Curative therapies for hepatocellular carcinoma include surgical resection, ablation, and liver transplantation. Internationally valid recommendations for liver transplantation in HCC were formulated at the 2010 Zurich Consensus Conference.
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-associated death worldwide and the sixth leading cause of death in Switzerland [1]. The incidence is increasing over the long-term course. The main causes here are infections with the hepatitis B/C virus (HBV/HCV) and, more recently, the epidemiological increase in non-alcoholic steatohepatitis (NASH). Untreated, HCC has an unfavorable prognosis with a 5-year survival rate of less than 10%. The majority of patients develop HCC in the setting of cirrhosis, making optimal treatment strategies much more difficult. The last decade has seen decisive advances in biomedical knowledge of the disease and in therapy. Treatment options are mainly based on surgical (resection, liver transplantation) and non-surgical approaches (interventional radiological chemoembolization, locoregional ablation, chemotherapy). In the case of localized and non-multifocal HCC disease, surgical tumor removal and liver transplantation are the gold standard [2,3].
Clinical presentation and diagnosis
The symptoms and clinical presentation depend on the stage of the tumor disease. At an advanced stage, patients often present with the triad of upper abdominal pain, palpable tumor in the right upper abdomen, and weight loss. In addition, ascites and clinical signs of portal hypertension and rarely icterus occur. In less than 5% of cases, patients present with tumor rupture, which can also lead to life-threatening bleeding and intra-abdominal “tumor seeding.” In addition, numerous paraneoplastic complications have been described, such as hypoglycemia, hypercalcemia, erythrocytosis, and hypertrophic pulmonary osteoarthropathy. In patients with liver cirrhosis who are monitored in a screening program, tumors can be detected at an earlier stage.
The tumor marker α-fetoprotein (AFP) is elevated in up to 90% of patients with HCC; however, it does not correlate with the extent of tumor disease and is limited in both specificity and sensitivity, as benign conditions such as hepatitis and cirrhosis may also be associated with AFP elevation. As a basic rule, an AFP >200 ng/ml in conjunction with appropriate imaging is highly sensitive for HCC disease.
With regard to imaging, CT, MRI as well as US are in the foreground. Ultrasound is well suited as a low-cost screening method. However, the low sensitivity and specificity as well as the high false-negative rates of more than 50% are the limitations of this test.
Similar to the established BiRAD criteria for breast carcinoma, LiRAD criteria (including contrast enhancement in the arterial phase, size of the finding, “wash out”) were defined by the American Society of Radiology. Based on these criteria, a hepatic nodule can be evaluated for malignancy.
With improved imaging, confirmatory diagnosis is indicated only in the presence of equivocal findings. In this case, ultrasound-guided percutaneous fine-needle biopsy is the gold standard, although tumor seeding may occur along the biopsy channel in <1%.
Staging according to BCLC classification
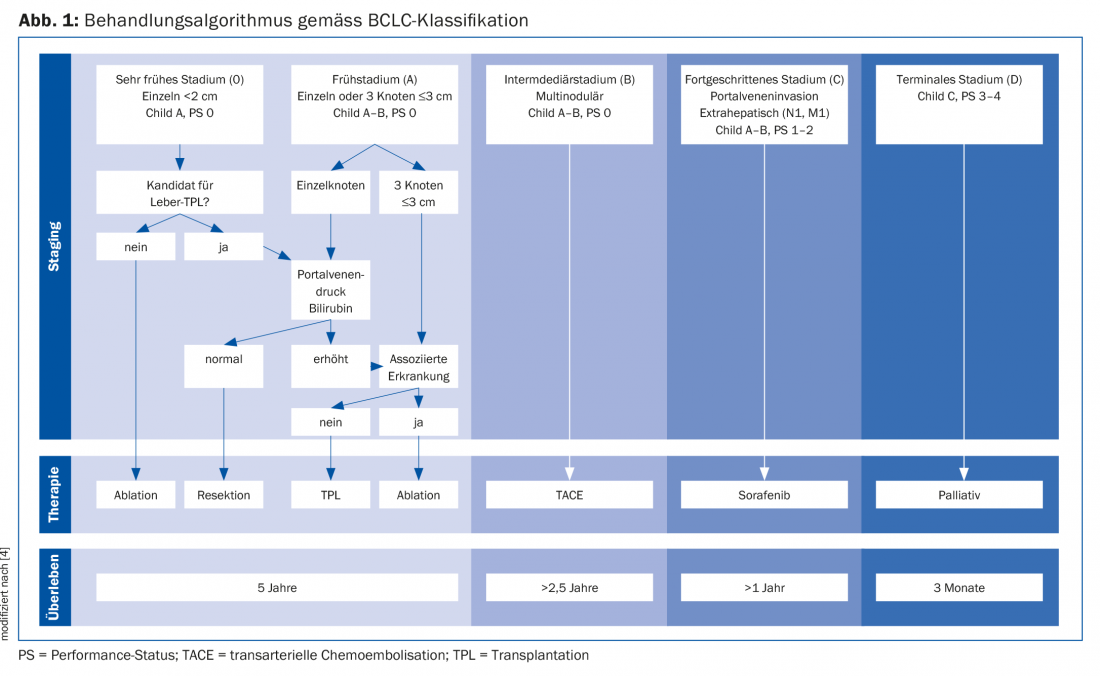
Staging and the appropriate choice of therapy are performed according to the Barcelona Clinic Liver Cancer (BCLC) classification algorithm, which defines five stages of HCC disease. These depend on tumor number and size, Child-Pugh stage, and ECOG performance status (Fig. 1) [4].
