Eczema is the most common skin condition seen in family practice and is one of the typical symptoms of atopic dermatitis. A disturbed skin barrier is common to all eczemas and is favorably influenced by consistent basic therapy.
Characteristic of this chronic recurrent skin disease is very dry sensitive skin and itching of varying severity. The course of atopic dermatitis (also: neurodermatitis) is characterized by disease episodes of varying duration and severity. The clinical picture varies from individual to individual, depending on the stage (acute or interval), age, and other factors [1]. Predilection sites of atopic eczema in adults are the large flexures, although the skin lesions may also occur on other parts of the body (e.g., hands, face). In infants, the face, the scalp (“milk crust”) and the extensor sides of the limbs are mainly affected, while in children the eczema tends to appear on the flexor sides of the arms and legs and on the wrists and ankles. Approximately one third of those affected by atopic dermatitis in childhood also suffer from atopic eczema in adulthood. The causes are multifactorial. In addition to genetic predisposition, numerous triggering factors also play a role in the initial manifestation of the disease, and there are a large number of possible triggers for the occurrence of the disease episodes.
An important pillar of therapy in all phases
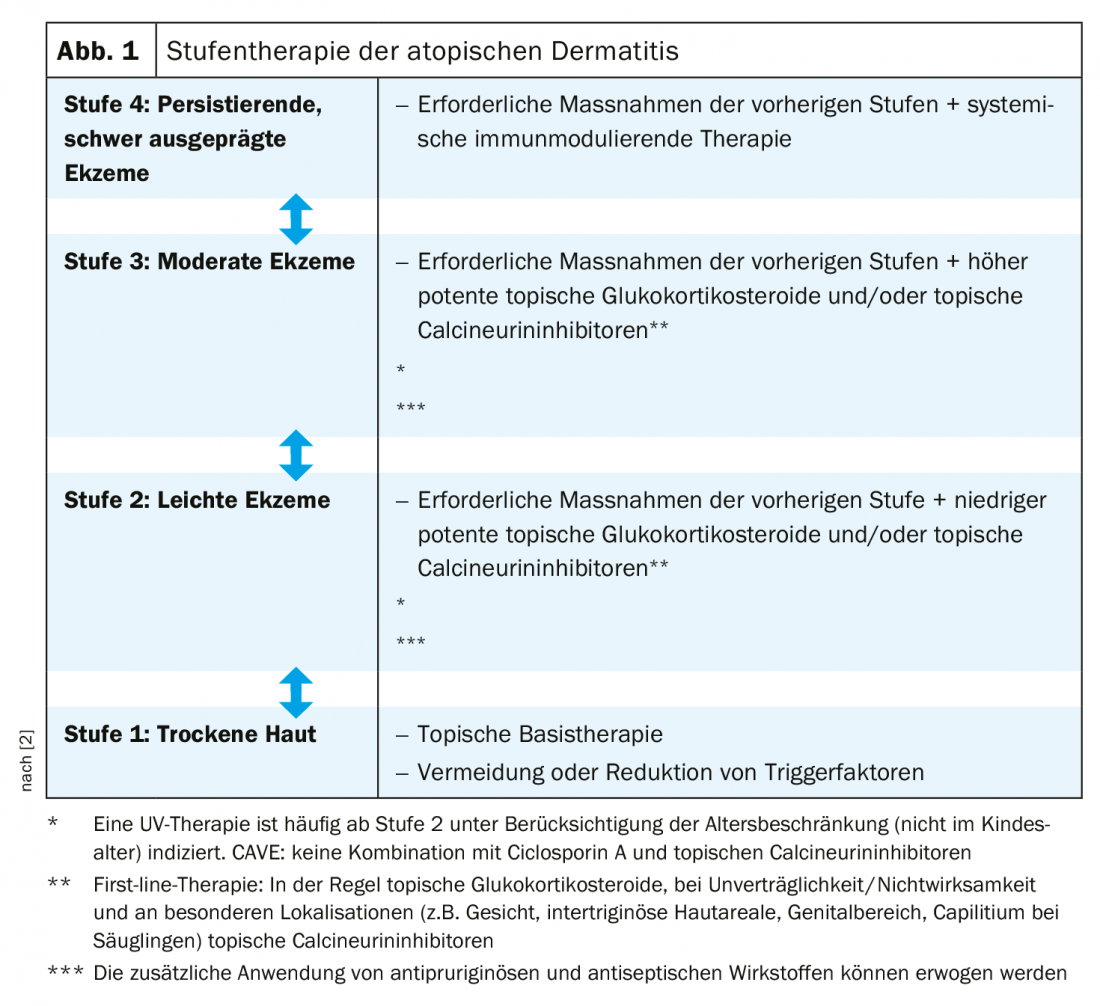
The treatment of atopic dermatitis remains a challenge. Therapy should be individually adapted to the different phases, severity and chronicity. Following international committees, the current AWMF guideline recommends a stepwise therapy (Fig. 1) [2]. This rough treatment regimen should be adjusted depending on the patient’s age, course, localization, and level of suffering. Basic therapy is a mainstay in the treatment of atopic dermatitis and is indicated at all stages regardless of disease severity [3]. Thus, consistent basic care plays a decisive role in restoring the disturbed barrier function, reducing xerosis and itching. In the long-term management of the disease, consistent basic therapy can lead to a prolonged recurrence-free interval [3]. The choice of topical preparations should be adapted to the stage of the disease or the current skin condition and is ideally applied twice daily to the entire integument [3]. The changes in barrier lipids and the epidermal differentiation complex are largely genetically determined, so lifelong treatment is useful.
