Acute coughs are often viral and usually do not require the use of antibiotics – however, if pneumonia is present, antibiotics may be essential for survival. Chronic cough is a symptom of many different diseases. What are the latest findings regarding diagnostic procedures?
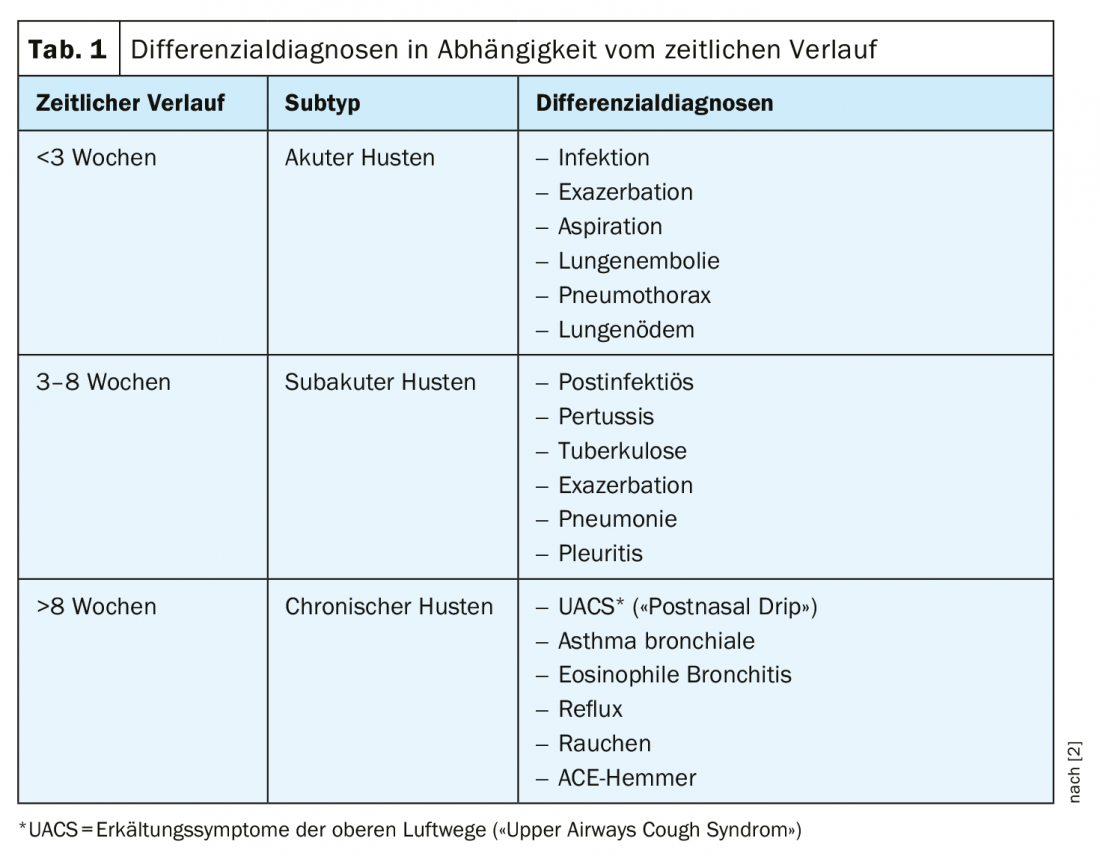
According to current guidelines, the following temporal criteria can be used to differentiate between different subtypes [1]: if <lasts 3 weeks, it is an acute form; if >lasts 8 weeks, it is a chronic form; if it lasts 3-8 weeks, it is a subacute form. Depending on the time course, various differential diagnoses can be considered (Table 1) [2]. Further clarification should be made in the following cases (“Red Flags”): Coughing up blood (hemoptysis), smoker/ex-smoker (>35 pack-years), dyspnea, cyanotic fever >38.5°C, suspected tuberculosis, weight loss, signs of heart failure, edema, dysphagia, hoarseness, recurrent pneumonia.
Suspected pneumonia: Infiltrate detection recommended
Acute cough is viral in 99% of cases and usually no use of antibiotics is required because it is self-limiting [2]. For upper respiratory tract infections, symptomatic therapy with decongestants, humidifiers and expectorants is often sufficient (CAVE: “Red Flags”, e.g. fever). However, the situation is different for lower respiratory tract infections. Community-acquired pneumonia is one of the infectious diseases with a high mortality rate and requires antibiotic treatment [3]. In contrast to bronchitis, this microbially caused inflammation not only affects the deep airways, but also directly affects the lung parenchyma. Classic symptoms include cough (with or without sputum), dyspnea, and respiratory-related chest pain, as well as impaired general condition (fever or hypothermia, lassitude, myalgias, arthralgias, and cephalgias, and neurologic symptoms such as disorientation). Since these symptoms do not allow specific differentiation from other lower respiratory tract infections, further clarification is required. However, the predictive value of leukocyte count, C-reactive protein (CRP), and procalcitonin (PCT) is not very high. PCT as a biological marker is predominantly relevant for patients with severe pneumonia, according to Daniel Franzen, MD, University Hospital Zurich [2]. A completely unremarkable auscultation finding, i.e., an absence of pneumonic rales, has a high negative predictive value [4]. Infiltration detection by imaging allows reliable differentiation from acute bronchitis, which, unlike pneumonia, does not necessarily need to be treated with antibiotics [5].
