In case of confirmed food allergy, the label with the product composition must always be studied carefully. Even small changes in the list of ingredients can lead to pronounced allergic reactions, as illustrated by the example of meat allergy.
Medical history
Melanie, a 40-year-old nonatopic patient, has suffered from intermittent abdominal cramping and colic for years. In the last months a strong worsening of the symptoms occurred. Internal, gastroenterological and gynecological examinations showed no pathological findings. At the patient’s request, an allergy assessment was performed at the allergy ward of the USZ.
Allergological clarification
The detailed anamnesis revealed that the patient had suffered sporadically from nausea, abdominal cramps and occasionally vomiting since the age of 14 , first after eating sausages, later also after (abundant) meat consumption. Fish, poultry, cow’s milk and eggs are tolerated.
Prick tests with inhalant allergens and foods were all negative. Based on the history, intradermal tests were performed with meat extracts (beef, pork, and lamb), which resulted in a simple positive immediate reaction. Specific IgE were positive with beef RAST (radio-allergo-sorbent test) class 3, with pork class 2, with lamb class 1, and with other foods (NM) class 0. On three different days, open oral provocations were performed on an empty stomach, with nausea, abdominal cramps, diarrhea, itching of the ears, face, and palms occurring 4-8 h after provocation with 30-50 g of sausage (cervelat) or 100 g of beef (roasted). A third oral provocation was performed with the same amount of beef after previous ingestion of 400 mg DNCG (Natrii cromoglicas, Nalcrom®). The indication of the product is preventive treatment in locally and systemically manifested food allergies. After the same latency period, the same symptoms appeared again. With the positive tests, the diagnosis of “gastrointestinal food allergy in monovalent sensitization to meat protein with delayed symptomatology in a nonatopic patient (NMA type C according to Pichler)” was confirmed [1,2].
Course
Under strict elimination diet of meat products, neither abdominal colic nor diarrhea occurred subsequently. The patient continued to tolerate fish and poultry meat (including “poultry meat cheese” from Migros). Subsequent re-exposures to beef promptly resulted in recurrence.
An acute episode requiring treatment with severe colic, severe abdominal pain, and diarrhea occurred early in the morning (05:30 am) after the patient ate “poultry meatloaf” (Migros) the previous evening. After close study of the label, it became apparent that this “poultry meat cheese” also contained pork and bacon (declared) (Fig. 1). “Poultry meat cheese” is not always “poultry meat cheese”!

Interest of the case
In the case of a confirmed food allergy, the allergy sufferer must always study the label with the product composition carefully, also because changes are always possible here [3].
Comment
Meat allergies are relatively rare (Fig. 2). According to an earlier evaluation of the allergy ward at the USZ, meat allergy was diagnosed in only 33 patients (corresponding to a frequency of 8.2%) out of 402 cases of IgE-mediated food allergy (NMA) over a study period of approximately 10 years (1978-1987). Allergy to beef and pork was present in 18 patients (4.5%), chicken in 10 (2.5%), dried sausages in 3 (0.8%), and lamb in only 2 (0.5%). Lamb is considered hypoallergenic and is part of a low-allergen search diet. Approximately 40,000 new patients were cleared in the above period, so the percentage of meat allergic patients among allergy patients is approximately 0.08-0.1% [4]. In the literature, reports of allergies to beef, veal, and pork were initially sparse, apparently because meat proteins are denatured by frying and thus lose most of their allergenic potency.
However, offal, predominantly as porcine derivatives (also in denatured form), still possesses a high antigenicity, as shown in the listed case description (casuistry) [5].

The “porc-chat” syndrome
In France, pork allergy is relatively common. Based on observations in 30 patients with anaphylactic reactions after consumption of pork, French authors described a new syndrome (“porc-chat”) as a consequence of cross-allergy in cat allergic patients between cat epithelia and pork [6,7].
Similar conditions exist in “bird-egg” and “egg-bird” syndromes as a result of cross-sensitization between inhaled and ingested avian proteins [8]. Milk allergic patients may have concomitant allergy to veal/beef if sensitization is to the milk protein fraction β-lactoglobin, but this is rare [9].
