Frequently, chronic contact dermatitis is a combination of irritant and contact allergic eczema. The selection of the test allergens is anamnesis-guided. In addition to nickel – still the most common trigger of contact allergy – contact sensitization often occurs to rubber ingredients, textile dyes and epoxy resins, but also to some of the preservatives contained in cosmetics. Sensitizations to para-phenylenediamine are also frequently encountered, and the trend with regard to acrylate sensitizations has been upward for several years.
Last year, an updated S1 guideline on contact dermatitis was published – reason enough to revisit contact dermatitis, its assessment and current contact allergens. Contact allergic eczema is common with a prevalence of up to 20%. Women are affected more frequently than men. In particular, irritant contact eczema must be differentiated, but there are a number of other differential diagnoses (overview 1) . Chronic contact eczema is often a combination of irritant and contact allergic eczema, especially on the hands. In the case of eczema manifestations, the pattern recognition and thus the noxious agent that could be the trigger can be difficult to recognize, since the allergen can be transmitted aerogenically or from the partner, or dislocated only leads to the eczema (e.g. is transmitted from the hands to the eyelids).
Allergenic substances: Medical history and frequency trends
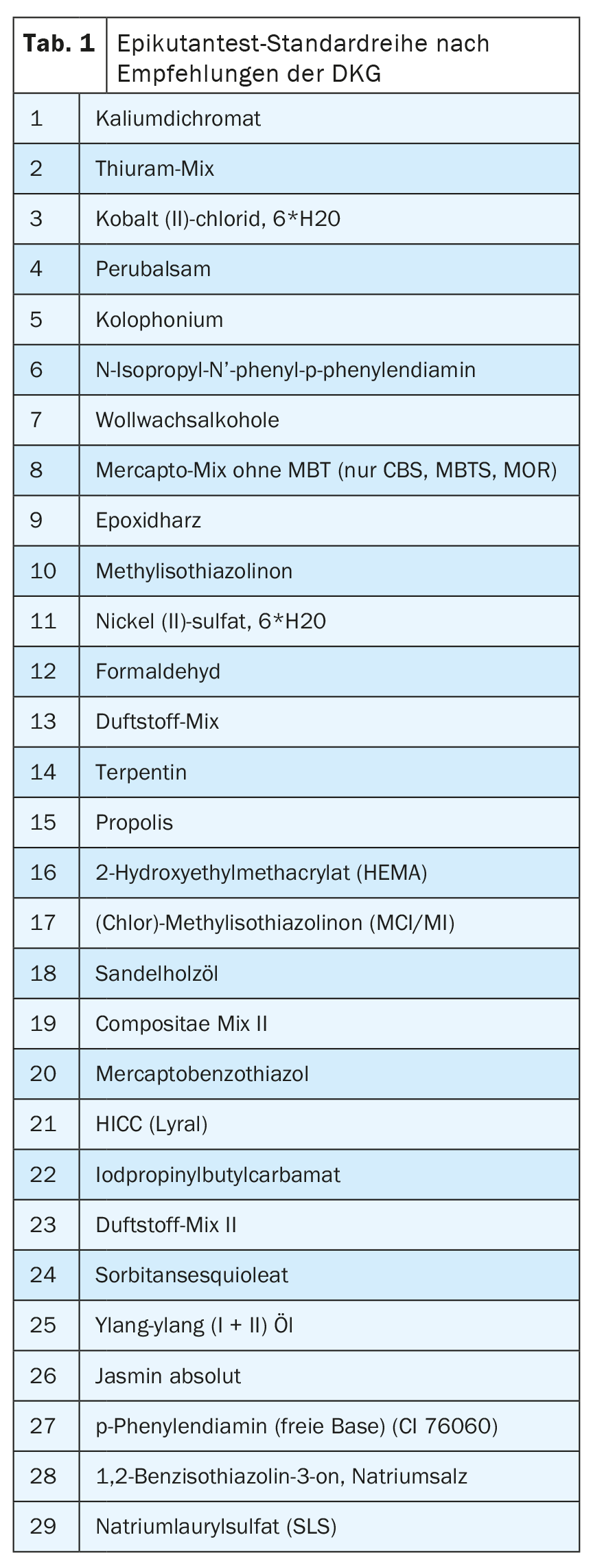
The selection of allergens to be tested should be guided by the medical history. Irrespective of this, testing of the standard series (Tab. 1) can frequently detect sensitization even in the case of an inconspicuous medical history. Patients must be informed in advance about possible risks. Thus, the epicutaneous test may cause irritative but also longer-lasting eczematous skin reactions. Pigmentary shifts on the test area are another risk. Rarely, a flare-up of the original eczema or active sensitization may result from the test.
