In a late stage of the disease, there may be detachment and expulsion of a piece of bone-cartilage (dissekat or articular mouse) from its bearing (mouse bed) into the joint space. This leads to painful entrapment and joint blockage. For diagnosis, magnetic resonance imaging (MRI) is the most reliable. Therapy is initially conservative, with surgical intervention required in later stages.
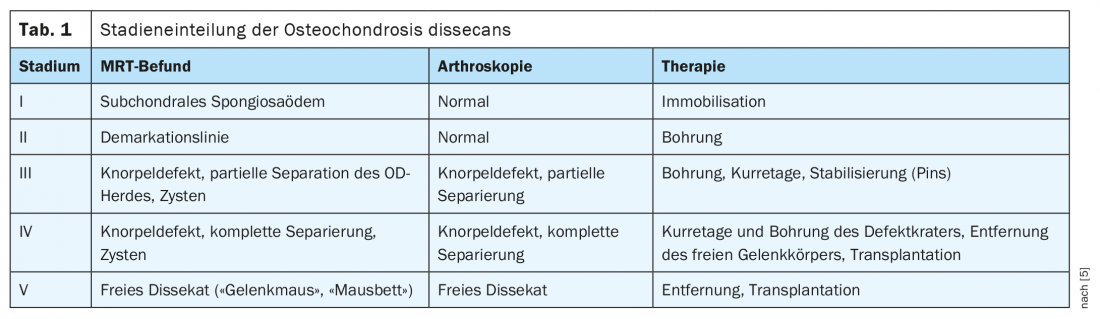
HAUSARZT PRAXIS 3/2021 reported on osteochondrosis dissecans (OD) of the knee joint. In the area of the ankle joint, the clinical picture is also determined by fragmentation of articular cartilage together with subchondral bone. The classification of OD into five stages (currently according to Kramer, 1992), as we know it from the knee joint (Tab. 1) and which can be verified very well by magnetic resonance imaging [1,3,5] also has its validity in this joint area and should be mentioned again because of the therapeutic relevance. The earlier classifications of Berndt and Harty 1959, elaborated by cadaveric studies or according to Dipaola (following arthroscopy) of 1991 are no longer relevant in radiological diagnostics.
The symptoms of an osteochondral lesion or osteochondrosis dissecans of the upper ankle joint (OSG) are often clinically ambiguous. The symptoms often resemble a sprain or distortion of the ankle joint: stiffness, swelling and ankle pain are then clinically superficial. Patients, often young, complain of pain deep in the upper ankle. This pain intensifies after exercise and then leads to unloading claudication [4]. Some of the patients also report a feeling of tightness or pain at rest inside the ankle. Only rarely are there clearly definable pains, blockages or a “cracking” sensation in the upper ankle joint.
For a definitive diagnosis, an imaging examination must usually complement the clinical findings. Not all osteochondral lesions or cases of osteochondrosis dissecans result in symptoms. In some cases, osteochondral diseases are discovered only as incidental findings. Until the dissect is rejected, pain is minor and clinical symptoms are uncharacteristic. Synovitis triggered by cartilage degradation can lead to swelling and joint effusions in the ankle joint and also result in joint pain. Typical late symptoms of osteochondrosis dissecans in the ankle joint are sudden and changing symptoms of entrapment up to joint locking. The disease can also lead to instability of the ankle joint.
Overview 1 summarizes image morphologic and clinical aspects of osteochondrosis dissecans of the ankle. In the case of fresh trauma, an osteochondral fracture should be considered as a differential diagnosis. Both the medical history, the clinical examination and the evidence of further damage, for example ligamentary damage, are diagnostically helpful. MRI is then diagnostically more advanced.

As with the knee joint, radiographs are useful only in late changes of OD with visualization of “mouse bed” or “joint mouse,” but can exclude other osseous changes.
Computed tomographic examinations , as in other joints, can detect free OD foci and reliably localize calcium- and bone-dense corpora libera, including bony defects. However, in detecting free intra-articular cartilaginous fragments, the method is clearly inferior to MRI.
Magnetic resonance imaging is very good at determining the different stages of OD (Fig. 2 to 6), as well as the localization and extent, stability and vitality of the subchondral fragment. Follow-up during or after completed therapy is again the domain of magnetic resonance imaging. Intravenous contrast application can reliably verify the vitality of bony structures and concomitant inflammatory intra-articular changes.
Case studies
In case report 1 (Fig. 1A and B), a 23-year-old patient with load-dependent pain and swelling of the joint shows OD stage II of the medial portions of the trochlea tali, locally in sagittal section also an initial flattening of the trochlea. Stage III OD after initial relief (initial stage I, 16-year course, multiple surgeries) in case 2 in a now 62-year-old man ultimately led to joint prosthesis, which was not assessable on MRI because of severe metal artifacts (Fig. 2A and B). For comparison in case report 3 after joint prosthesis of the upper ankle no artifacts in the X-ray. This was preceded by several years of significant osteoarthritis in a 66-year-old man with a distal tibial fracture and capsular ligament ruptures, inflammatory activation with subluxation of the joint components (without evidence of OD on clinical suspicion) and marked capsular ligament edema and initial osteonecrosis in the OSG (Fig. 3A to C).


Case report 4 shows the bony defect in an MS-CT (Fig. 4) of a 17-year-old with stage II OD (confirmed in out-of-hospital MRI).

Take-Home Messages
- The upper ankle joint is one of the main sites of manifestation of osteochondrosis dissecans.
- Imaging diagnostics of choice is magnetic resonance imaging.
- The symptoms depend on the stage and can lead to recurrent joint blockages, severe pain and swelling due to effusion, as well as limited load-bearing capacity of the joint.
- Traumatic joint damage must be differentiated on the basis of anamnesis, clinical findings and image morphology.
- Treatment of OD is conservative in the initial stage and surgical at the latest when a completely isolated or luxated osteochondral fragment is formed.
- MRI is also the gold standard for posttherapeutic controls.
Literature:
- Breitenseher M: The MR trainer. Lower extremity. Georg Thieme Verlag: Stuttgart, New York 2003, 88.
- Burgener FA, Meyers SP, Tan RK, Zaunbauer W: Differential diagnosis in MRI. Georg Thieme Verlag: Stuttgart, New York 2002, 407.
- Reiser M, Nägele M. (Eds.): Current joint diagnostics. Georg Thieme Verlag: Stuttgart, New York 1992, 39-42.
- https://gelenk-klinik.de/sprunggelenk/osteochondrosis-dissecans.html, (last accessed 03/15/2021)
- Thiel H-J: From symptom to diagnosis: joint diagnostics: osteochondrosis dissecans of the knee joint. HAUSARZT PRAXIS 2021; 3: 35-37.
HAUSARZT PRAXIS 2021; 16(4): 36-38












