The risk of having an allergic reaction after an insect bite ranges from 0.3-8.9%. Not every sting reaction is the same as an allergy. The correct assessment of a reaction facilitates the decision of further diagnostics and possible specific treatment.
Insect bites are among the most common causes of severe allergic reactions, along with drugs and food. The incidence of fatal events worldwide is estimated at 0.03 to 0.48 per million population. In Switzerland, about one to four people die each year due to a severe allergic reaction following an insect bite. In Europe, insects from the two families Apidae (honeybee/Apis melifera, bumblebees/Bombus terrestris/B. agrotum) and Vespidae (short-headed wasp/Vespula germanica/V. vulgaris, longheaded wasps/Dolichovespula media, D. saxonica, hornets/Vespa crabro, field wasps/Polistetdominulus/P. gallicus) are significant for the allergic events [1]. Short-headed wasps show a preference for human food, so stings often occur in association with food and/or social events such as picnics and barbecues, usually in mid/late summer. Stings of hornets and longheaded wasps occur practically only near the nest. As a rule, the barbed bee stinger gets stuck in the skin. Less known is that the wasps can also occasionally lose the sting.
If a general allergic reaction occurs after an insect bite, an allergological evaluation with regard to venom-specific immunotherapy (VIT) should be initiated in the course (optimally about three to six weeks after an acute event). VIT has been established worldwide as the only causal and highly effective (effectiveness in wasp venom allergy >95% and bee venom allergy 80-85%) method.
Clinical manifestations
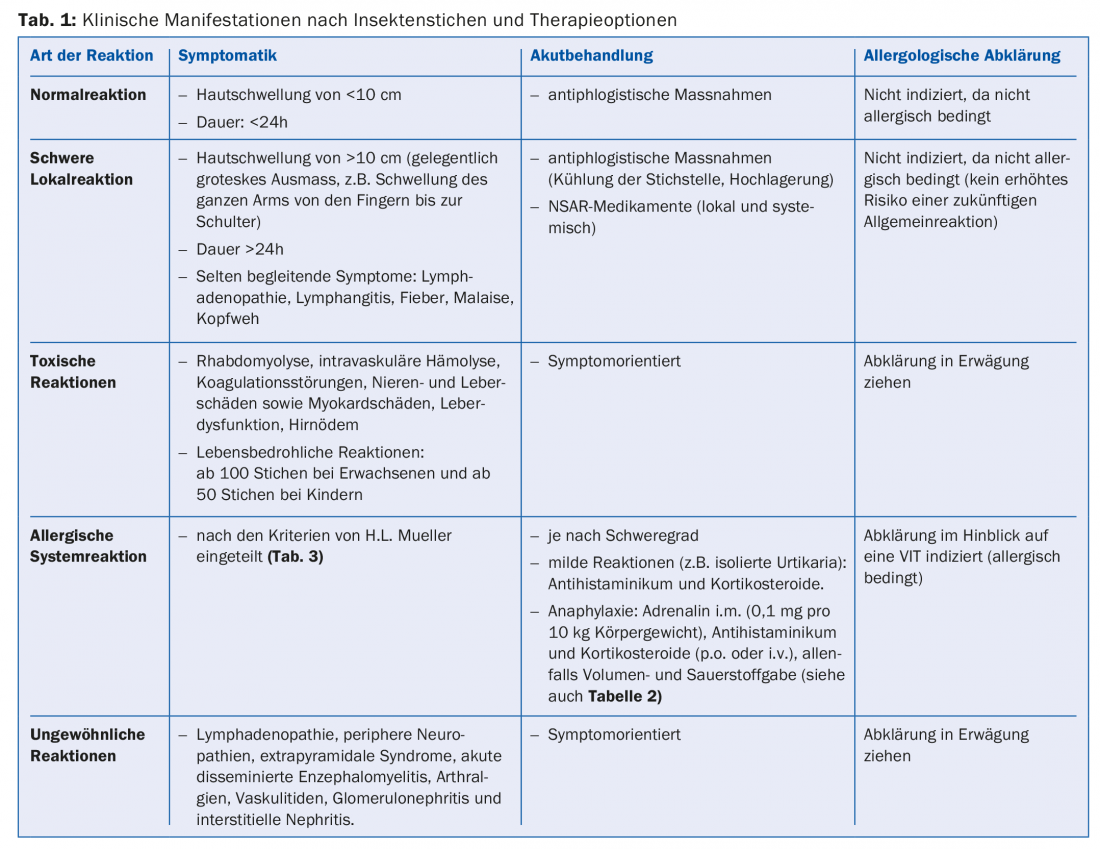
For many people, insect bites cause painful local swelling. These local sting reactions, although severe (skin swelling of >10 cm, duration >24h), are usually not allergic. According to studies, those with severe local reactions to insect bites do not have an increased risk of a future general allergic reaction. Systemic toxic reactions caused by cytotoxic effects of venom toxins such as melittin, phospholipases and kinins after multiple insect bites are also not allergic in nature. If sensitization to components of the venom occurs after a sting, an allergic reaction could develop as a consequence of this sensitization in the event of repeated stings. The various clinical manifestations of sting reactions have been summarized in Table 1.
