In the acute treatment of cerebral stroke, in addition to lysis, treatment in a spatially defined stroke unit with an interdisciplinary, specialized team is an important factor in reducing mortality and morbidity. Within the stroke unit, interdisciplinary neurorehabilitative treatment is a critical component for optimal use of recovery potential and good long-term outcome. According to studies, an early start of therapy and a high intensity of therapy are decisive for long-term success. However, the ideal time should be determined individually after weighing the risks.
Acute stroke is the most common cause of disability in adults in industrialized countries. Currently, we assume 150 events per 100,000 inhabitants per year in Switzerland. In addition to the classic vascular risk factors, age is a relevant risk factor. For example, the risk of stroke increases markedly with age and is approximately 1000 events per 100,000 population per year for those over 85 years of age. In about 85% of those affected, the cerebral stroke is due to a circulatory disorder, and in about 15% there is a hemorrhage.
Treatment on the stroke unit
Acute treatment in a stroke unit initiated as soon as possible is a decisive advantage in reducing mortality and functional deficits in the early phase of stroke. By stroke unit we mean an infrastructural and personnel treatment unit. An interdisciplinary treatment team, consisting of therapists, nurses and medical stroke specialists, is responsible for the care of patients and maintains a continuous, close exchange. Based on a comprehensive treatment concept, there is the possibility of intravenous and/or intra-arterial lysis therapy, thrombectomy and neurosurgical decompression in the acute phase in the case of space-occupying ischemia or hemorrhage.
Indredavik et al. [1] were able to demonstrate the superiority of treatment in a stroke unit for ischemic cerebral infarction in a first randomized trial in 1991. In the Norwegian study, 110 patients with acute stroke were treated in a stroke unit and 110 in a general internal medicine department. Treatment differed only in the first six weeks, and follow-up assessments were made after six and after 52 weeks. The first evaluation at six weeks showed a significant survival benefit after treatment on a stroke unit. Thus, 17.3% of patients treated traditionally and 7.3% of patients cared for in the stroke unit died. Significantly more patients could be discharged home after treatment in the stroke unit and did not need to transfer to a nursing facility. This effect could also be demonstrated in the follow-up assessment after one year; however, at this point there was no longer a relevant difference with regard to survival: 24% of the patients died after care on the stroke unit vs. 32.7% after traditional treatment. The critical time window in terms of survival was the subacute phase (days 5-42). The cause of death was usually determined clinically. In the traditionally treated group, the cause of death was more frequently documented as pneumonia, acute pulmonary embolism, and a new stroke event.
Comprehensive, structured treatment concept
Therefore, after acute care, an intensive investigation of the cause is initiated in the stroke unit by means of vascular imaging, cardiac embolic source detection, and laboratory tests, and appropriate secondary prophylaxis with medication is established to minimize the risk of stroke recurrence.
Essential are good control of blood pressure, blood sugar, and prophylaxis and treatment of infections, especially pneumonia. Infections pose a significant risk of mortality and are a consequence of both immobilization and lack of protective reflexes due to brain injury with increased risk of aspiration. Infections are also thought to be favored as a result of overactivity of the sympathetic nervous system, triggered by poorer immunological control after a major cerebral infarction [2].
Swallowing assessment and individual swallowing training by a specialized speech therapy team is indispensable for the prophylaxis of aspiration and the associated increased risk of pneumonia. The appropriate dietary form and composition of the food is coordinated with nutritional counseling specialists.
In 2007, a large meta-analysis of observational studies confirmed the survival benefit after stroke unit treatment in the “real world”. This benefit was largely due to less frequent pulmonary infections and a lower number of stroke recurrences and stroke progression compared with conventional treatment [3].
According to a 2011 study, treatment in a stroke unit seems to be even more effective with a trend toward better functional outcome when discharge and rehabilitative measures were accompanied by a specialized team [4].
