Late-type allergies to medications can take a variety of forms, from mild exanthema to life-threatening reactions. Diagnosis is usually difficult and is based on history, skin testing and the classic lymphocyte transformation test (LTT). The cyto-LTT is based on the measurement of a combination of cytokines in cell culture supernatants and has replaced the classical LTT in routine diagnostics due to its higher sensitivity.
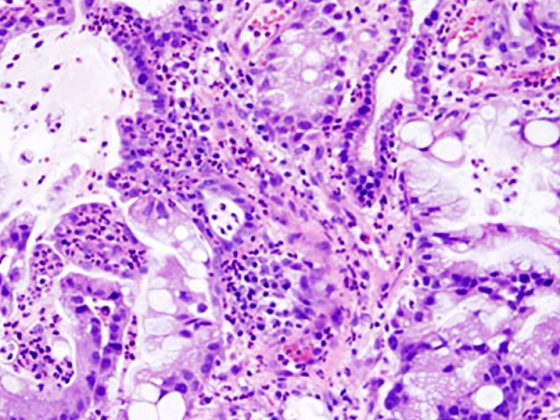
Drug allergies most often manifest on the skin, but in more severe forms, the liver, kidney, lungs, and even the heart muscle are also involved. Leading symptoms are exanthema occurring as maculopapular exanthema (MPE), acute generalized exanthematous pustulosis (AGEP), bullous reaction (Stevens-Johnson syndrome, SJS, and toxic epidermal necrolysis, TEN), and Drug Reaction with Eosinphilia and Systemic Symptoms (DRESS). These are T-cell responses to a drug. They usually appear only after days of treatment. Affected patients do not exhibit IgE antibodies against the drug, so that corresponding serological tests remain negative. After initial contact with sensitization, few T cells persist as memory cells, also called T memory lymphocytes, majority in spleen and lymph nodes. Few of these memory cells also circulate in the blood. Despite the low numbers, sufficient drug-specific T cells are present in the blood and can be detected diagnostically with special cellular tests.
For more than 40 years, the lymphocyte transformation test (LTT) has been used here and is applied to a large number of drugs. The test is complex because it does not rely on the analysis of serum but detects the specific response of live T cells. The mononuclear cells (=lymphocytes, monocytes) are isolated from whole blood by density gradient centrifugation and subsequently cultured with the presumably triggering drug, which represents the allergen. Usually 3-5 concentrations are tested. After one week, proliferation of these cells is measured in the last 16 hours of cell culture by uptake of radiolabeled thymidine and compared with spontaneous proliferation without antigen. This ratio is called the stimulation index (SI). In general, an SI of 2-3 is considered positive and indicates the presence of specifically sensitized T lymphocytes. This test thus helps to identify the triggering drug and to confirm the suspicion of a drug allergy. respectively Determine the responsible drug when multiple drugs are administered.
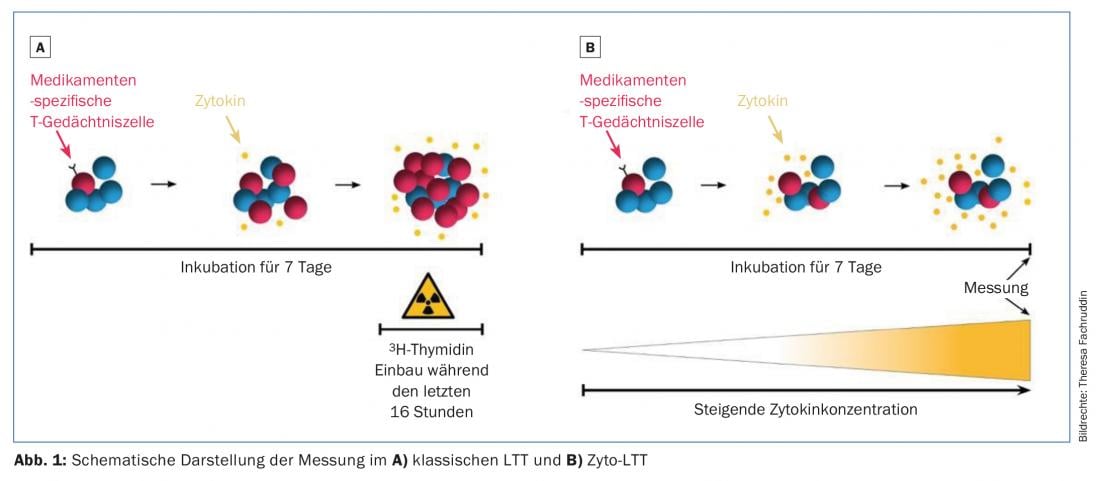
A disadvantage of the previous LTT is a partly low sensitivity depending on the drug. There are two reasons for this: First, only the proliferative cell response is measured over a short time window. With a short stimulation time, the cultured cells can already be dormant again and are then no longer detectable in the standard LTT. Second, drug allergies are very heterogeneous in their manifestations, and cellular-mediated responses do not result in a strong increase in proliferation in every case. It has already been shown that in cytotoxic reactions such as Stevens-Johnson syndrome, LTT yields a positive result for the causative drug in only 30% of cases. In such cases, the response is not based on increased proliferation, but rather on the release of cytotoxic mediators such as granzyme B and granulysin. In recent years, therefore, alternatives have been sought for the standard LTT described above.
