The success of scar treatment depends on various factors. There is still no universally valid gold standard. An approach based on individual circumstances has proven successful. Depending on the type of scar, different procedures can be used. Laser therapy can be used for many indications and can be combined with “laser-assisted drug delivery” and other methods.
Scars are the permanent remaining sign of deeper injuries of the skin and are formed in the course of physiological wound healing. The management of scars was one of the main topics of the advanced training course “Inflammation and Wound Healing” of the University Hospital Zurich in collaboration with “Skintegrity”, an association of researchers and clinicians for the improvement of wound healing with the participation of ETH Zurich. Laurence Imhof, MD, Medical Director Physical Therapies and Aesthetic Dermatology, Dermatology Clinic, University Hospital Zurich [1], spoke on the current state of scar treatment.
Individual and interdisciplinary approach to therapy
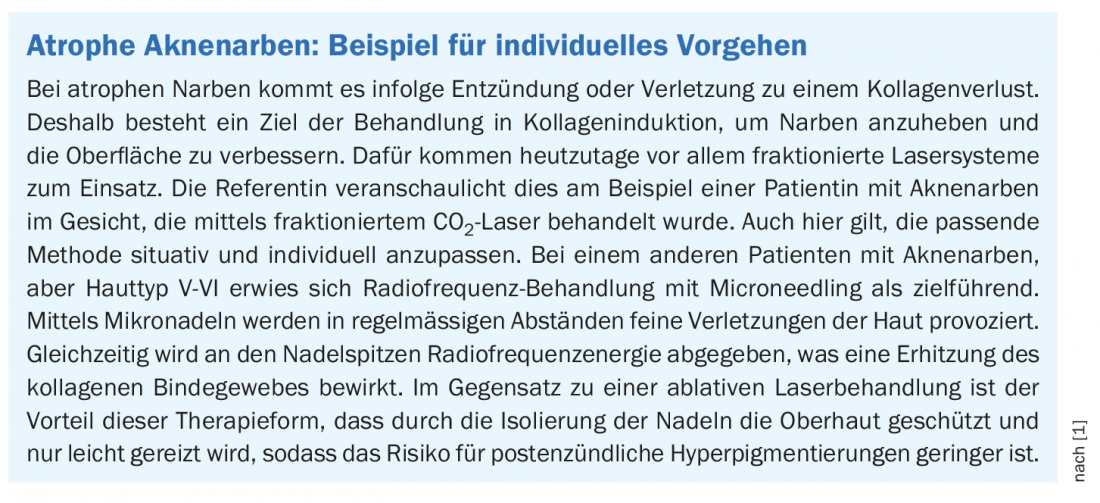
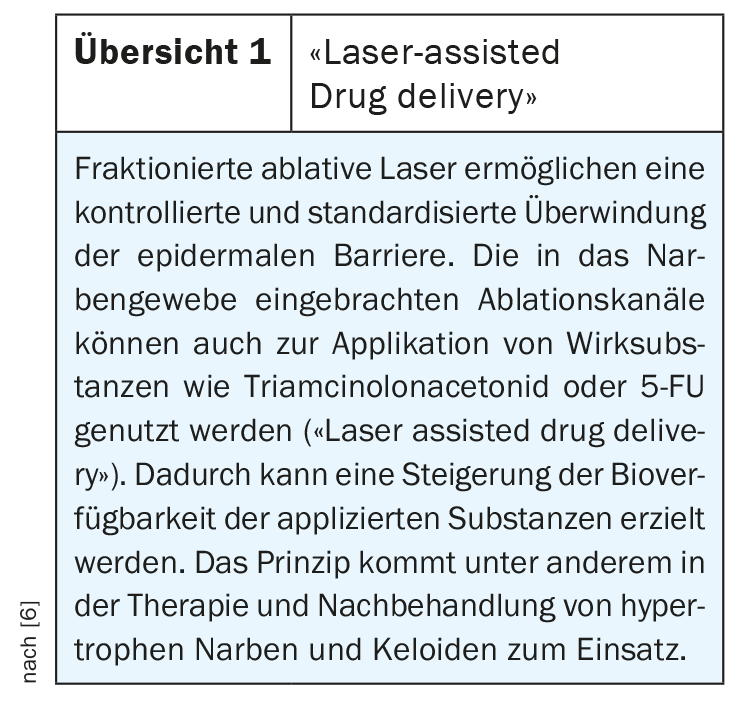
Depending on individual disposition, localization, cause and healing process, pathological scars may occur as a result of pathologically altered wound healing with consecutive increased formation of scar tissue. Hypertrophic scars and keloids in particular are often associated with itching, pain, and functional limitations, so treatment is usually medically indicated. “Look at each scar individually and treat it accordingly,” is a key message from Dr. Imhof [1]. “The optimal therapy often consists of a combination of different therapeutic approaches,” the speaker elaborates. There are several international consensus-based treatment recommendations on which to base [2,3]. Among others, an update of the s2k guideline on the therapy of pathological scars under the auspices of the German Dermatological Society (DDG) was published last year [4]. Fractional ablative and non-ablative lasers are among the most advanced laser technologies in the field of scar treatment. The fractional laser technique is characterized by the fact that vital tissue remains between each ablation zone, which ensures the specific effectiveness of the procedure with a low rate of side effects. The mechanism of action is mainly to induce thermal microlesions in the scar tissue. In the course of healing, the skin tissue becomes almost normotrophic. This method can be combined with “laser-assisted drug delivery”, which allows the application of drugs that are difficult to insert into the skin (overview 1) [5].
