 20,000 to 12,000 years ago. During this time, neither dairy nor cereal products were consumed, and basal insulin levels were about 50% lower. The Neolithic period then saw a complete transition from a hunter-gatherer culture to sedentary farmers with animal domestication and cultivation. This is where today’s Western dietary style originated. It is characterized by the high consumption of sugar, hyperinsulinotropic cereal flour products, milk and dairy products,” explained PD Dr. med. Peter Häusermann, Dermatology University Hospital Basel. “Recent studies confirm the correlation of acne with increased BMI as well as insulin resistance.”
Crucial for this is the food- and growth factor-sensitive kinase mTORC1: At high glycemic load and consumption of milk protein, mTORC1 is increasingly activated. Studies have been able to confirm this association and a lower incidence of acne when glycemic load and dairy consumption are reduced [1,2]. “The Western diet, with its high glycemic load plus dairy protein, increases insulin/IGF-1 signal transduction and thus exaggerates puberty-related IGF-1 signaling of mTORC1 activation,” Dr. Häusermann concluded.
Paleolithic diet
In conclusion, acne is a disease of civilization that is at least partly determined by diet and shows an association with BMI, obesity, insulin resistance, increased risk of diabetes and prostate cancer.
A paleolithic emphasized diet can therefore be useful for acne: Carbohydrates with a high glycemic index (GI) and high glycemic load, sweets, sugary soft drinks, white bread, whole milk chocolate, yogurt, milk of all fat levels, etc. should be reduced. Low GI and low glycemic load carbohydrates, whole grain bread, vegetables, salads, fruits, bitter chocolate and fish are recommended, for example. “Placebo-controlled studies demonstrate the effectiveness of a Paleolithic acne diet,” Dr. Häusermann concluded.
Certain special forms of acne (steroid acne, chloracne and acne cosmetica), on the other hand, have no nutritional connection, yet they cannot be distinguished in clinical appearance from classic acne.
Source: 3rd DermAcademy 2014, February 13, 2014, Basel
Literature:
- Smith RN, et al: A low-glycemic-load diet improves symptoms in acne vulgaris patients: a randomized controlled trial. Am J Clin Nutr 2007; 86 (1): 107-115.
- Di Landro A, et al: Family history, body mass index, selected dietary factors, menstrual history, and risk of moderate to severe acne in adolescents and young adults. J Am Acad Dermatol 2012 Dec; 67(6): 1129-1135. doi: 10.1016/j.jaad.2012.02.018. Epub 2012 Mar 3.
DERMATOLOGIE PRAXIS 2014; 24(3): 49-51