Conservative therapies: System therapy vs. local therapies
Conservative therapeutic modalities include systemic therapy (multikinase inhibitors and immunotherapy) and tumor ablation methods. The protein kinase inhibitor sorafenib is indicated as first-line therapy for stage C BCLC. There is a survival benefit of 10.7 vs. 7.9 months in patients treated with sorafenib (vs. placebo) [5]. Newer multikinase inhibitors such as lenvatinib also appear to be effective according to recent non-inferiority studies (not yet published: Cheng et al., Abstract 4001 at ASCO 2017) and will soon be approved as first-line systemic therapies. In addition, other multikinase inhibitors (e.g., regorafenib and cabozantinib) will soon be available as second-line therapies [6].
Still unclear and the subject of current research is the place of immunotherapy, with phase II trials of nivolumab showing promising results. Thus, we can look forward to the upcoming efficacy studies with excitement.
Patients with HCC on the liver transplant list are reevaluated regularly. In the event of hepatic progression of tumor disease outside of listing criteria-determined with imaging and AFP-in many cases, inactive listing occurs and downstaging is anticipated. If progression occurs despite locoregional therapies, the patient should be “delisted” from the transplant waiting list. Transplant centers with long waiting lists perform local bridging therapies for tumor control in these patients. These include transarterial chemoembolization (TACE), radiofrequency (RFA) and microwave ablation (MWA), and percutaneous ethanol injection (PEI) [7]. TACE is selective embolization of hepatoma arterial inflow using chemotherapeutic agents (mainly cisplatin or doxorubicin), which in combination results in ischemic tumor damage and local chemotherapy with few systemic side effects. With this interventional method, a size reduction of the tumor from 50% to complete tumor necrosis can be achieved. TACE can also be used to reduce the waiting list drop-out rate and tumor recurrence rate after liver transplantation and to achieve downstaging. RFA/MWA involves imaging-assisted percutaneous placement of an RFA probe into the tumor, which is thermally destroyed with high-frequency alternating electrical energy. Results have been satisfactory, and reports of a zero percent drop-out rate and 3-year survival of up to 83% have been published [8]. PEI has been the least studied as a bridging therapy. The use of a fine needle makes it theoretically less invasive and therefore less likely to cause “tumor seeding.” With a favorable side effect spectrum of PEI, successful results can be achieved with up to 80% tumor necrosis. However, since multiple treatments are required, the majority of this technique has been replaced by RFA. New ablation techniques, such as selective internal radiotherapy (SIRT), show promising results in terms of tumor response and survival [4]. In a recent study, patients with HCC after frustrated TACE were treated with SIRT versus sorafenib; there was no difference in survival [9]. However, the value of SIRT remains to be defined according to recent studies [4].
In case of borderline tumor size and number after bridging therapy, the patient is listed inactive to learn about tumor biology by MRI, CT and AFP during progression. If no tumor progression is observed after a three-month inactive waiting period on the list, the patient may be actively listed.
