Developments in the field of dermatological lasers are very dynamic with a large number of newly launched systems. The how to of an implementation of laser interventions requires training, alignment and equipment with the goal of perfect execution. The main indication areas are laser epilation, ablative laser systems, vascular and pigment lasers. A corresponding detailed weighting of published evidence is available. Those who can laser have more fun in dermatology, provided that the marginal conditions are carefully observed and evaluated again and again.
First things first – almost any dermatological laser intervention can be replaced by other methods. In addition, lasers are dangerous, expensive, difficult to operate and require a high degree of manual dexterity.
However, laser intervention often offers the more precise, faster, more aesthetic and more elegant therapeutic approach. If you want this, you should definitely read on. Those who can laser have more fun in dermatology. Assuming good and complete training, nothing stands in the way of implementing the lasers into the individual’s daily practice routine. Which additional things have to be considered and which indication areas can be easily developed will be explained in the following.
Training, alignment, equipment, selection and execution
There is no question that the beginner, on the basis of good training, the existing and or desired orientation of the practice or clinic, must assemble his equipment so that, with skillful selection of perfectly executed indications, laser therapy works in his own hands from the very beginning. With such an established concept, the spectrum of indications and interventions can later be expanded.
The need for constraint at the outset arises not only from the usually finite economic resources and the individual supply profile but also from the complexity of the systems. The care profile or else the potential patient volume that is being considered for a specific laser therapy, in addition to soft criteria such as acquisition costs, etc., usually determines the first laser that can be introduced. Once the first step is taken, the laser practice can be developed successively on a cold acquisition basis. The following is a discussion of the options that make sense for a laser practice that is starting up.
Important indications that can be excellently treated with lasers are vessels [1], pigments, hair [2] as well as the very diverse ablative and fractional ablative procedures [3]. Which of the indications can be primarily addressed is therefore decided by the level of training, the patient volume and the announced strategic orientation.
In addition to the laser devices, a number of pieces of equipment and standard operational procedures (SOP) are required for lasing, which make practical life easier and are very important in terms of safeguarding against potential risks. This includes good photo documentation, which the patient can use to understand the changes and actively involve himself in the decision to continue therapy. The new possibilities of 3D photography also allow the simulation of therapeutic effects. Photo documentation is essential in cases of dispute. In addition to the obligatory photo documentation, the so-called SOP also includes the special reconnaissance, which must be carried out at least 24 hours in advance. The education includes all standard items of laser therapy as well as potential complications, side effects and risks related to the accompanying anesthesia and aftercare, if applicable. It is essential to inform the patient about alternatives to the planned laser therapy. Furthermore, the contractual bases must be observed. Last but not least, ensure that all systems are maintained and that any STK are documented and available. Once the uniform requirements for laser therapy have been met, the individual risks must be assessed and, if necessary, accompanying protective measures tailored to the anticipated procedure must be introduced. In particular, the potential possibility of scarring in association with post-operative superinfection or triggering of an HSV outbreak, e.g., with fractional lasering, should be discussed and the need for close monitoring and, if necessary, antibiotic and antiviral shielding inferred. This is especially true for patients with a history of recurrent herpetic or bacterial infections, chronic inflammatory skin lesions or pathological scars. If there is an increased risk of postinflammatory hyperpigmentation when treating patients with darker skin types or for other reasons, special precautions should be taken. Removal of tattoos, on the other hand, requires special items in the clarification: color change, incomplete removal, allergic reactions up to anaphylaxis, and many others. In the case of laser epilation, it should be noted that it is almost impossible to achieve permanent epilation and there may also be a risk of paradoxical hair growth if certain conditions are present.
Once these points have also been clarified, the best possible eye protection, respiratory protection if necessary, should be clarified by staff and patient, and the pain management required for the patient should be determined.

Epilation
With the exception of the hair on the head, the last hairy remnants of man have been removed for thousands of years using increasingly sophisticated methods. Professional laser epilation has a special significance among the abundance of available methods due to the achievable efficiency and elegance, which is why it has been listed among the most frequent interventions in international registries for years.
Numerous systems based on a few concepts are available. For the beginner, the decision to use a hair removal laser is significant because after a usually short and steep learning curve, this indication is safe to offer. The advantage of professional systems over so-called home-devices is the efficiency due to much higher performance of the devices. Passing responsibility to less trained personnel is common practice but fraught with danger, as laser epilation is disproportionately associated with complications in lay hands [4–7] (Table 1) .