Early rehabilitation within the stroke unit
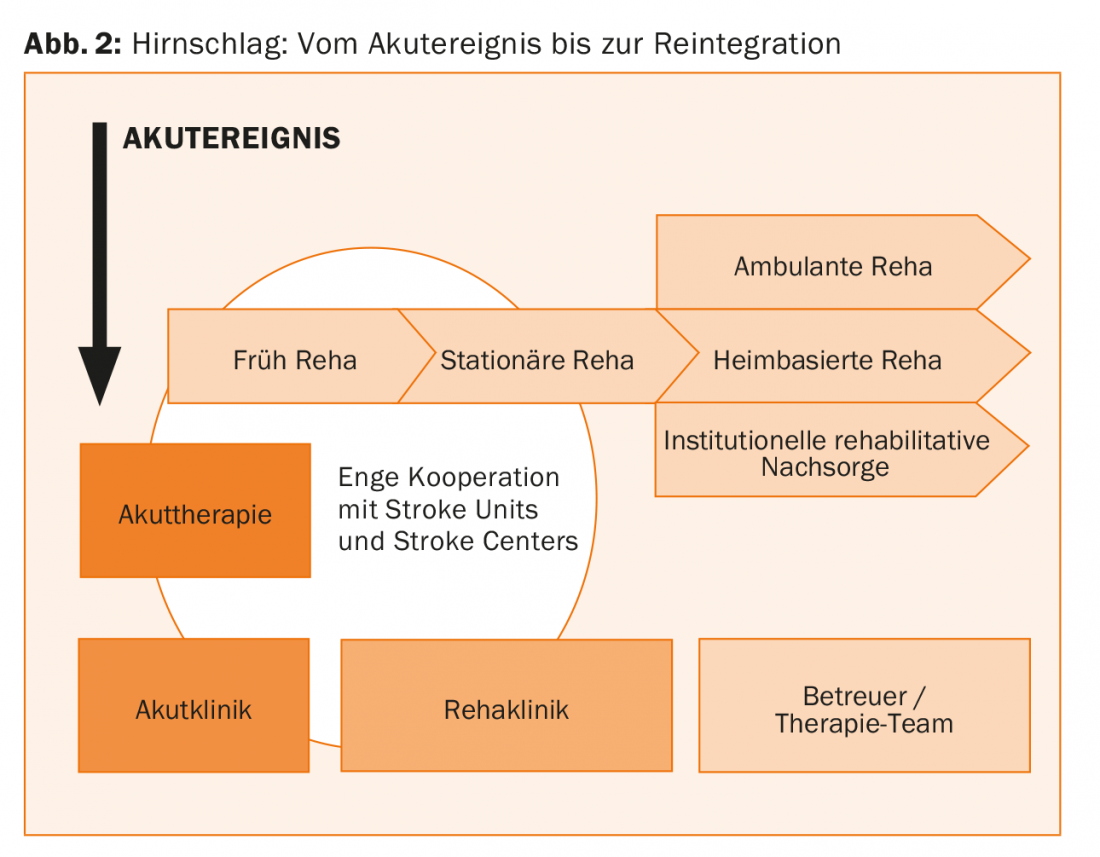
A key factor in the success of stroke units is the early start of rehabilitation after a function-based structured assessment, based on an interdisciplinary treatment concept by physiotherapists, occupational therapists and speech therapists. Early-onset rehabilitation aims to minimize the effects of organ damage, promote recovery, and prevent secondary complications. An initial education regarding lifestyle adjustment with the aim of reducing the risk of cerebrovascular events in the future is part of the care concept; intensified training and support in implementation, such as nicotine cessation, follow during inpatient or outpatient rehabilitation treatment. Regular rounds on the stroke units are accompanied by a rehabilitation physician from an associated stroke rehabilitation facility. This helps to set priorities within the multimodal therapy concept already in the acute phase and to assess the rehabilitation potential. In addition, personal contact can be established with the patient, thus creating a good basis for a rehabilitation stay that is individually tailored to the patient.
What is the impact of early rehabilitation?
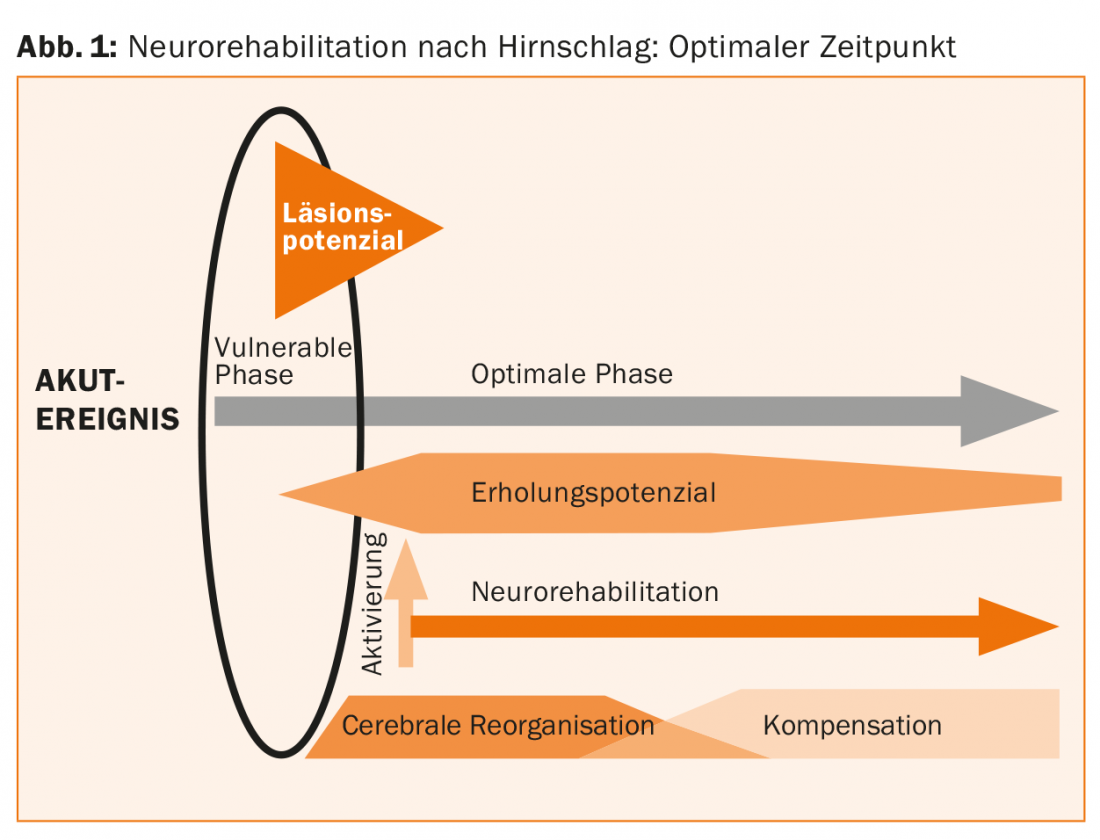
The goal of subsequent neurorehabilitation is to support functional recovery and, in the case of insufficient functional recovery, to promote compensatory and adaptive mechanisms.