Allergic reactions after insect bites
According to the latest literature reports, up to 50% of the population may have asymptomatic sensitization to bee and wasp venom [2]. The prevalence of an allergic systemic reaction after a hymenopteran sting is estimated between 0.3-8.9%. The risk of allergic reaction is particularly high when two stings occur within a short time. After a mild general reaction, the risk of a recurrence of a systemic reaction in adults is about 30%, and after a severe one it is as high as 50-70% [3]. Elevated basal serum tryptase has been shown to be an important risk factor for a general reaction after an insect bite [4]. Other factors such as underlying diseases (severe cardiovascular disease, COPD GOLD III-IV, severe asthma), older age (>70 years) and treatment with beta-blockers or ACE inhibitors may also increase the risk. Atopics (e.g., those allergic to pollen or house dust mites) are not known to be at increased risk for an allergic reaction to insect bites.
Treatment of allergic reaction
The treatment principle for any allergic reaction is uniform regardless of triggers. According to the recommendation of the World Allergy Organization (WAO) and national guidelines, intramuscular administration of epinephrine is the treatment of choice for anaphylaxis [5]. There is no absolute contraindication for the use of epinephrine in severe allergic reaction. In adults, the initial dose is 0.3-0.5 mg (rule of thumb 0.1 mg per 10 kg body weight). Other treatment measures for anaphylaxis are shown in Table 2. Mild reactions such as isolated urticaria and/or mild angioedema can be treated with an antihistamine, although a therapeutic effect can be expected after oral administration after half an hour at the earliest.