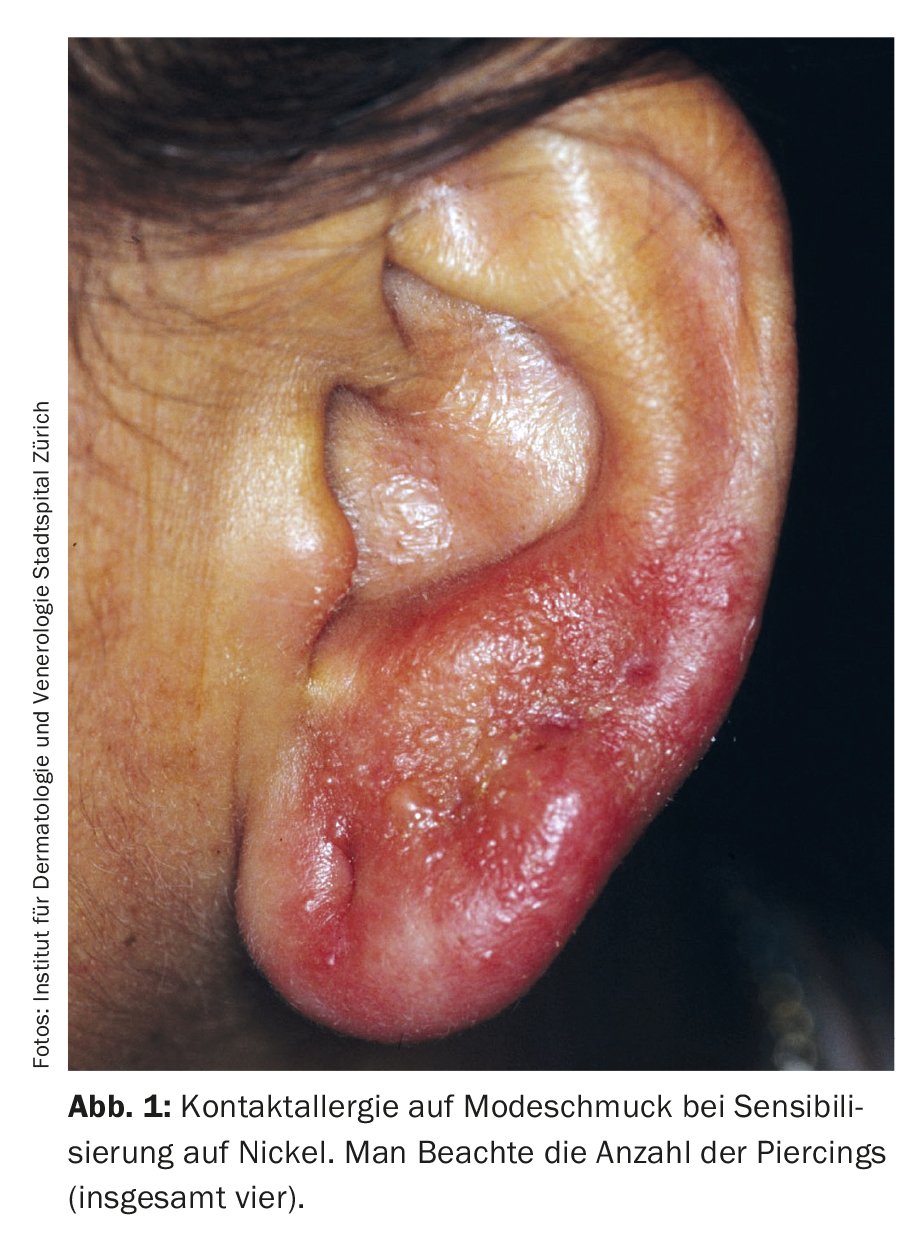
Nickel, cobalt: The allergen “hit list” is still headed by nickel, although a decrease in sensitization can be observed. However, the nickel content in jewelry and piercing materials still occasionally exceeds the limits permitted by the EU directive, so that sensitization continues to occur, especially in younger patients. (Fig. 1). Also razors and somewhat less obvious also computer mice, laptops and mobile phones can represent nickel sources, which have to be anamnesed depending on the localization of the eczema.
Cobalt sensitization is also common and usually associated with nickel sensitization. However, in addition to such coupling allergy to metal salts from jewelry, cobalt can also be observed as an isolated allergen. The allergen sources can be colors and leather.
Fragrances: Increasing causes of contact allergy to fragrances include terpene hydroperoxides such as limonene, linalool, and occasionally geraniol.
(Chlor)-Methylisothiazolinone: The preservative (chlor)-methylisothiazolinone(MI) has been increasingly used in cosmetics, personal care and household products since the 1980s and has led to a veritable epidemic of contact sensitization. An amendment to Annex V of the EU Cosmetics V. 2018 banned the use of MI in cosmetic leave-on products and limited it in rinse-off products to a concentration that is no longer sufficient for a preservative effect, so that use in this respect in products is no longer useful. MI can also be observed as an occupational toxin (Fig. 2) and then mainly affects cosmeticians and painters.
Epoxy resin: Epoxy resin sensitization is also of occupational relevance and is most common in the construction industry. Allergies can occur not only to the resins themselves, but also in isolation to the thinners and hardeners required, so these should always be tested as well if they are suspected.
