Lyme serology or even PCR (polymerase chain reaction) tests are by no means always necessary when it comes to diagnosing skin borreliosis and initiating treatment. In typical erythema migrans, the motto is: do not search for antibodies, but treat directly. Early antibiotic therapy may even prevent seroconversion. Serologies for therapy or progression control are useless. Prof. Dr. Martin Hartmann, Heidelberg, spoke about the place of serology in Lyme disease diagnostics at the 2017 Annual Meeting of the SGDV.
Lyme disease diagnosis is based on the clinical findings (supplemented by the medical history), on the differential diagnosis and in certain cases additionally on serology. Only a quarter of patients remember being bitten by a tick. The disease can have a long course, but this varies greatly from individual to individual. For this reason, two manifestation phases of skin Lyme disease have recently been distinguished instead of the previous three stages: the early manifestations of the early phase (localized early infection: erythema migrans or, in the case of longer duration, erythema chronicum migrans, borrelia lymphocytoma; disseminated early infection: multiple erythemata migrantia) and the late phase (late infection of the skin: edematous infiltration and acrodermatitis chronica atrophicans) [1]. Serology is most important and also easiest in the late phase, the speaker said.
Erythema migrans: typical or atypical, rarely multiple
After the tick bite, the Borrelia bacteria remain in the area of the entry site for about a week. After that, the swarming begins, which manifests as erythema migrans. If the pathogens have entered the blood, serological testing becomes possible. Acute or chronic erythema migrans begins within four weeks after the tick bite (on average after seven to fourteen days) and spreads. It may have marginal tenderness and may be facultatively itchy or painful. It is often axillary, inguinal, or popliteal in location. General symptoms such as fever, myalgia, arthralgia, fatigue may occur. Because different Borrelia bacteria are present in North America than in Europe, the clinic is different in the two continents. The subspecies Borrelia burgdorferi sensu stricto, which occurs in the United States, is “arthritogenic,” whereas the human pathogenic subspecies Borrelia afzelii and Borrelia garinii, which are most common in Europe, are “dermotropic” and “neurotropic,” respectively. In Europe, Lyme disease manifests as skin Lyme disease in 80-90% and other organs in 10-20% [1].
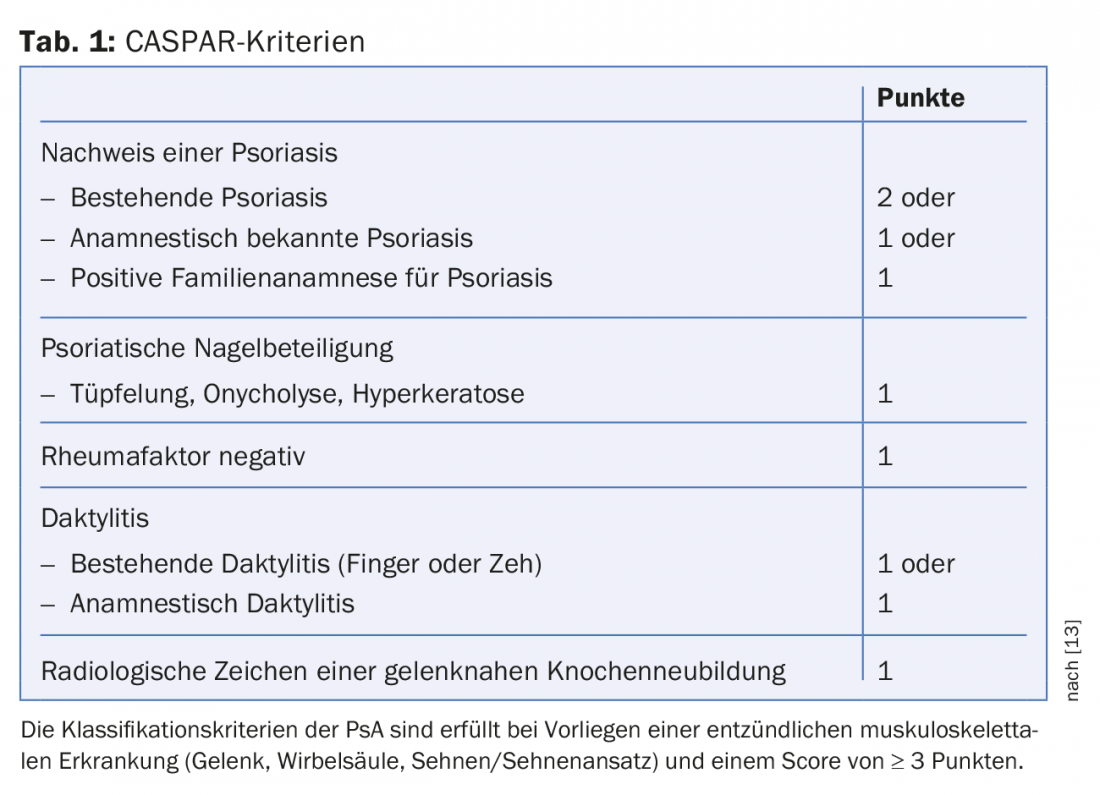
If the clinic is typical, serology is not required because it is important to treat whether the serology is positive or negative. In 60%, erythema migrans is typical. In atypical findings, which are relatively common, or in multiple erythema migrantia, which are relatively rare (in 5-20%), serology should be performed to confirm the diagnosis or to find another differential diagnosis (e.g., erysipelas, dermatomycosis). The diagnosis of erythema migrans is summarized in Table 1. PCR or culture are indicated as complex and expensive investigations in atypical clinic and serologically negative patients, furthermore in patients with immunosuppression.