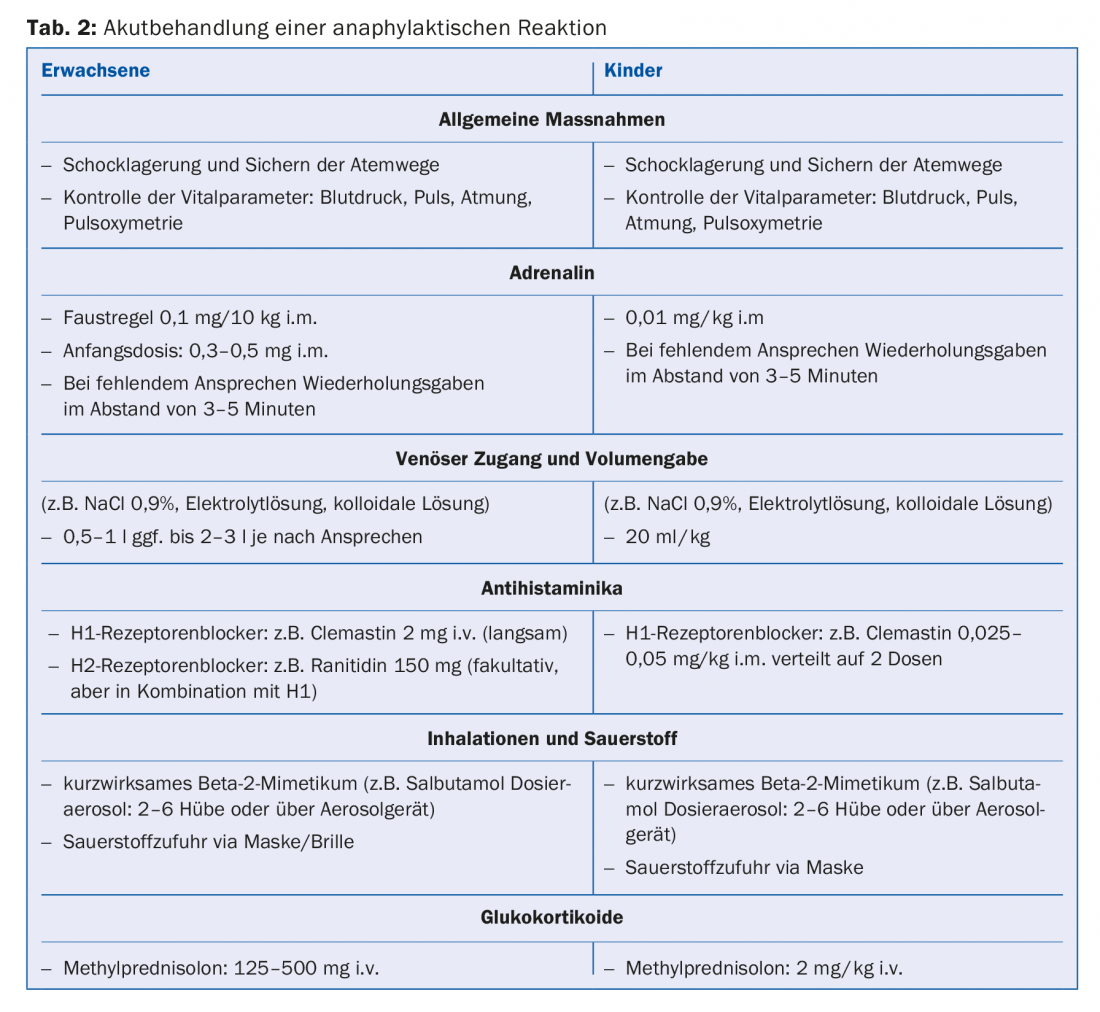
Every patient should carry emergency medications after a systemic reaction following an insect bite. The emergency kit consists of antihistamines (e.g., two tablets of levocetericine, cetericine, or fexofenadine) combined with a corticosteroid preparation (e.g., two tablets of prednisone 50 mg each) and epinephrine auto-injector (Epipen, Jext). In infants, antihistamine drops (e.g., levocetericine drops 0.25-0.5 mg/kg/day), water-soluble cortisone tablets (e.g., betnesol 0.2-0.5 mg/kg), and Epipen Junior (in children >7.5 kg and <25 kg) should be prescribed [6].
Diagnosis of insect venom allergy
Allergic evaluation is recommended in every patient after a systemic reaction following a bee/wasp sting, especially to assess whether venom-specific immunotherapy (VIT) is indicated [7]. Specialist site assessment is based on a detailed history, intradermal testing with increasing concentrations of bee and wasp venom, and venom component-based molecular allergy diagnostics (Fig. 1).
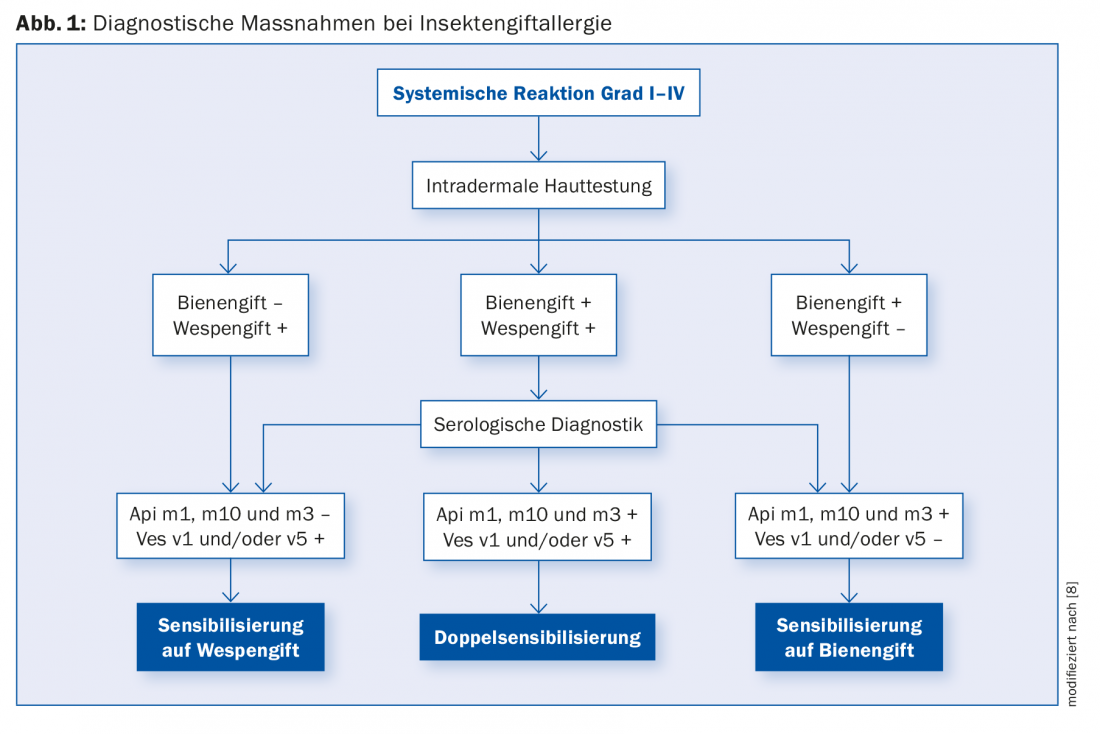
For the serological diagnosis of wasp venom allergy, the recombinant major allergens Ves v5 and Ves v1 are available (test sensitivity with a combination of both allergens is 97%). Api m1, m10, m2, m5 and m3 are available for bee venom allergy, resulting in a detection rate of 93% when all five bee venom components are determined [8].