Molecular diagnostics of meat allergy with determination of IgE antibodies to α-Gal
The work of A. Bircher and coworkers regarding the discovery of the carbohydrate galactose-1,3-alpha-galactose (α-Gal for short) as a new (food) allergen responsible for IgE-mediated delayed immediate-type reactions after red meat consumption provides an exciting lesson [10]. Careful clinical observations, epidemiological data and applied immunology led to the discovery of a new relevant allergen. α-Gal is an oligosaccharide (two galactose molecules) expressed in cells from most mammals. However, the enzyme β-galactosyl-α-1,3-galactosyltransferase, which is responsible for the formation of α-Gal, is inactivated in humans and Old World monkeys, so that the oligosaccharide cannot be synthesized.
Bircher et al. [10] describe the sequence of the identification of α-Gal as follows: The story started with the observation of anaphylactic reactions, which already occurred in cancer patients during the initial administration of the monoclonal antibody cetuximab (Erbitux®) [11,12]. Elevated anti-cetuximab IgE antibodies were measured in affected patients, as well as in control subjects from the same areas. These IgE antibodies were present before cetuximab administration, implying sensitization by another source. Especially in patients who developed a strong inflammatory reaction after tick bites, the production of IgE against α-Gal, which is probably also present in tick saliva, could be detected.
At the same time, an American research group led by Thomas Platts-Mills found that patients who had suffered from unexplained anaphylactic reactions for years also had IgE to α-Gal [13]. Previous investigations of such patients with regard to food allergy were consistently negative. Most suffered anaphylactic reactions to mammalian meat, but not to poultry and fish. The allergic reactions to mammalian meat occurred with up to several hours of latency because of the digestive process required for the release of α-Gal. Trigger factors include physical activity, alcohol, infections, or use of nonsteroidal anti-inflammatory drugs (NSAIDs). Recently, indolent systemic mastocytosis has been identified as a trigger factor in addition to the known trigger factors, so tryptase levels should also be measured in cases of unclear anaphylaxis [14].
Summary
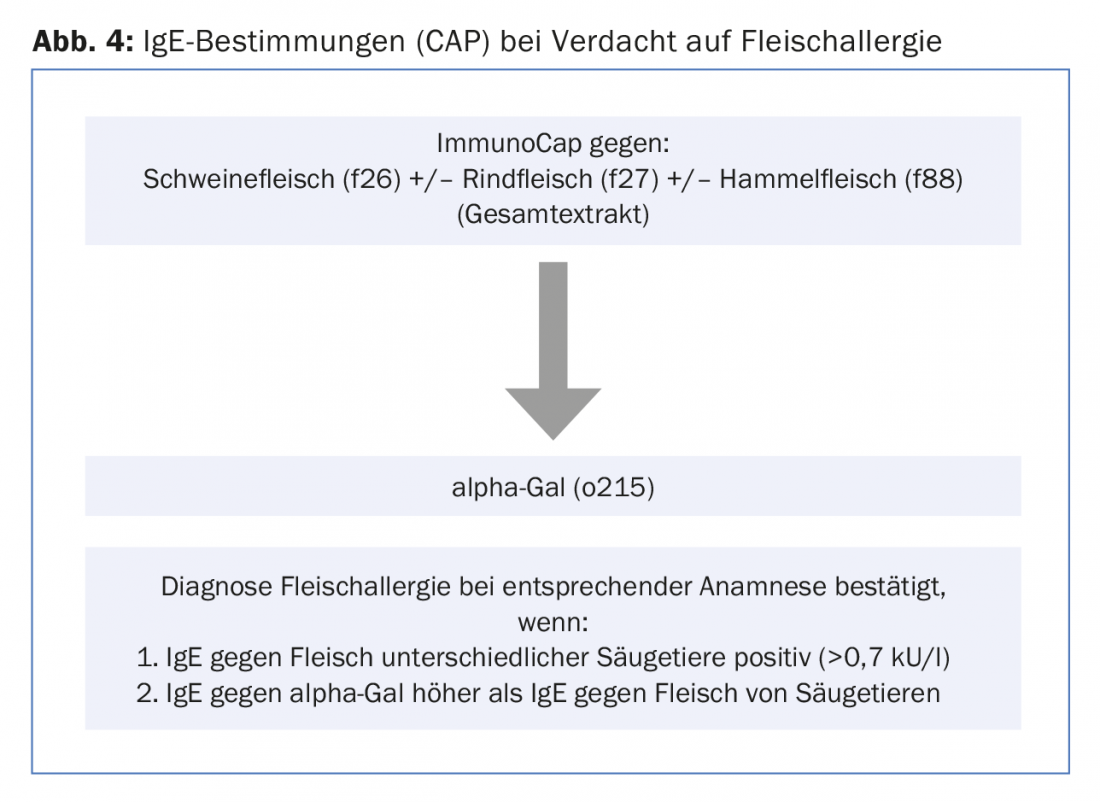
