RSV infection is associated with hospitalizations and deaths in adults with cardiovascular and respiratory disease. However, most studies have focused on the association in the older population; less is known about the cardiac complications of RSV disease and the risk across the adult age spectrum. A recent study has now shown that the risk of HI is increased from the age of 50.
Although respiratory syncytial virus (RSV) is a common cause of lower respiratory tract infections in infants and children, it can also cause severe disease in the elderly and adults with cardiopulmonary conditions such as heart failure (HF). In addition, studies to date have been limited by a lack of consideration of risk factors for cardiac events or their severity.
A team of researchers from the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC), Atlanta, USA, led by Dr. Stephanie A. Kujawski, conducted a study quantifying the rate of RSV infection in hospitalized adults based on their HIV status and age [1]. They used data from the population-based RSV surveillance (RSV-NET) in the United States.
Surveillance was conducted over two respiratory seasons (2015-2017) from October 1 through April 30 of each year at seven sites across the United States. The study enrolled adults ≥18 years of age who received a laboratory-confirmed diagnosis of RSV infection within 14 days of hospitalization or at any time during their hospital stay. The diagnosis was based on tests ordered by the treating physician. In addition, demographic and clinical information, including the presence of underlying heart failure, was obtained from medical records by trained staff.
HI patients had an 8.1 times higher hospitalization rate due to RSV
The researchers identified 2204 RSV cases who were hospitalized, of which 2042 (92.6%) had a registered HI status. Of these participants, 1230 (60.2%) were aged ≥65 years and 1208 (59.2%) were female. The median duration of hospitalization was 4 days (IQR: 3-7). 414 patients (20.3%) had to be transferred to the intensive care unit and 101 (4.9%) died during hospitalization.
The results showed that over a quarter of hospitalized patients with RSV (28.3%) suffered from heart failure. The majority of them were ≥65 years old (73.5%). Hospitalized RSV cases with heart failure were older, with a median age of 76 years versus 67 years (p<0.001), and were more likely to also have chronic obstructive pulmonary disease (COPD) compared to hospitalized RSV cases without heart failure (39.9% vs. 29.1%, p<0.001). They were also more likely to be obese or morbidly obese (41.6% vs. 34.5%).
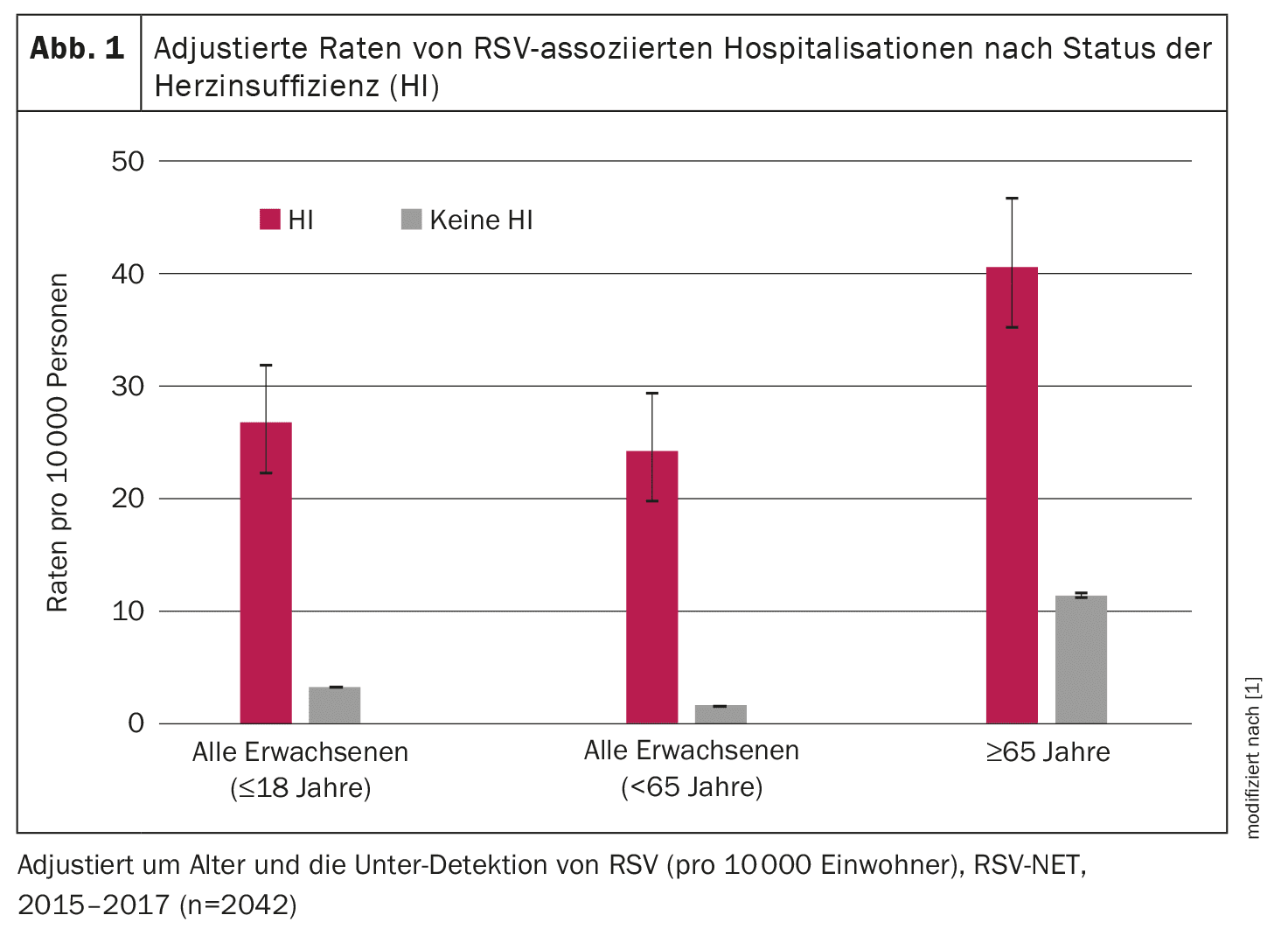
Overall, there were 23.4 (95% CI 18.9-28.5) additional cases of RSV-related hospitalizations per 10,000 population in adults with chronic HI compared to adults without chronic HI (Fig. 1). In addition, patients with heart failure were more frequently admitted to the ICU (24.5% vs. 18.6%, p=0.003) and also a higher proportion of patients died during their hospitalization (7.8% vs. 3.8%, p<0.001) compared to patients without HI. Similar trends in characteristics and clinical outcome by HI status were observed when stratified by age groups <65 and ≥65 years. In patients with chronic HI, the rate of RSV hospitalization was 8.1 times higher than in patients without chronic HI (95% CI 6.8-9.7). Adults aged ≥65 years with heart failure were 3.5 times (95% CI 3.1-4.0) more likely to be hospitalized with RSV than adults without HI (RD: 29.1; 95% CI 23.9-34.9). In adults under 65 years of age with chronic heart failure, the RSV rate was 14.3 times (95% CI 11.8-17.3) higher than in adults without chronic heart failure (RD: 22.5; 95% CI 18.1-27.6).