Hypertrophic scars: with fractional laser to the target
A hypertrophic scar (Fig. 1) is defined as a reddish connective tissue proliferation that does not exceed the border of the original surgical or injury wound. Growth is usually accelerated in the first six weeks. Often, spontaneous involution occurs thereafter. “However, there are patients in whom this regression does not occur or is very delayed,” said Dr. Imhof [1]. If the wound remains hypertrophic and erythematous, silicone gels and corticosteroid injections are considered first-line treatments. For hypertrophic small scars, second-line vascular laser is used, combined with (ablative) fractional laser as appropriate. The aim of laser treatment is selective destruction of pathological capillary perfusion and reduction of vascularization with lightening and regression of fibrosis. Directly following fractionated laser therapy, triamcinolone or 5-fluorouracil (5-FU) can be applied by means of “laser-assisted drug delivery” (overview 1) .

“More problematic are extensive hypertrophic scars, for example after trauma or burns,” the speaker explained [1]. These cases are complex and often require a multimodal interdisciplinary approach. In addition to compression bandages and silicone overlays, occupational therapy, physiotherapy and plastic surgery measures are often used. However, laser medical methods have also proven successful. “What works very well, especially in burn scars, is the use of ablative fractional laser systems,” said Dr. Imhof, reporting on a patient who was treated in collaboration with the Department of Plastic Surgery [1]. After various interventions, including skin grafting and compression of the skin, patients underwent multiple facial treatments using a fractionalCO2 laser.
Keloid treatment remains a “challenge
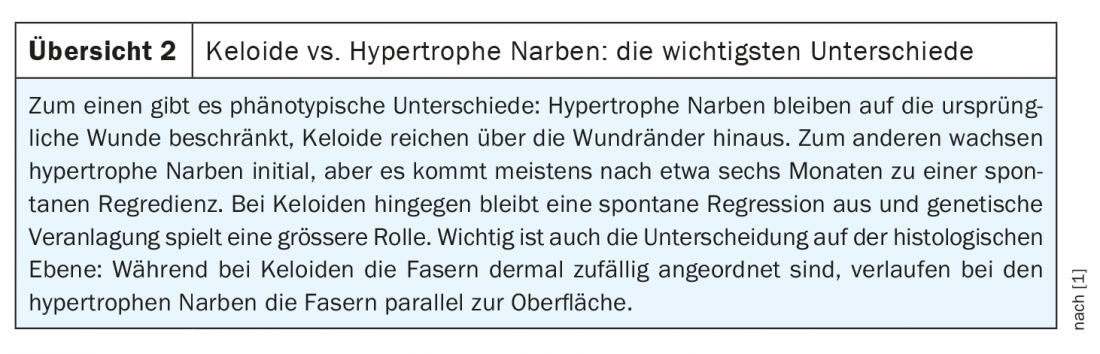
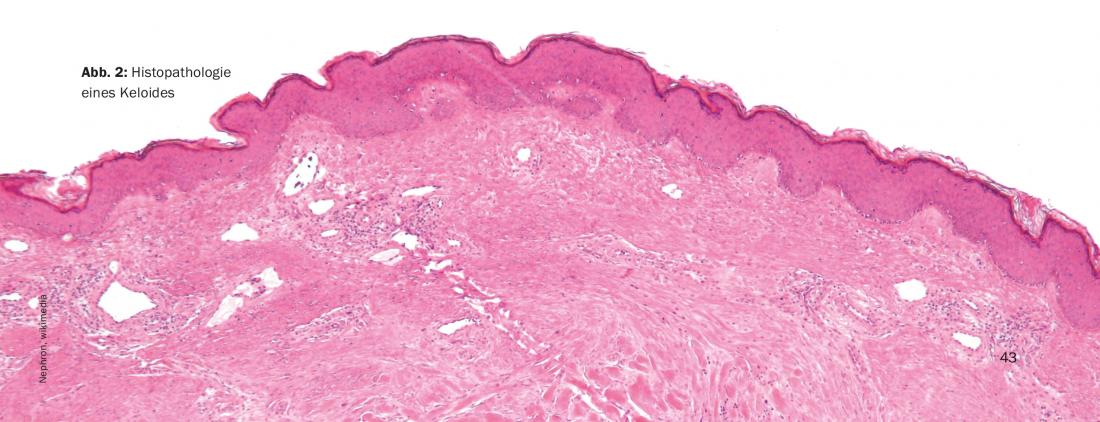
“Keloids continue to be a major challenge,” Dr. Imhof said. In contrast to hypertrophic scars, keloids are characterized by growth extending beyond the wound margins, and there are also some differences at the histologic level (overview 2, Fig. 2) . There is no recipe for success in the treatment of keloids. According to current guidelines, the following procedure is recommended [4]: For the treatment of small keloids, initially the use of triamcinolone acetonide (TAC) or cryotherapy, if necessary combined. If these methods are not effective, the guideline recommends a combination of TAC and cryosurgery plus 5-FU intralesional. Alternatively, excision followed by follow-up may be considered, with adjuvant follow-up required for recurrence prophylaxis. Postoperative radiotherapy can greatly reduce recurrences, and the mechanism of action is based on antiproliferative and anti-inflammatory effects. It is important that radiation is administered within 24 hours of the surgical procedure [1]. The use of dye laser or IPL is recommended for the treatment of erythematous changes.