Surgical therapy: resection vs. liver transplantation
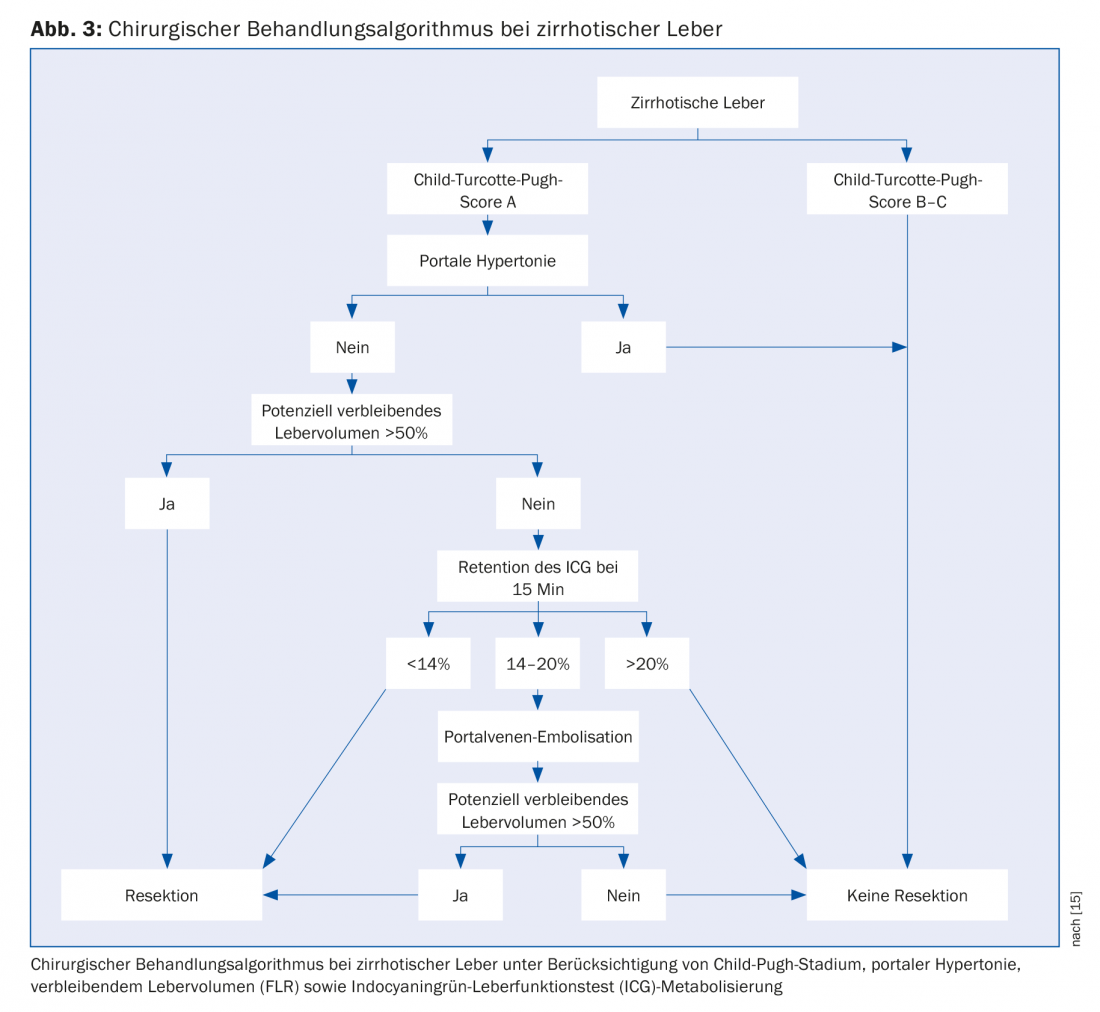
The gold standard for HCC is surgical resection or orthotopic liver transplantation. However, only 10-30% of patients with HCC are candidates for resection. After exploratory laparotomy, curative resection can be performed in only 50-70% of patients. The only contraindication to surgery is extrahepatic metastasis. Resectability depends on tumor size, number, proximity to blood vessels, and underlying liver disease. The goal of surgery is complete resection in healthy tissue corresponding to a histopathologic R0. Resectability is also co-determined by in-situ remaining liver volume (“future liver remnant”, FLR) and portal hypertension. According to our proposed algorithm, a residual volume of the remaining tumor-free liver of at least 50% should remain. For volumes below this value, portal vein embolization can be performed for volume induction. Portal hypertension is no longer necessarily an absolute contraindication to liver resection [10,11]. When considering resection in cirrhotic patients, a minimally invasive surgical approach should be pursued whenever possible, as this group of patients is particularly likely to benefit [12]. We in Zurich offer our patients laparoscopic and robotic resection procedures as minimally invasive surgeries [7].