Antitussives and protussives against cold cough
Cold cough or acute (tracheo-)bronchitis usually lasts 5-21 days. The causes are predominantly viral, with only 3-5% of cases being bacterial. Since it is usually self-limiting, no antibiotics need to be used – with the exception of pertussis. Regarding symptomatic therapy, there are new treatment recommendations from the German Society of Pneumology (DGP)[6]. Consequently, protussive and antitussive agents are the main therapeutic principles. Protussives cause elimination of secretions, resulting in relief of cough receptors. This can be achieved by secretolytics or mucolytics, which are characterized by polyvalent action (anti-inflammatory, antioxidant, local anesthetic, antiviral). Antitussives are classically prescribed for irritable cough and result in elimination of mucus production. Substances in this class include demulcent agents and some antihistamines. Also having antitussive properties are certain opiates, local anesthetics, inhaled corticosteroids, and antibiotics.
Solmucalm® is a drug with a combined mechanism of action. N-acetylcysteine causes liquefaction of mucus. Chlorphenamine, an anticholinergic antihistamine, reduces the excitability of TRPV1 receptors that can be activated by viruses. Regarding alternative medicine for cold cough, a meta-analysis demonstrated superior efficacy for several phytotherapeutic expectorants (e.g., anise, eucalyptus, ribwort, thyme) and for some antitussives (e.g., thyme, ivy, primrose, eucalyptus, ribwort) compared with placebo [2,7].
Clarification algorithm for chronic cough
Since there are many possible differential diagnoses of chronic cough, identifying the underlying causes is a particular challenge. The most common and important diseases include [6]:
- Upper respiratory tract diseases: Chronic. Diseases of the nose and sinuses or pharynx and larynx, chronic. Ear affections, VCD (“vocal cord dysfunction”)
- Asthma
- Eosinophilic bronchitis
- Chronic bronchitis and COPD
- Bronchiectasis disease
- Lung parenchymal diseases
- Gastroesophageal reflux
- Tuberculosis
- Somatic cough syndrome (formerly: psychogenic or habitual cough).
- Cough Tic

In the current guidelines of the DGP [6], a clarification algorithm was defined (Fig. 1) . An overview of the recommendations for the diagnosis of chronic cough [6]: X-ray of the thoracic organs and pulmonary function testing can diagnose the most common diseases (e.g., COPD, asthma, lung tumors, tuberculosis, aspiration, lung parenchymal diseases). Before a diagnosis of chronic bronchitis is made, other causes must be ruled out (e.g., smoker’s bronchitis). Substitution may be attempted in patients treated with ACE inhibitors. If neither radiography nor pulmonary function tests lead to clear findings, upper respiratory tract disease or gastroesophageal reflux should be considered as triggers of chronic cough. Furthermore, rare diseases of the tracheobronchial system (including bronchiectasis), side effects of various medications and cardiac diseases with pulmonary congestion as well as pertussis, tuberculosis and early stages of diffuse lung parenchymal diseases should be considered. Multislice computed tomography of the thorax and bronchoscopy are recommended as further diagnostic tests. Lack of treatment response of chronic cough in patients with reflux, asthma, or sinusitis is chronic refractory cough, which mostly affects middle-aged women. In some cases, the etiology of chronic cough remains unclear; this is subsumed under the term “chronic idiopathic cough.”
Source: FOMF Zurich
Literature:
- Gibson P, et al: Treatment of Unexplained Chronic Cough. CHEST Guideline and Expert Panel Report. CHEST 2016; 149 (1): 27-44.
- Franzen DP: Slide presentation, PD Daniel P. Franzen, MD. Symposium: Cold, Cough, Pneumonia – Practical Tips & Tricks from Pneumology. Internal Medicine – Update Refresher. 03.12.2019, Zurich
- Murray CJ, Lopez AD: Measuring the global burden of disease. N Engl J Med 2013; 369: 448-457.
- Leuppi JD, et al: Diagnostic value of lung auscultation in an emergency room setting. Swiss Med Wkly 2005; 135(35-36): 520-524.
- Smith SM, Fahey T, Smucny J, Becker LA: Antibiotics for acute bronchitis. Cochrane Database Syst Rev 2014; 3: CD000245.
- Kardos P et al: Guideline of the German Society of Pneumology and Respiratory Medicine for the Diagnosis and Therapy of Adult Patients with Cough, https://pneumologie.de/fileadmin/user_upload/DGP_Husten_2019.pdf
- Wagner L, et al: Herbal Medicine for Cough: a Systematic Review and Meta-Analysis. Forsch Komplementmed 2015; 22(6): 359-368.
HAUSARZT PRAXIS 2020; 15(2): 25-26 (published 2/6/20, ahead of print).