Scalp diseases are many. For an accurate diagnosis, it is necessary to distinguish whether the hair follicles, the scalp or a combination of both is affected. Depending on the cause and severity, there are different treatment strategies. In his presentation, de Viragh, MD, also provided an outlook on changing therapeutic approaches.
Scalp diseases are many. For an accurate diagnosis, it is necessary to distinguish whether the hair follicles, the scalp or a combination of both is affected. Furthermore, diseases of this type are divided into inflammatory and non-inflammatory pathologies. In addition to a parasitic infestation, microbial inflammations, i.e. an infestation with fungi, bacteria or viruses, and a so-called sterile inflammation, i.e. an infection without causative microorganisms, can be considered as differential diagnoses.
Seborrheic dermatitis
Seborrheic dermatitis occurs mainly in areas with a large number of sebaceous glands. The cause of the greasy, scaly skin disease is probably increased sebum production and excessive colonization with Malassezia yeasts. Greasy, yellowish scales appear on a mostly reddened background. Etiologic factors for the development of seborrheic dermatitis include [1]:
- The amount of sebum production
- Colonization with Malassezia restricta and globosa
- Individual sensitivity (differences in barrier function, immune system, microflora).
Therapeutically, attempts are made to reduce the amount of sebum. This can be done by using shampoos containing tar. In difficult cases, systemic therapy with isotretinoin at a low dosage may also be used in long-term application. The second therapeutic approach is directed against colonization with Malassezia yeasts. Azoles, other antifungal agents or zinc pyrithione and selenium can help here. If possible, preventive treatment should be given and with a prevalence of approximately 10% of seborrheic dermatitis in the population, over-the-counter products are best. There are some shampoos on the market as antifungal preparations. However, these usually only have a very short residence time on the affected scalp. Alternatively, a tincture can be used, such as DermoCapillaire Anti-Dandruff Tincture from Eucerin®, which can be left on the scalp. The long exposure time can thus achieve some additional improvement in effectiveness, the speaker said.
In severe courses of seborrheic dermatitis with an inflammatory clinical picture, transient alopecia may occur (Fig. 1). In the case of very pronounced inflammation, the so-called “scarring seborrheic dermatitis Laymon”, scarring and thus definitive alopecia may occur [2,3]. Therapy then consists primarily of systemic steroids to combat the inflammatory reaction as effectively as possible.
Pityriasis amiantacea is another severe form of seborrheic dermatitis (Fig. 2) . The reaction pattern may resemble psoriasis in 2-15% of cases and, primarily in children, also tinea capitis (<5% of tinea capitis cases are in postpubertal patients). However, until these differential diagnoses are proven, the suspected diagnosis in an adult patient remains seborrheic dermatitis. Treatment should consist of systemic antifungal therapy for four weeks. In rare cases, the clinical picture of pityriasis amiantacea may also be associated with lichen planopilaris, folliculitis decalvans, impetigo (especially in children), or erosive pustular dermatosis.
Folliculitides
These pustular diseases of the hair follicles may result from mechanical stress, triggered, for example, by scratching due to itching in trichotillomania or atopic dermatitis. Similarly, they may occur as a symptom of a complex clinical picture, such as fungal and bacterial infections, neutrophilic and mixed scarring alopecia, or pustular psoriasis [4].
Acne-like scalp dermatoses describe the clinical picture of centrally or peripherally located isolated pustules and may lead to the following tentative diagnosis:
- “Red scalp” with pustules (and without pustules, the “Red Scalp Syndrome”).
- Rosacea (Fig. 3)
- Folliculitis caused by steroids
- Gram-negative folliculitis
- Chronic non-scarring folliculitis of the scalp
- Folliculitis necroticans varioliformis.
It is important to note that, in contrast to “true” acne, all of these clinical pictures occur without accompanying comedones or hypertrophic scarring.

For the treatment of acne-like scalp dermatoses, topical medications are ineffective. An attempt at therapy with tetracyclines can be started [5]. An exception is Gram-negative folliculitis; since this condition may be antibiotic-induced, these should rather be avoided. Isotretinoin also shows good efficacy. In folliculitis necroticans varioliformis, which tends to occur peripherally and frontally on the head and whose crusts leave belly-button-like scars, tetracyclines also usually do not help well, so isotretinoin is often switched to, Dr. de Viragh reported.