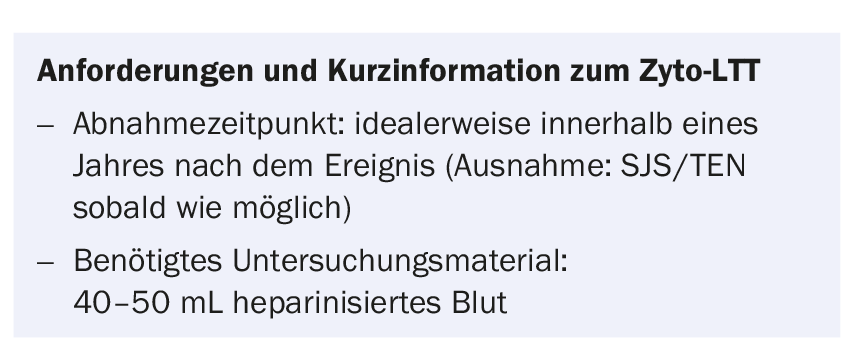
The diversity of clinical manifestations of drug allergy is based on the release of cytokines (IL-2, IL-4, IL-5, IL-13, IFN-γ,…) and cytotoxic molecules (granzyme B, granulysin, perforin,…). In an effort to improve the standard LTT (and replace radioactive methodology), the focus has been on selecting appropriate cytokines. The influence of cell number and time duration of cell culture as well as the exact culture conditions were investigated. The cyto-LTT (cytokine-LTT) resulting from these efforts measures the concentration of five mediators IL-5, IL-13, IFN-γ, granzyme B, and granulysin in cell culture supernatants by flow cytometry. The incubation period is seven days, and SI values are determined, analogous to the classic LTT. Increased sensitivity with consistently excellent specificity has been demonstrated in over 150 patients tested. An important reason for this is probably the non-proliferative responses, which can be detected with cytokine measurement in addition to proliferation, in contrast to classical LTT. An additional key advantage of cyto-LTT is its cumulative detection: cytokine levels have been shown to accumulate in culture supernatants over the entire seven-day period, whereas classical LTT detects only the last 16 hours of proliferation. Thus, by means of the cyto-LTT, the entire reaction period can now be indirectly followed.
The cyto-LTT has significant advantages over the classical LTT and has replaced it in the meantime. Sensitivity was improved to 50% (SJS, n=8) to 83% (MPE, n=36). The measurement of several functionally different cytokines is one reason for the increased sensitivity and also allows to better capture the heterogeneity of a disease pattern or reflects it in the test tube. It is even possible to draw conclusions about the dangerousness of the reaction. Preliminary data show that “banal” exanthema to e.g. amoxicillin is mainly associated with elevated IL-5/IL-13 levels, whereas all five measured parameters are elevated in patients with DRESS. In patients with Stevens-Johnson syndrome, again only granzyme B and granulysin levels and possibly IFN-γ are elevated.