If testing is negative despite suggestive history, repeat testing a few weeks later is recommended. In addition, an in vitro analysis, the “basophil activation test” (BAT), can be performed. If sensitization is again not detected in the second test, VIT is usually not indicated. We do not recommend diagnostic provocation tests with live insects.
Venom-specific immunotherapy (VIT)
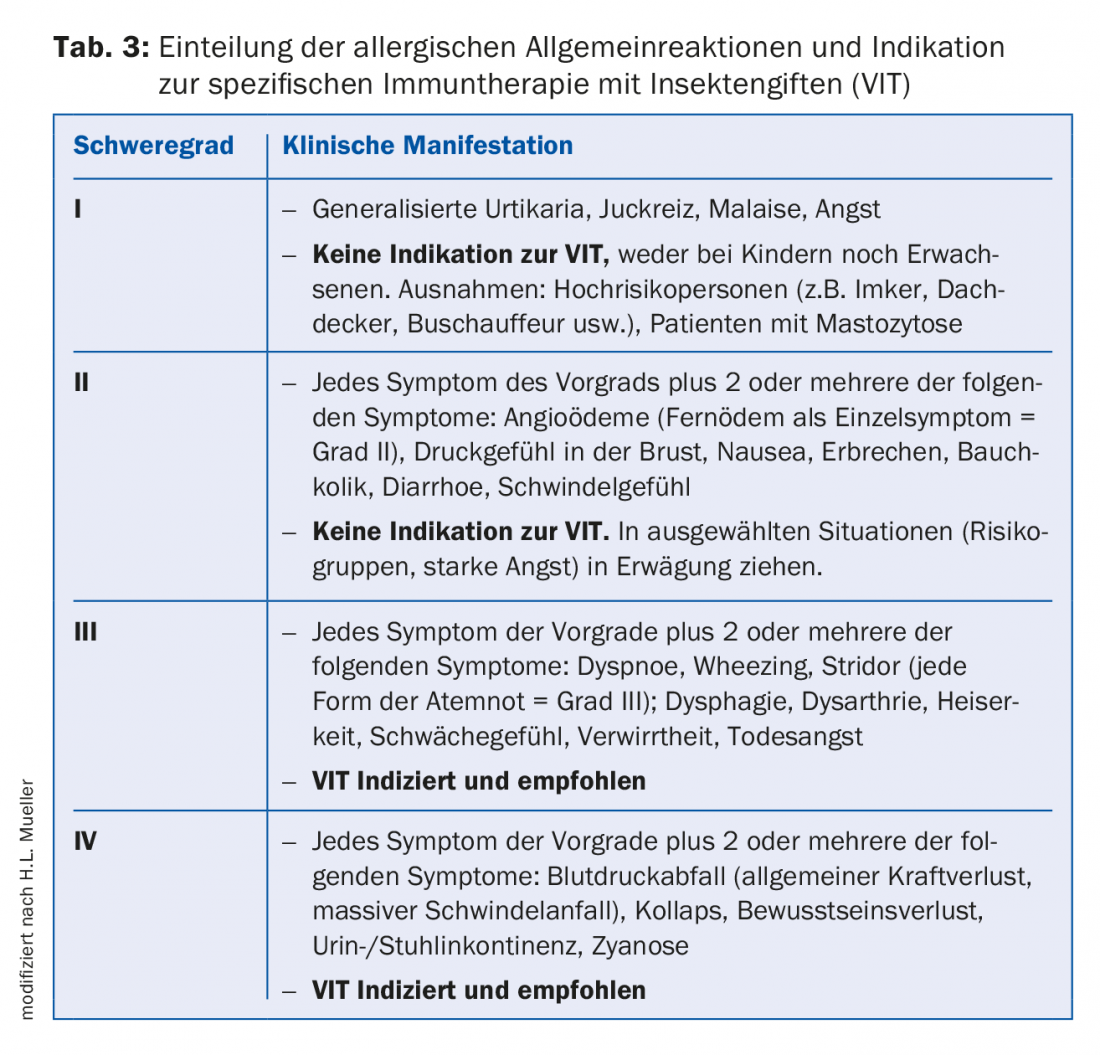
VIT with bee and wasp venom is considered the only causal and very effective treatment for insect venom allergy [9]. In all patients who have had a severe general reaction with respiratory and/or circulatory involvement after a bee or wasp sting (severity III and IV according to H.L. Mueller, Tab. 3) have suffered and show sensitization to bee or wasp venom in the course of allergological clarification, VIT with appropriate insect venom is indicated. Other indications for VIT (even in mild grade I and II reactions) are: high sting exposure and special risk occupations (beekeepers, farmers, gardeners, chauffeurs, roofers) and proven mastocytosis. In the context of an allergological assessment, other factors such as concomitant cardiac and/or pulmonary diseases, medications, and a reduction in quality of life due to anxiety or panic attacks should also be taken into account when determining the indication.