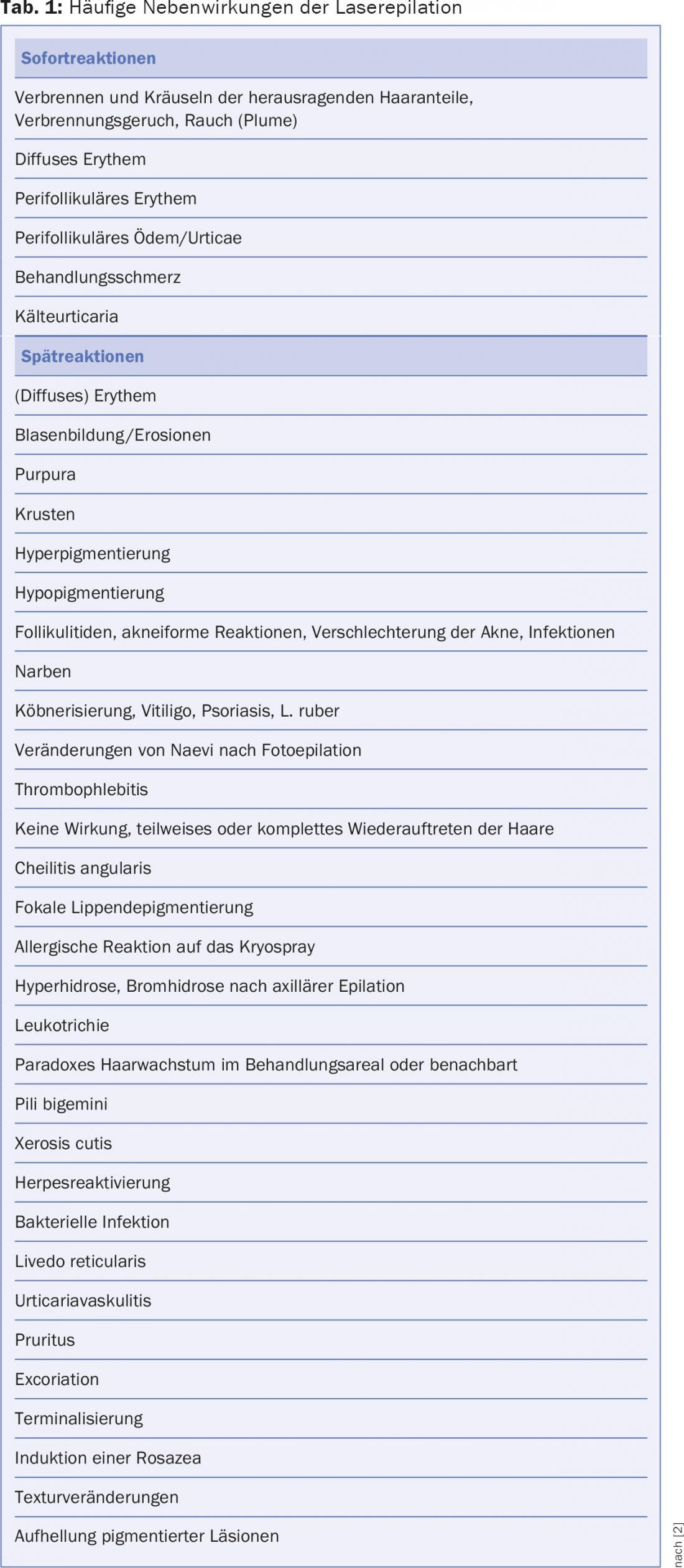
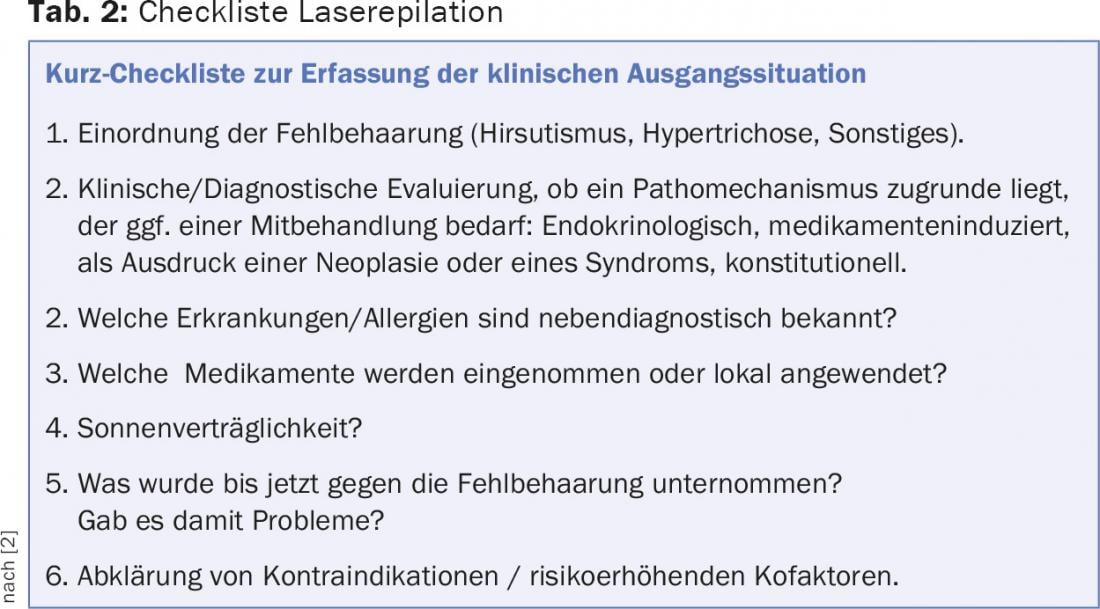
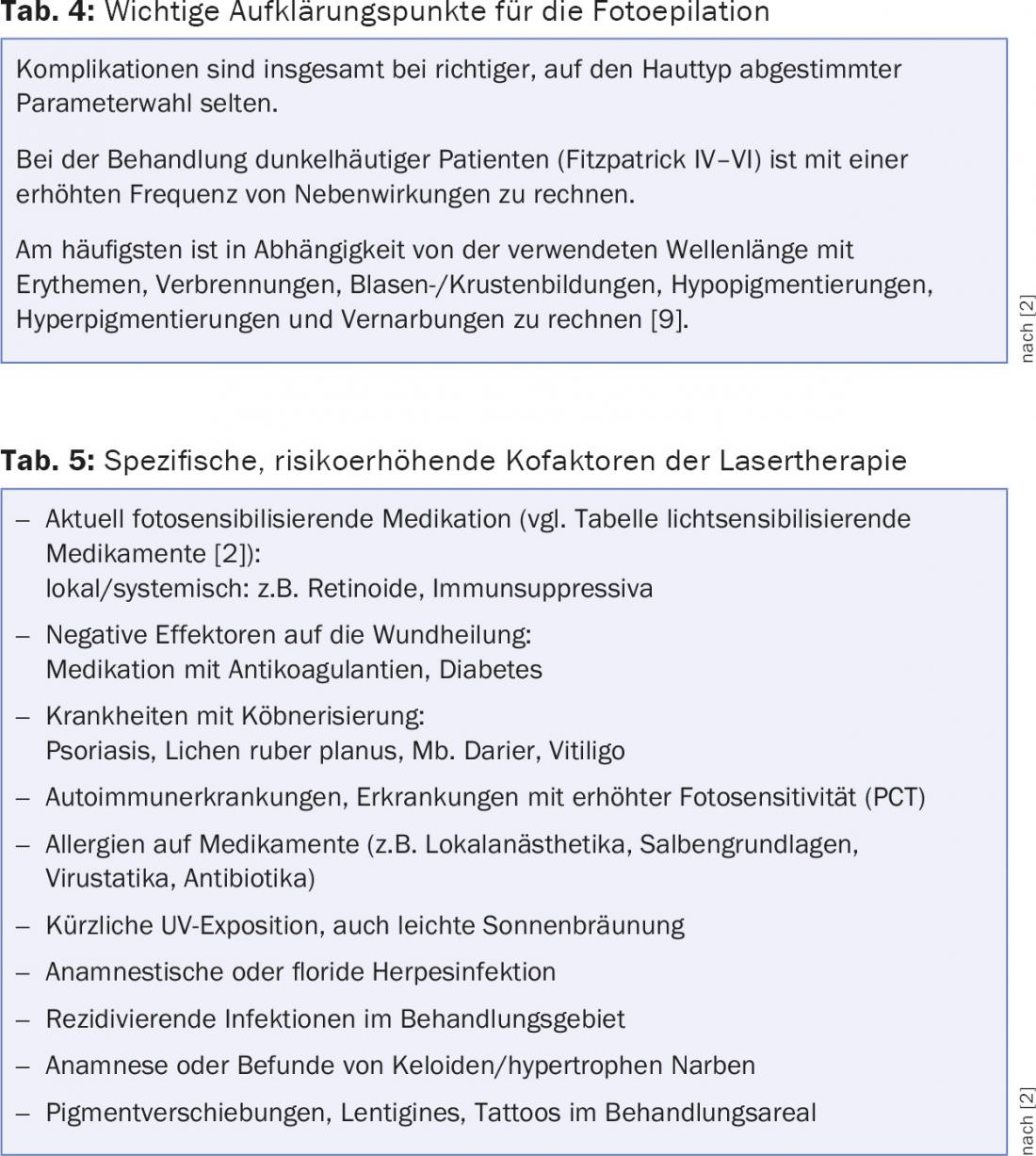
It is always advisable to work through checklists [8] during laser treatment (Tab. 2), so that, in view of the large number of known side effects, some of which are frequent, complications and, above all, interaction with concomitant medications are not risked (Tab. 3). Most commonly, depending on the wavelength used, erythema, burns, blistering/crusting, hypopigmentation, hyperpigmentation, and scarring are to be expected (Tab. 4) [9]. Therefore, the specific risk-increasing cofactors should be known and taken into account (Table 5) [2].

Ablative, incisional and ablative fractional lasers
A prerequisite for the successful use of ablative, incisional, and fractional lasers is adequate patient selection and focus on an appropriate indication. As with all other types of lasers, it is of particular importance not to overlook malignant conditions and to always refer such for dermatohistopathological evaluation. In addition to dermoscopy, in vivo confocal microscopy and optical coherence tomography, along with impedance measurement techniques, open many new fields for the classification of clinically ambiguous findings. You are definitely doomed to failure if the indication is wrong. Two principal classes of equipment are available, in addition to niche systems. While the Er.YAG laser is easier for the