Primary sensitization to α-gal is likely through tick bites. This explains immediate type reactions after initial administration of cetuximab, a chimeric antibody that has an α-Gal epitope on the Fab fragment. The latency of an anaphylactic reaction can be up to several hours when meat is ingested, as alpha-gal must first be released through the digestive process. Patients must be advised to avoid consumption of mammalian meat, whereas poultry and fish are easily tolerated. It would be interesting to know retrospectively whether sensitization to α-Gal was also present in our two patients. The clarification of a meat allergy with specific IgE determinations should be performed according to the figure 4 .
Literature:
- Pichler WJ: IgE-mediated food allergies. Classification based on sensitization pathway. Allergology 1998; 21: 441-50.
- Wüthrich B, Blötzer I C: IgE-mediated food allergy type C: The rarer type of food allergy? A casuistry of 16 cases. Act Dermatol 2004; 30: 95-102.
- Wüthrich B: The new Swiss Food Ordinance (LMV). Allergology 2004; 27: 431-432.
- Wüthrich B: On food allergy. Frequency of symptoms and allergenic foods in 402 patients – cow’s milk allergy – food and atopic dermatitis. Allergology 1993: 16: 280-287.
- Wüthrich B: Allergies to meat proteins in adults. Allergology 1996;19: 130-134.
- Drouet M, et al: Le syndrome porc-chat ou l’allergie croisée entre viande de porc et épithélia de chat (1ère partie). Allergie et Immunologie 1994; 26: 166-172.
- Sabbah A, et al: Le syndrome porc-chat ou l’allergie croisée entre viande de porc et épithélia de chat (2e partie). Allergie et Immunologie 1994; 26: 173-180.
- Wyss M, Huwyler T, Wüthrich B: “Bird-egg” and “egg-bird” syndrome. Cross-sensitization between inhaled and ingestive avian proteins. Allergology 1991; 14: 275-278.
- Stöger P, Wüthrich B: Type I allergy to cow milk proteins in adults. A retrospective study of 34 adult milk- and cheese-allergic patients. Int Arch Allergy Immunol 1993; 102: 399-407.
- Bircher A, Scherer Hofmeier K, Michel S: Allergology and immunology: the discovery of a new allergen: galactose-1,3-alpha-galactose. Switzerland Med Forum 2013; 13(0102): 19-21.
- O’Neil B, Allen R, Spigel D, et al: High incidence of cetuximab-related infusion reactions in Tennessee and North Carolina and the association with atopic history. Journal of Clinical Oncology 2007; 25(24): 3644-3648.
- Chung CH, Mirakhur B, Chan E, et al: Cetuximab-Induced Anaphylaxis and IgE specific for Galactose-alpha-1,3-galactose. New Engl J Med 2008; 358(11): 1109-1117.
- Commins S, Satinover S, Hosen J, et al: Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol 2009; 123(2): 426-433.
- Malisiewicz B, Kaufmann R, Valesky E: Delayed anaphylaxis after consumption of kidney spit – a link between α-gal and mastocytosis. Allergology 2017; 40: 517-521.
DERMATOLOGIE PRAXIS 2018; 28(4): 38-41
DERMATOLOGIE PRAXIS 2018 Special Edition (Anniversary Issue), Prof. Brunello Wüthrich