VIT consists of two phases: Initiation and Maintenance Therapy. Initiation of VIT should be done by allergists. Most often, this is done by ultra-rush (several hours of hospitalization with repeated subcutaneous injections until the maintenance dose is reached). The maintenance dose is usually 100 mcg of the appropriate venom for both children and adults and is equivalent to one to two bee stings and several wasp stings. In beekeepers, a maintenance dose of 200 mcg is targeted a priori.
During continuation treatment, which may be provided by the primary care physician, the maintenance dose is administered subcutaneously every four weeks. From the second year of treatment, the injection interval can be extended to six weeks if the course is unremarkable. The total duration of VIT is usually five years, although longer, or at most lifelong, treatment is recommended in patients with life-threatening reactions, systemic mastocytosis or markedly elevated basal serum tryptase, and patients with significant cardiovascular and/or pulmonary comorbidities [10].
Take-Home Messages
- The risk of having an allergic reaction after an insect bite ranges from 0.3-8.9%. Beekeepers have a higher risk of allergy than the general population at 14-43%. In Switzerland, up to four people die each year after an insect bite.
- Not every sting reaction is the same as an allergy. The correct assessment of a reaction facilitates the decision of further diagnostics and possible specific treatment.
- All patients with a general reaction after an insect bite should be clarified allergologically with regard to specific immunotherapy (the only effective causal therapy).
- In an emergency, intramuscular epinephrine is the treatment of choice (intial 0.3-0.5 mg). Mild reactions can be treated with an antihistamine. Corticosteroids are not primary emergency medications for anaphylaxis.
- All patients with a general allergic reaction after an insect bite should carry an emergency kit (epinephrine auto-injector 0.3 mg and emergency tablets e.g. 2× 10 mg cetericine and 2× 50 mg prednisone). The handling of the auto-injector must be checked regularly.
Literature:
- Bilò MB, Bonifazi F: The natural history and epidemiology of insect venom allergy: clinical implications. Clin Exp Allergy 2009; 39: 1467-1076.
- Stoevesandt J, et al: Sensitization to hymenoptera venom marker allergens: prevalence, predisposing factors, and clinical implications. Clin Exp Allegy 2018; doi: 10.1111/cea.13237 [Epub ahead of print].
- Helbling A, Müller UR: Update on insect venom allergy with special aspects in diagnosis and therapy. Review Article. Allergo J 2013; 22: 265-273.
- Vázquez-Revuelta P, González-de-Olano D: Prevalence of clonal mast cell disorders in patients presenting with hymenoptera venom anaphylaxis might be higher than expected. J Investig Allergol Clin Immunol 2018; 28: 193-194.
- Simons FE, et al: 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organ J 2015; 8: 32.
- Bilò MB, et al: Self-medication of anaphylactic reactions due to Hymenoptera stings-an EAACI Task Force Consensus Statement. Allergy 2016; 71: 931-943.
- Alfaya AT, et al: Key issues in hymenoptera venom allergy: an update. J Investig Allergol Clin 2017; 27: 19-31.
- Jakob T, et al: Component resolved diagnostics for hymenoptera venom allergy. Curr Opin Allergy Clin Immunol 2017; 17: 363-372.
- Oppenheimer J, Golden DBK: Hymenoptera venom immunotherapy: past, present, and future. Ann Allergy Asthma Immunol 2018; 121: 276-277.
- Ruëff F, et al: Clinical effectiveness of hymenoptera venom immunotherapy: a prospective observational multicenter study of the European academy of allergology and clinical immunology interest group on insect venom hypersensitivity. PLoS One 2013; 8: e63233.
HAUSARZT PRAXIS 2018; 13(10): 18-23
DERMATOLOGIE PRAXIS 2019; 29(4): 18-21