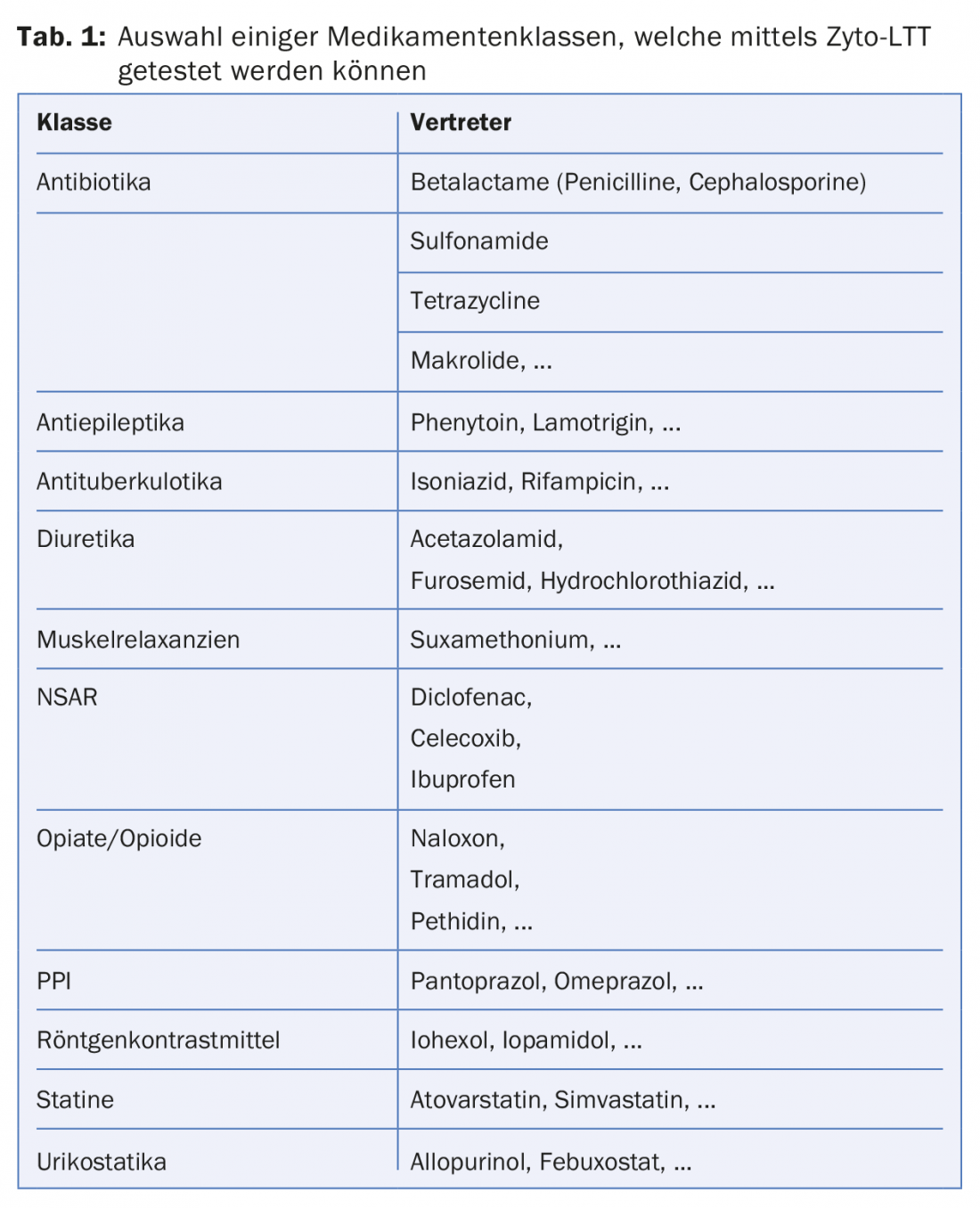
Cyto-LTT can facilitate the difficult diagnosis of drug allergies. To date, over 250 different drugs have been tested, and the most common are listed in Table 1. Since the cyto-LTT can provide clearly positive results even in the case of negative skin tests and is thus not infrequently more sensitive than the skin test, it can under certain circumstances even replace the technically and time-consuming skin test with drugs (intradermal or epicutaneous). On the other hand, it is an expensive test. Analyses are only justified if there is a reasonable suspicion of drug allergy and the indication for this should be made by the specialist.
Take-Home Messages
- Late-type allergies to medications can take a variety of forms, from mild exanthema to life-threatening reactions.
- Diagnosis is usually difficult and is based on history, skin testing and the classic lymphocyte transformation test (LTT).
- Provocation tests are poorly standardized for late type reactions (single dose or complete therapy cycle?)
- The cyto-LTT is based on the measurement of a combination of cytokines in cell culture supernatants and has replaced the classical LTT in routine diagnostics due to its higher sensitivity.
Further reading:
- Yawalkar N, Egli F, Pichler WJ, et al: Infiltration of cytotoxic T cells in drug-induced cutaneous eruptions. Clin Exp Allergy 2000; 30: 847-855.
- Pichler WJ: Immune mechanism of drug hypersensitivity. Immunol Allergy Clin North Am 2004; 24(3): 373-397, Review.
- Lochmatter P, Beeler A, Pichler WJ, et al: Drug-specific in vitro release of IL-2, IL-5, IL-13 and IFN-gamma in patients with delayed-type drug hypersensitivity. Allergy 2009; 64: 1269-1278.
- Naisbitt DJ, Farrell J, Pichler WJ, et al: Characterization of drug-specific T cells in lamotrigine hypersensitivity. J Allergy Clin Immunol 2003; 111(6): 1393-1403.
- Pichler WJ, Tilch J: The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy 2004; 59(8): 809-820.
DERMATOLOGIE PRAXIS 2018; 28(2): 23-25