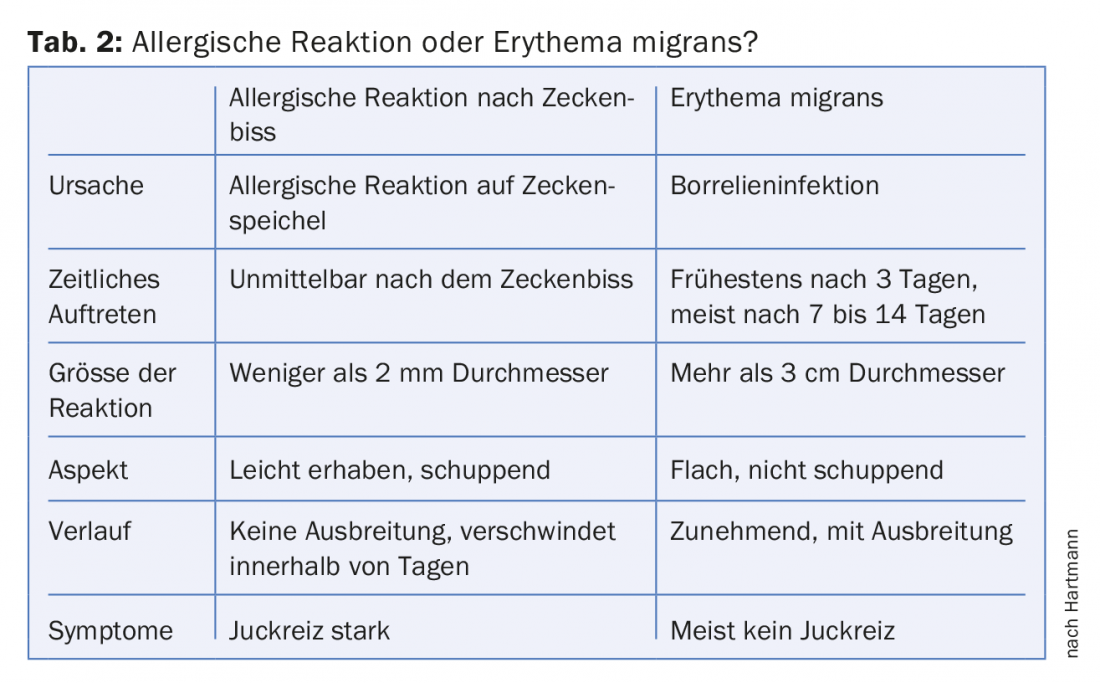
Borrelia lymphocytoma (lymphadenosis cutis benigna) is less common than erythema migrans and is most common in children on the earlobe. Livid brownish nodules appear weeks to months after infection and may persist for months. Lymphocytoma is most commonly caused by Borrelia afzelii. Allergic reactions to the saliva of ticks also occur after tick bites. These skin reactions appear shortly after the tick bite, do not spread, and are very itchy (Table 2).
Practical aspects of borrelia serology
Borrelia antibodies are commonly found in the population. Seroprevalence increases with age and is dependent on exposure risk. In Switzerland, it is 10% among blood donors, 26% among orienteers and 35% among forest workers. The immune response to Borrelia varies greatly from individual to individual. In the first weeks the serology is still negative. Specific IgM antibodies appear in serum about two to three weeks after infection, IgG antibodies about four to six weeks after infection. There is no difference between active infection and seropositive patients. Thus, a positive serology does not mean that the patient has Lyme disease. Serological control is not possible and not necessary. Serologic response to therapy varies greatly among individuals and is usually very slow. A positive serology as a laboratory diagnosis has no therapeutic consequences without a corresponding clinic, the speaker emphasized. Isolated positive IgM antibodies often represent a false positive result. Positive IgM antibodies without clinical symptoms are therefore not an indication for therapy. The antibodies do not protect against reinfection. Early therapy of erythema migrans can prevent seroconversion. Prophylactic therapy immediately after a tick bite is not worthwhile because of the low risk of infection and disease, the speaker said. Positive for Borrelia are 20% of adult ticks, 10% of nymphs and 1% of larvae, he said.
Serology is positive in late infections, which are usually caused by Borrelia afzelii, and usually poses no problems. In late Lyme disease of the skin, reticular livid erythema and infiltrates may form unilaterally or symmetrically on the extremities or face. There may be increasing atrophy with hair loss (acrodermatitis chronica atrophicans) or fibroid nodules on the elbows or knees.
Source: Key Lecture 3 “Borrelia: Diagnostics in Practice”, lecture by Martin Hartmann, Heidelberg, 99th Annual Meeting of the SGDV, Bern, September 8, 2017.
Literature:
- Cutaneous Lyme disease. Guideline of the German Dermatological Society, 2016, www.awmf.org
DERMATOLOGIE PRAXIS 2017; 27(5): 40-41