If comedones are visible on the scalp, early perifolliculitis suffodiens et abscedens should be considered as a “monosymptomatic acne tetrade”. Since this disease is difficult to treat, high-dose specific therapy should be given from the beginning.
A very rare condition that can occur in young children and is associated with clustering pustules on the head is eosinophilic pustular folliculitis (Fig. 4). Recurrent apparently infectious folliculitis is found. A smear or biopsy shows multiple eosinophils. This condition is self-limiting; parents need to be reassured, and topical steroids can be used to treat it if necessary [6].
The symptom of red scalp
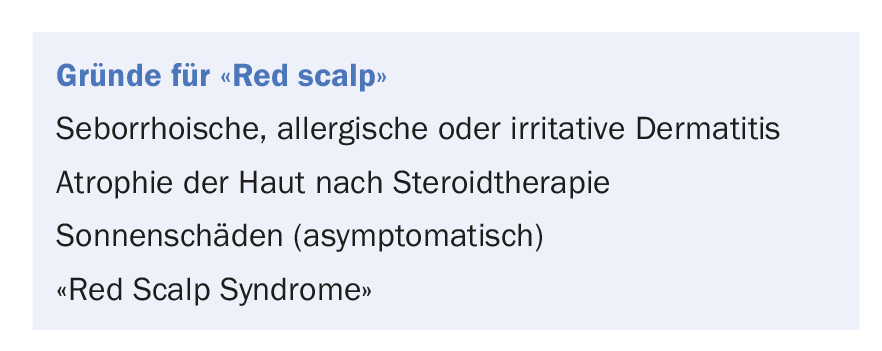
Red scalp as a symptom has its very own differential diagnoses – from simple irritation from cosmetics to sun damage. The box provides an overview. It is important that a scalp thinned by long-term steroid therapy is not further atrophied after the underlying disease has been cured, because the residual redness due to telangiectasia is misinterpreted as persistence of the disease.
The “Red Scalp Syndrome” is an actual “driving physicians crazy syndrome”. Clinically, a persistent redness of the scalp with itching and a burning sensation is noticeable, which cannot be explained by other causes. Steroids do not help here, on the contrary, they worsen the symptoms. The therapy of choice is tetracyclines. Topical preparations of witch hazel (Erol® or Mavena shampoo and tonic) are also relatively effective [7].
Outlook
A very common inflammatory disease of the scalp is frontal fibrosing alopecia (Kossard’s disease). Controversy exists regarding the etiopathogenesis. A form of scarring androgenetic alopecia or a variant of lichen planopilaris are discussed. With different therapeutic approaches, accurate diagnosis is desirable. A study is currently being conducted by a research group headed by Dr. de Viragh on this issue and on the most appropriate form of therapy in each case.
Source: Swiss Derma Day and STI reviews and updates, January 10-11, 2018, Lucerne.
Literature:
- DeAngelis YM, et al: Three etiologic facets of dandruff and seborrheic dermatitis: Malassezia fungi, sebaceous lipids, and individual sensitivity. J Investig Dermatol Symp Proc 2005; 10(3): 295-297.
- Laymon CW: The cicatricial alopecias; an historical and clinical review and an histologic investigation. J Invest Dermatol 1947; 8(2): 99-122.
- Sperling LC, et al: The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg 2006; 25(1): 41-50.
- Lugović-Mihić L, et al: Differential diagnosis of the scalp hair folliculitis. Acta Clin Croat 2011; 50(3): 395-402.
- Hersle K, et al: Chronic non-scarring folliculitis of the scalp. Acta Derm Venereol 1979; 59(3): 249-253.
- Dupond AS, et al: Eosinophilic pustular folliculitis in infancy: report of two affected brothers. Br J Dermatol 1995; 132(2): 296-299.
- Trüeb RM: North American Virginian Witch Hazel (Hamamelis virginiana): Based Scalp Care and Protection for Sensitive Scalp, Red Scalp, and Scalp Burn-Out. Int J Trichology 2014; 6(3): 100-103.
DERMATOLOGIE PRAXIS 2018; 28(1): 38-40