For smaller tumors (<2-3 cm), the indication for curative ablation is discussed, as equivalent survival compared with surgical resection has been postulated [13,14]. However, the value of these studies should be considered with reservations, because on the one hand they are subgroup analyses from retrospective studies with a limited level of evidence, and on the other hand the few prospective studies so far have shown no difference [7].
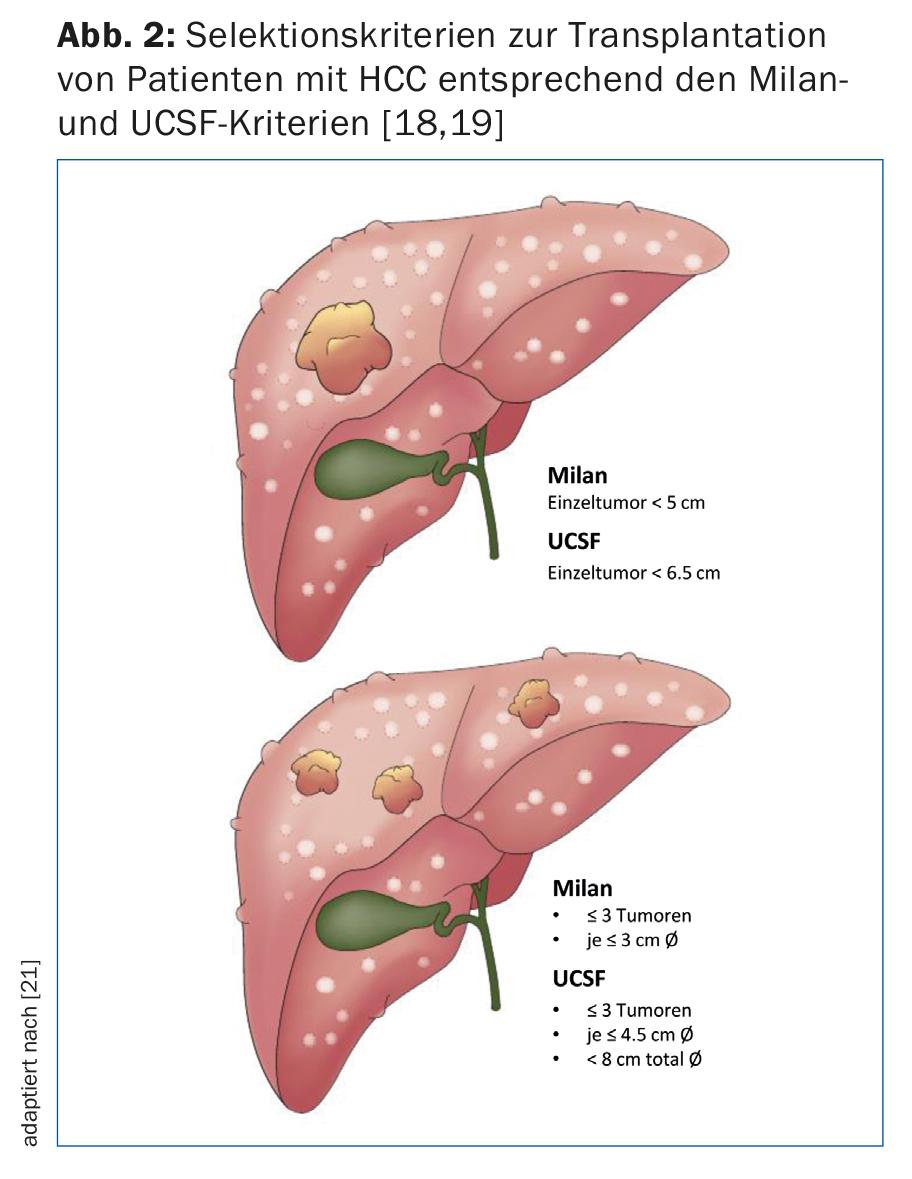
Liver transplantation is clearly superior to resection in terms of 5-year recurrence-free survival and is certainly the best therapeutic option in cirrhotic patients with small HCC. Due to the shortage of donor organs as well as the often advanced stage of disease outside accepted criteria (Fig. 2), transplantation can only be offered in a selective HCC population. Therefore, resection remains the treatment of choice for cirrhotic patients with compensated liver function (Child-Pugh stage A) without portal hypertension (Fig. 3) [15].