beginner to learn, in the long run aCO2 laser can be used in a wider spectrum. Today, both systems are capable of all common forms of application (cutting, point ablations, scanned ablations, fractionated ablations) and are offered by various companies. It is necessary to evaluate the systems in detail to find the most suitable system for individual cutting. It is important to note that with increasing use, practical experience accumulates and this quickly releases desires for better devices. So you should not think too short.
In particular, fractional ablative lasers have opened up numerous new indications. Thus, scars up to keloids, in limits vessels, pigments and the chronically light-damaged skin can be treated. The ablative fractional laser-assisted application of topical agents has gained special importance. With the help of fractional ablative lasers, the efficiency of PDT in the treatment of actinic keratoses can be increased to the point of field carcinization. However, there are clear limitations in the treatment of infiltrative malignant non-pigmented tumors such as basal cell carcinoma and squamous cell carcinoma. These tumors should be excised according to guidelines. No value is placed on these lasers for non-benign pigmented changes.
The somewhat less versatile fractional non-ablative lasers are to be distinguished. Such systems emit in the near-infrared range and cause tissue coagulation. Consequently, like other coagulating systems, they are used wherever heating is required rather than ablation. This is especially true for the treatment of wrinkles but also of redness, scars, acne scars and pigmentation within certain limits.
Vessels
Unwanted vessel therapy has historically been one of the most common indications that can be gratefully treated with lasers if craftsmanship is present along with solid training, good systems are purchased, and the required SOP is implemented [10]. The choice of system is not particularly easy, as there is a certain demand in the variability of cutaneous human vessels. Unfortunately, it is still not possible to treat all indications satisfactorily with a universal system. For this reason, the professional always resorts to several highly specialized systems. For the beginner, a 532 nm long-pulsed system is definitely recommended, which is referred to as a KTP (potassium tetanyl phosphate) or LBO (lithium borate) laser with regard to the underlying technology. Unfortunately, only telangiectasias and small haemangiomas can be treated very well with these systems. For larger vessel calibers such as spider veins and large haemangiomas as well as vascular malformations, for example, long-pulsed 1064 nm Nd:YAG lasers are needed. If N. flammei are to be treated, a pulsed dye laser is the first choice. The latter can also be used for areal redness when the vessels are too small to use a 532 nm laser.