Benefit relevant to progression
For optimal basic therapy, different active ingredients can be applied in combination. Urea is the longest-used active ingredient and a component of the natural moisturizing factor (NMF) of the epidermis [4]. Topical application of an externum containing 5-10% urea has been shown to hydrate the stratum corneum and decrease SCORAD [5,6]. In vitro studies have also demonstrated that urea reduces epidermis proliferation and induces increased synthesis of barrier lipids and antimicrobial peptides. Regulation of the expression of genes involved in keratinocyte differentiation (TG-1, involucrin, loricrin, filaggrin) and in the synthesis of antimicrobial peptides (LL-37, β-defensin-2) and barrier-related lipids plays an important role in this process [7]. On this background, it is presumed that urea as a component of basic therapy positively influences the function of keratinocytes and the synthesis of barrier lipids [7]. That the use of urea-containing topical preparations can significantly prolong the relapse-free interval of atopic dermatitis has been empirically demonstrated [8]. In addition to urea, glycerin and ceramides are proven effective substances in external formulations of products for basic therapy [9,10]. Glycerol promotes hydration of the stratum corneum and ceramides are essential lipids of the stratum corneum, which are decreased in patients with atopic dermatitis [9,10].
Literature:
- Werfel T, et al: The diagnosis and graded therapy of atopic dermatitis. Dtsch Arztebl Int 2014; 111: 509-520.
- AWMF: Guideline Neurodermatitis, Register number 013 – 027, ClassificationS2k Status: 03/31/2015 (under revision), valid until 03/30/2020 www.awmf.org/uploads/tx_szleitlinien/013-027l_S2k_Neurodermitis_2016-06-verlaengert.pdf
- Chylla R, Schnopp C, Volz T: Basic therapy in atopic dermatitis – new and proven. JDDG 2018; 16(8): 976-979. DOI: 10.1111/ddg.13594
- Rawlings AV, Harding CR: Moisturization and skin barrier func- tion. Dermatol Ther 2004; 17 (Suppl 1): 43-48.
- Bissonnette R, et al: A double-blind study of tolerance and efficacy of a new urea-containing moisturizer in patients with atopic dermatitis. J Cosmet Dermatol 2010; 9: 16-21.
- Loden M, Andersson AC, Lindberg M: Improvement in skin barrier function in patients with atopic dermatitis after treat- ment with a moisturizing cream (Canoderm). Br J Dermatol 1999; 140: 264-267.
- Grether-Beck S, et al: Urea uptake enhances barrier function and antimicrobial defense in humans by regulating epidermal gene expression. J Invest Dermatol 2012; 132: 1561-1572.
- Akerström U, et al. Comparison of Moisturizing Creams for the Prevention of Atopic Dermatitis Relapse: A Randomized Double-blind Controlled Multicentre Clinical Trial. Acta Derm Venereol 2015; 95: 587-592.
- Lindh JD, Bradley M: Clinical effectiveness of moisturizers in atopic dermatitis and related disorders: A Systematic Review. Am J Clin Dermatol 2015; 16: 341-359.
- Di Nardo A, et al: Ceramide and cholesterol composition of the skin of patients with atopic dermatitis. Acta Derm Venereol 1998; 78: 27-30.
HAUSARZT PRAXIS 2020; 15(2): 16