Recovery of neuronal function is achieved by activating inactive or associated cerebral networks with the goal of performing movement and using it for activities in the same way as was possible before the stroke; the original body parts can be used in an unchanged way to accomplish a task. Adaptive compensation mechanisms lead at the neuronal level to the activation of brain areas that are not normally engaged for function. Thus, a movement can succeed again by activating new movement patterns and tasks can be accomplished by using other body parts and effectors. Unfortunately, adaptive movement patterns are usually uneconomical, which can lead to particularly severe fatigability.
In a study of treatment in a stroke unit with integrated early rehabilitation, early mobilization followed by good diastolic blood pressure control was a significant associated factor for the possibility of discharge home. With the early start of neurorehabilitative measures, improved connectivity through activation of intracellular signaling proteins and neurotransmitters within three weeks after stroke has also been documented in animal experiments.
Early rehabilitation measures promote recovery and counteract “learned non-use”. They prevent infection complications and orthostasis tendency and prevent deconditioning. Potential risks of early mobilization include deterioration of perfusion in the zone around the infarct core, an area where cerebral autoregulation of blood flow is impaired. In patients with stenoses of the extracranial and intracranial vessels supplying the brain with scarce perfusion reserve, early mobilization may also lead to relevantly worse perfusion. In addition, a possible expansion of the damaged area during early activation due to an excess of excitatory neurotransmitters in animal experiments is discussed [5].
For example, a large randomized trial of very early mobilization (within 24 hours of stroke onset) showed no benefit in terms of functional recovery and no difference in immobility-related complications with comparable mortality at 3 months (7% usual therapy vs 8% very early mobilization). Among patients who died early, progressive stroke was detected more frequently in the very early treatment initiation group (n=31) than in the traditionally managed group (n=16) [6].
Because immobilization leads to higher complication rates and early initiation of rehabilitative measures has a positive effect on recovery and long-term outcomes, patients should be mobilized as early as possible after a cerebral stroke and begin adapted rehabilitation training. However, the ideal time should be determined individually after risk assessment [5].
Switzerland situation
With the establishment of 9 stroke centers and 14 stroke units with associated rehabilitation facilities, high-quality, nationwide care for stroke patients has been made possible in Switzerland. Thus, the close cooperation of acute and rehabilitation hospitals aims at optimally exploiting the recovery potential of stroke patients and promoting social reintegration (Figs. 1 and 2).
Only recently, a study conducted in Switzerland demonstrated the superiority of treatment success after three months in a spatially defined stroke unit with a specialized team compared with treatment in an intensive care unit followed by care by a stroke team without an infrastructural unit [7].
Acknowledgments: The author would like to thank Mr. Serafin Beer, Senior Physician, Clinic for Neurology and Neurorahabilitation, Valens, for valuable suggestions and review of the manuscript.
Literature:
- Indredavik B, et al: Benefit of a Stroke Unit. Stroke 1991; 22: 1026-1031.
- Meisel Ch, et al: Suppressing Immunosuppression after stroke. NEJM365; 22 December 1, 2011.
- Seenan P, et al: Stroke units in their natural habitat: systematic review of observational studies. Stroke 2007; 38: 1886-1892.
- Fjaertoft H, et al: Stroke unit care combined with early supported discharge improves 5-year outcome: a randomized controlled trial. Stroke Jun; 42(6): 1707-11.
- Beer S, et al: On behalf of the Swiss Society for Neurorehabilitation (SNRG) and the Neurorehabilitation Topic Group of the Cerebrovascular Working Group of Switzerland (ZAS) Neurorehabilitation after Brain Stroke. Switzerland. Medical Forum 2007; 7: 294-297.
- Bernhardt J, et al.: The AVERT Trial Collaboration group. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial.
- Cereda CW, et al: Beneficial effects of a semi-intensive stroke unit are beyond the monitor. Cerbrovasc Dis. 2015; 39(2): 102-9.
InFo NEUROLOGY & PSYCHIATRY 2017; 15(1): 12-15.