Pigment removal
Pigment removal is another important pillar of laser therapy. While discrete epidermal or dermal localized pigments in the skin are very small and therefore necessarily treated according to the concept of selective photothermolysis using extremely short pulses (q-switched systems emitting in the ns range or ps range), the pigment bound in the hair is best addressed with pulses in the range of ms. A distinction must also be made between the addressing of endogenous pigments (phaeo- and eumelanin) and exogenous pigments. Therefore, it is malpractice when pigments of e.g. tattoos are treated with long-pulsed (ms pulses) lasers or flash lamps and other radiation sources. Complications such as burns, blistering and scarring usually result.
Of the multitude of conditions that lead to endogenous hyperpigmentation in various skin layers, only a few are found to respond excellently to laser therapy. The published evidence indicates a first line recommendation (level A, > 212 publications for qs ns laser) for e.g. Lentigines, N. Ota, N. Ito, Horis nevus, and Mongolian spots. In contrast, cafe au lait spots, seborrheic keratoses, congenital and epidermal nevi, N. Becker, and melasma are classified as variable response. Absolute restraint is recommended in the treatment of pigmented nevi for the above reasons. Any clinically suspicious or clearly non-benign pigmented lesion should be excised and submitted for dermatohistopathological evaluation.
Tattoo removal using qs laser is a widely practiced practice. Concerns include the need for numerous sessions, the risk of incomplete removal, color change, allergic reactions and even anaphylaxis. It is also important to know that the response of highly variable tattoo colors is wavelength-dependent. Consequently, a system that covers several wavelengths is recommended. This also makes sense because greater penetration depths can be achieved with higher wavelengths.
The data available to date on the recently introduced ps lasers is still incomplete. Initial reports indicate that the number of treatments required is decreasing. The final evaluation remains to be seen.
Summary
Developments in the field of dermatological lasers in recent years have shown that new wavelengths, concepts and combinations can be used to cover numerous indication areas, therapeutic options and aesthetic indications.
The how to of successful implementation of laser interventions in the therapeutic armamentarium requires specific training, conceptual orientation and acquisition of appropriate equipment matched to indication selection to become perfect in execution. The main indication areas of interest to the novice include laser epilation, ablative, incisional and fractional ablative laser systems, vascular removal, and pigment removal of endogenous and exogenous origin. For each of these core indications, there are a variety of specific systems with equally specific technical features. A detailed orientation can be found in addition to the weighting of published evidence in the indication-corresponding textbooks. In addition, there are numerous systems for special indications, which the beginner will be able to discover for himself after a successful start.
Those who can laser have more fun in dermatology, provided that the boundary conditions are carefully observed and evaluated again and again. The development of laser dermatology is not finished and there is no end in sight. This opens up a unique therapeutic future for the laser specialist of tomorrow.
Literature:
- Grunewald S, et al: 2012. vascular laser. KVM, Berlin.
- Bodendorf M.O., et al.: 2013. epilation laser. KVM, Berlin.
- Paasch U., et al.: 2011. dermatological laser therapy: fractional lasers. KVM Verlag, Berlin.
- Zelickson Z, et al: Complications in cosmetic laser surgery: a review of 494 Food and Drug Administration Manufacturer and User Facility Device Experience Reports. Dermatol. Surg. 2014; 40: 378-382.
- Hussain M, et al: Laser-assisted hair removal in Asian skin: efficacy, complications, and the effect of single versus multiple treatments. Dermatol. Surg. 2003; 29: 249-254.
- Goldberg D: Laser complications: hair removal. J. Cosmet. Laser Ther. 2006; 8: 197-202.
- Vano-Galvan S, et al: Complications of nonphysician-supervised laser hair removal: case report and literature review. Can. Fam. Physician. 2009; 55: 50-52.
- Hammes S, et al: [Side effects and complications of therapy with laser and intense light sources]. Dermatologist. 2013; 64: 145-154.
- Breadon JY, et al: Comparison of adverse events of laser and light-assisted hair removal systems in skin types IV-VI. J. Drugs Dermatol. 2007; 6: 40-46.
- Thaysen-Petersen D, et al: Side effects from intense pulsed light: Importance of skin pigmentation, fluence level and ultraviolet radiation-A randomized controlled trial. Lasers Surg. Med. 2016.
DERMATOLOGIE PRAXIS 2016; 26(5): 24-28