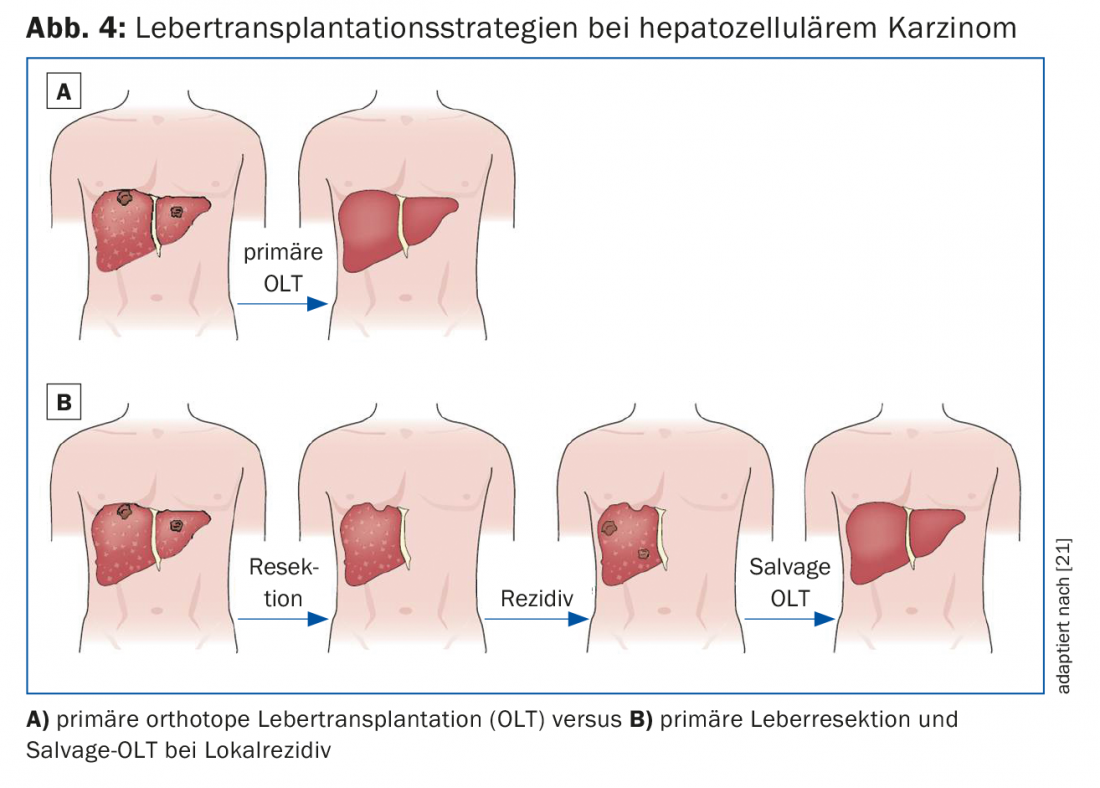
Combination therapy of liver resection and transplantation may be considered in three different clinical scenarios:
- Primary therapy with salvage transplantation in case of tumor recurrence (Fig. 4).
- Diagnostic procedure for histopathological evaluation of the tumor with regard to vascular invasion as well as tumor satellites with consecutive adequate selection of transplant candidates.
- Bridging therapy before transplantation to ensure tumor control within Milan or UCSF criteria (Fig. 2) [16].
HCC patients with noncompensated liver function (Child-Pugh B or C) and/or portal hypertension should receive primary liver transplantation if the tumor disease is within the respective accepted transplantation criteria (Fig. 2).
Liver transplantation appears to be the ideal HCC therapy because complete removal of the tumor-infested liver is formally equivalent to oncologic tumor removal with negative resection margins. In the context of donor organ shortage, liver transplantation is considered only in patients whose survival is comparable to an organ recipient without HCC.
Originally, Bismuth’s group reported the extent of tumor involvement as a surrogate marker for tumor biology. They demonstrated that patients with small uni- or binodular tumors <3 cm have better survival in case of transplantation compared with tumor resection (83% vs. 18%). In addition, patients with diffuse HCC with more than two nodules >3 cm or portal vein thrombus had a higher recurrence rate with consecutive decreased survival [17]. Mazzaferro et al. studied patients with cirrhosis and non-resectable HCC treated with transplantation. They established specific criteria – the basis of the so-called Milan criteria – defined as a single tumor <5 cm or ≤3 tumors each <3 cm in diameter (Fig. 2). Patients who met the Milan criteria showed significantly improved recurrence-free and overall survival after transplantation [18]. Numerous studies have reported excellent survival data in HCC patients transplanted within these criteria. This led some experts to consider the criteria too restrictive. In fact, a research group from the University of California, San Francisco (UCSF) showed that patients outside the Milan criteria also benefit significantly from transplantation. The broader UCSF criteria are defined as single tumor ≤6.5 cm or ≤3 tumors each ≤4.5 cm and sum of total tumor diameters ≤8 cm (Fig. 2) [19]. The European Liver and Intestine Transplant Association (ELITA) and International Liver Transplantation Society (ILTS) have launched the Metroticket project. Based on pre- and postoperative patient data (maximum tumor size, number of tumors, AFP value), “post-transplant” survival can be predicted using an online calculator on the website www.hcc-olt-metroticket.org [20] (Fig. 5).