Rubber ingredients: Contact sensitization to rubber ingredients is also frequently found. Among these, thiuram sensitizations are most common, followed by dithiocarbamate and mercaptobenzothiazole. These allergies can be particularly problematic with protective gloves, even if they are latex-free.
Textile dyes: show sensitization frequencies of >1%, so that epicutaneous testing of these dyes should be considered in cases of persistent or chronically recurrent eczema of unclear etiology, especially on the trunk. Affected patients should avoid synthetic textiles, as these are more frequently treated with correspondingly allergenic (azo) dyes than textiles made from natural fibers.
para-Phenylenediamine: Sensitization to para-phenylenediamine by so-called “black henna” tattoos is an unbroken trend (Fig. 3) in vacation acquired contact sensitization. This sensitization makes subsequent darkening of the hair (e.g. with dyes containing toluylenediamine) and employment in the hairdressing profession impossible. The supposedly harmless, because only painted on “temporary tattoos”, which are offered on vacation beaches, but occasionally also in hotels or at hairdressers, should be absolutely avoided.
Acrylate sensitizations: are increasing as a consequence of the use of appropriate nail polish products and of acrylate adhesives for fixing glucose measurement systems and insulin pumps.
Recommendations for epicutaneous testing
The testing itself should be performed only after the acute eczema has healed. The test sites are the back or the thighs. The test area should not be exposed to UV for four weeks prior to application of the test. levels, local corticosteroids should be discontinued seven days prior to testing in the test area. Systemic corticosteroids and H1 antihistamines should also have been discontinued five days prior to testing. The test should be pasted for 48 hours with reading after 48 and 72 hours. This test protocol yields a higher sensitivity. A reading as early as 24 hours, on the other hand, can increase specificity. A later reading may be useful for certain allergens (corticosteroids, formaldehyde, formaldehyde/resins, p-phenylenediamine, metals) to record positive reactions.
Positive reactions are characterized by papules and infiltrate. If these are not clearly visible, palpation or even the tangential light of a flashlight can be helpful. Allergic reactions are characterized by dispersion and a crescendo of reaction; irritant reactions tend to be sharply circumscribed and atrophic. Finally, the results must be evaluated in conjunction with the medical history with regard to their clinical relevance. For documentation purposes, the patient is given a written document (allergy passport) listing the substances tested positive and their possible occurrence.
Take-Home Messages
- Irritant and allergic contact dermatitis may occur following acute, repetitive or chronic damage to the epidermal barrier by irritants.
- The diagnosis of allergic contact dermatitis is made by detecting contact sensitization to the causative allergens in the epicutaneous test.
- The selection of test allergens should be guided by the medical history. Important allergens are nickel, cobalt, rubber ingredients, textile dyes and epoxy resins. In addition, the preservative (chloro)methylisothiazolinone (MI), which is increasingly found in cosmetics, has led to a veritable epidemic of contact sensitization.
- Sensitization to para-phenylenediamine by so-called “black henna” tattoos also occurs repeatedly, and acrylate sensitization is steadily increasing as a consequence of the use of corresponding industrial products.
Further reading:
- Dickel H, et al: S1 guideline contact dermatitis. J Dtsch Dermatol Ges 2022; 20: 711-734.
- Alinaghi F, et al: Prevalence of contact allergy in the general population: A systematic review and meta-analysis. Contact Dermatitis 2019; 80: 77-85.
- Johansen JD, Werfel T: Highlights in allergic contact dermatitis 2018/2019. Curr Opin Allergy Clin Immunol 2019; 19: 334-340.
- Kreft B, Geier J: Perennial preservative allergy: what goes, what comes, what stays? Dermatologist 2020; 71: 190-196.
- Skudlik C, Geier J, John SM: Current trends in occupational dermatology. Dermatologist 2014; 65: 983-995.
- Richardson C, et al: Mobile Phone Dermatitis in Children and Adults: A Review of the literature. Pediatric Allergy, Immunology and Pulmonology 2014; 27: 60-68.
- Läuchli S, Lautenschlager S: Contact dermatitis after temporary henna tattoos – an increasing phenomenon. Swiss Med Wkly 2001; 131: 199-202.
- Kind F, Scherer K, Bircher AJ: Contact dermatitis to para-phenylenediamine in hair dye following sensitization to black henna tattoos – an ongoing problem. JDDG 2012; 10: 572-578.
- Wagner N, Kamann S, Oppel E: Contact allergy to glucose monitoring systems and insulin pumps. Dermatologist 2020; 71: 205-210.
- Uter W, et al: Contact Allergy-Emerging. Allergens and Public Health Impact. Int J Environ Res Public Health 2020; 17: 2404.
- Oppel E, et al: Contact allergy to the Dexcom G6 glucose monitoring system-Role of 2,2′-methylenebis(6-tert-butyl-4-methylphenol) monoacrylate in the new adhesive. Contact Dermatitis 2022; 87: 258-264.
DERMATOLOGIE PRAXIS 2023; 33(3): 5-7