Excision may be considered for larger narrow-based keloids, emphasizing the need for follow-up. Adjuvant measures following laser ablation or excision can be performed, for example, using triamcinolone or 5-FU. Low-dose radiotherapy and compression have also been shown to be effective. If keloids are large in area, a similar treatment as for small keloids is suggested, i.e., a combination of injections and (intra)lesional cryotherapy. Large keloids are often refractory to therapy and prone to recurrence. Therefore, the indication for excision should be well considered here, explains Dr. Imhof.
What to do about dyspigmentation and erythema?
For hyperpigmented post-inflammatory scars, the use of short-pulsed pigment-specific picosecond or nanosecond lasers, such as Q-switched Ruby laser, has proven effective. In most cases, a few sessions are sufficient. Depigmented or hypopigmented scars are more difficult to treat, Dr. Imhof says. There are rather few studies in this area, he said. One can try a fractionated laser followed by “laser-assisted drug delivery” of the prostaglandin bimatroprost (off-label).
If erythema persists for weeks or months after an injury, it may indicate the development of pathologic scarring. The lasers of choice for this indication are vascular lasers; the target is hemoglobin in the blood vessels. Teleangiectasia and dilated vessels in scars can be treated, for example, with a dye laser or a long-pulsed NdYAG laser (1064 nm). This has the side effect of flattening the hypertrophic scar tissue.
Congress: USZ Inflammation and Wound Healing
Literature:
- Imhof L: Scar treatment – current status. Dr. med. Laurence Imhof, Inflammation and Wound Healing, University Hospital Zurich, 18.03.2021
- Seago M, et al: Laser Treatment of Traumatic Scars and Contractures: 2020 International Consensus Recommendations. Lasers Surg Med 2020; 52(2): 96-116.
- Anderson RR, et al: Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol 2014; 150(2):187-193.
- Nast A, et al: S2k-Leitlinie Therapie pathologischer Narben (hypertrophic scars and keloids) – Update 2020. J Dtsch Dermatol Ges 2020, https://doi.org/10.1111/ddg.14279
- Wenande E, Anderson RR, Haedersdal M: Fundamentals of fractional laser-assisted drug delivery: An in-depth guide to experimental methodology and data interpretation. Adv Drug Deliv Rev 2020; 153: 169-184. doi: 10.1016/j.addr.2019.10.003. Epub 2019 Oct 16.
- Braun SA, et al: Laser assisted drug delivery: principles and practice. JDDG 2016; 14(5): 480-489.
DERMATOLOGIE PRAXIS 2021; 31(2): 42-43 (published 4/13/21, ahead of print).