According to the authors, this is one of the first studies to calculate hospitalization rates due to RSV in all adults by HI status. These results highlight the increased burden of RSV hospitalizations in adults with HI in all age groups, which is important for decision making regarding RSV prevention and therapeutic interventions in adults with HI.
Significantly higher risk of suffering an acute cardiac event
Numerous studies have already shown that RSV infection can cause severe respiratory disease in older people. However, compared to influenza and SARS-CoV-2 infections, less is known about the cardiac complications of RSV disease.
Dr. Rebecca Woodruff of the Division of Heart Disease and Stroke Prevention, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, and her colleagues conducted a cross-sectional study in which they analyzed the incidence and severity of acute cardiac events during hospitalization in adults 50 years and older with RSV infection by collecting and analyzing surveillance data from the RSV Hospitalization Surveillance Network [2]. The network maintains detailed medical records of hospitalized patients with RSV infection detected by physician-ordered laboratory tests.
The study included 6248 hospitalized adults (mean age [IQR]: 72.7 [63,0–82,3] years, 59.6% female). More than half (56.4%) of the participants had underlying cardiovascular disease (CVD) with laboratory-confirmed RSV infection. In addition, the results showed that the weighted estimated prevalence of a cardiac event was 22.4% (95% CI 21.0-23.7). For acute heart failure, the value was 15.8% (95% CI 14.6-17.0) and for acute ischemic heart disease 7.5% (95% CI 6.8-8.3). In addition, the weighted estimated prevalence for hypertensive crisis was 1.3% (95% CI 1.0-1.7), for ventricular tachycardia 1.1% (95% CI 0.8-1.4) and for cardiogenic shock 0.6% (95% CI 0.4-0.8).
Adults with underlying cardiovascular disease were found to have a higher risk of an acute cardiac event than adults without such disease (33.0% vs. 8.5%; ARR 3.51; 95% CI 2.85-4.32). Of all hospitalized adults with RSV infection, 18.6% required ICU admission and 4.9% died during hospitalization. The risk of ICU admission was higher in those with an acute cardiac event than in those without (25.8% vs. 16.5%; ARR 1.54; 95% CI 1.23-1.93), as was in-hospital death (8.1% vs. 4.0%; ARR 1.77; 95% CI 1.36-2.31).
This cross-sectional study examined cases of RSV infection in adults ≥50 years of age in 12 states during five RSV seasons (annually from 2014/2015 through 2017/2018 and 2022/2023). Nearly a quarter of these hospitalized patients experienced an acute cardiac event (most commonly acute heart failure), including one in 12 adults (8.5%) without documented cardiovascular disease. The risk of severe outcomes was almost twice as high in patients with acute cardiac events as in patients who did not experience an acute cardiac event.
These findings not only highlight the epidemiology and potential risk of cardiac complications during RSV infection, but also show the great need for prevention and active protection against RSV infection in adults, especially through vaccines, Dr. Woodruff and colleagues conclude.
Literature:
- Kujawski SA, et al: Rates of respiratory syncytial virus (RSV)-associated hospitalization among adults with congestive heart failure-United States, 2015-2017. PLoS ONE 2022; 17(3): e0264890; doi: 10.1371/journal.pone.0264890.
- Woodruff RC, et al: Acute Cardiac Events in Hospitalized Older Adults With Respiratory Syncytial Virus Infection. JAMA Intern Med 2024; 184(6): 602-611; doi: 10.1001/jamainternmed.2024.0212.
CARDIOVASC 2024; 23(3): 34-35