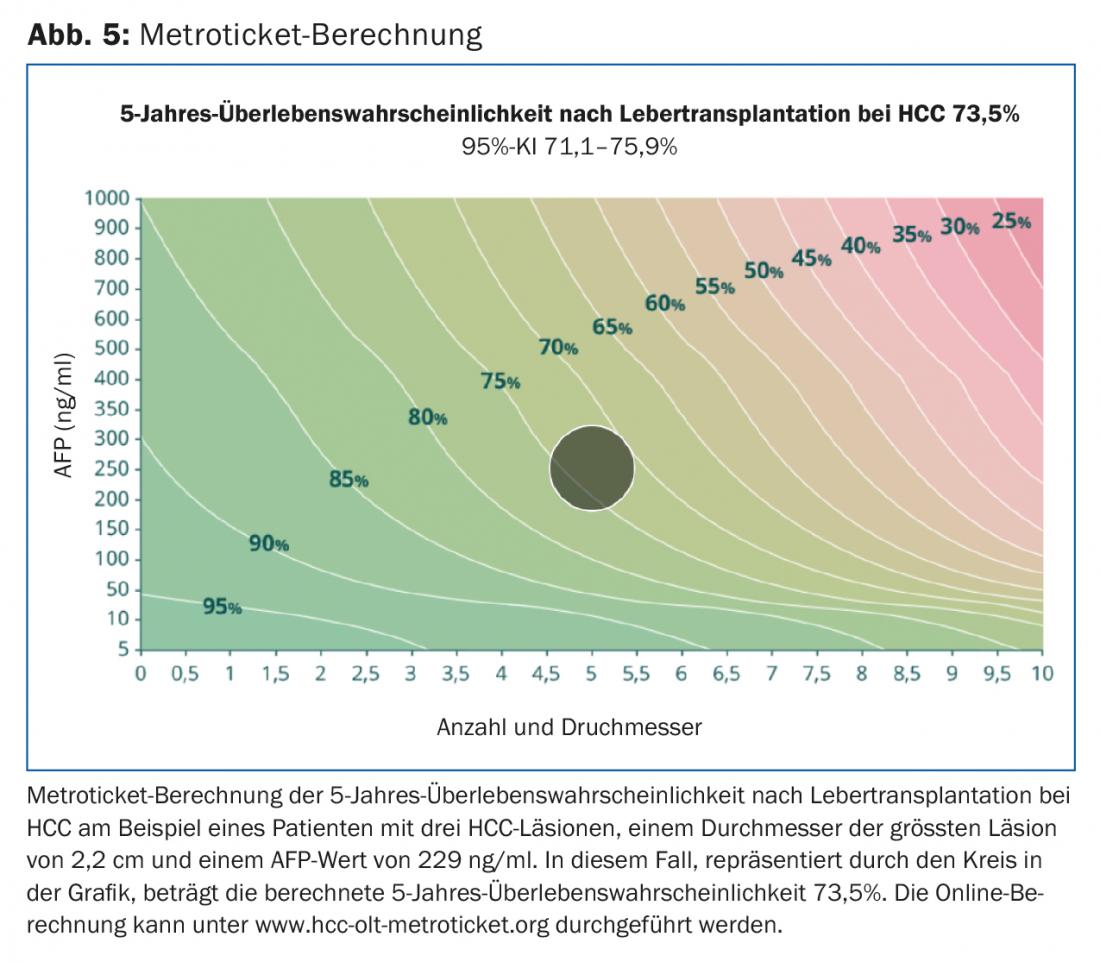
Patients transplanted within Milan or UCSF criteria have similar survival data (80% vs. 75% 5-year survival). However, transplantation outside of UCSF criteria is associated with decreased survival – with a 5-year survival rate well below 50%. Regardless of tumor size and number, evidence of macrovascular tumor invasion is a contraindication to liver transplantation.
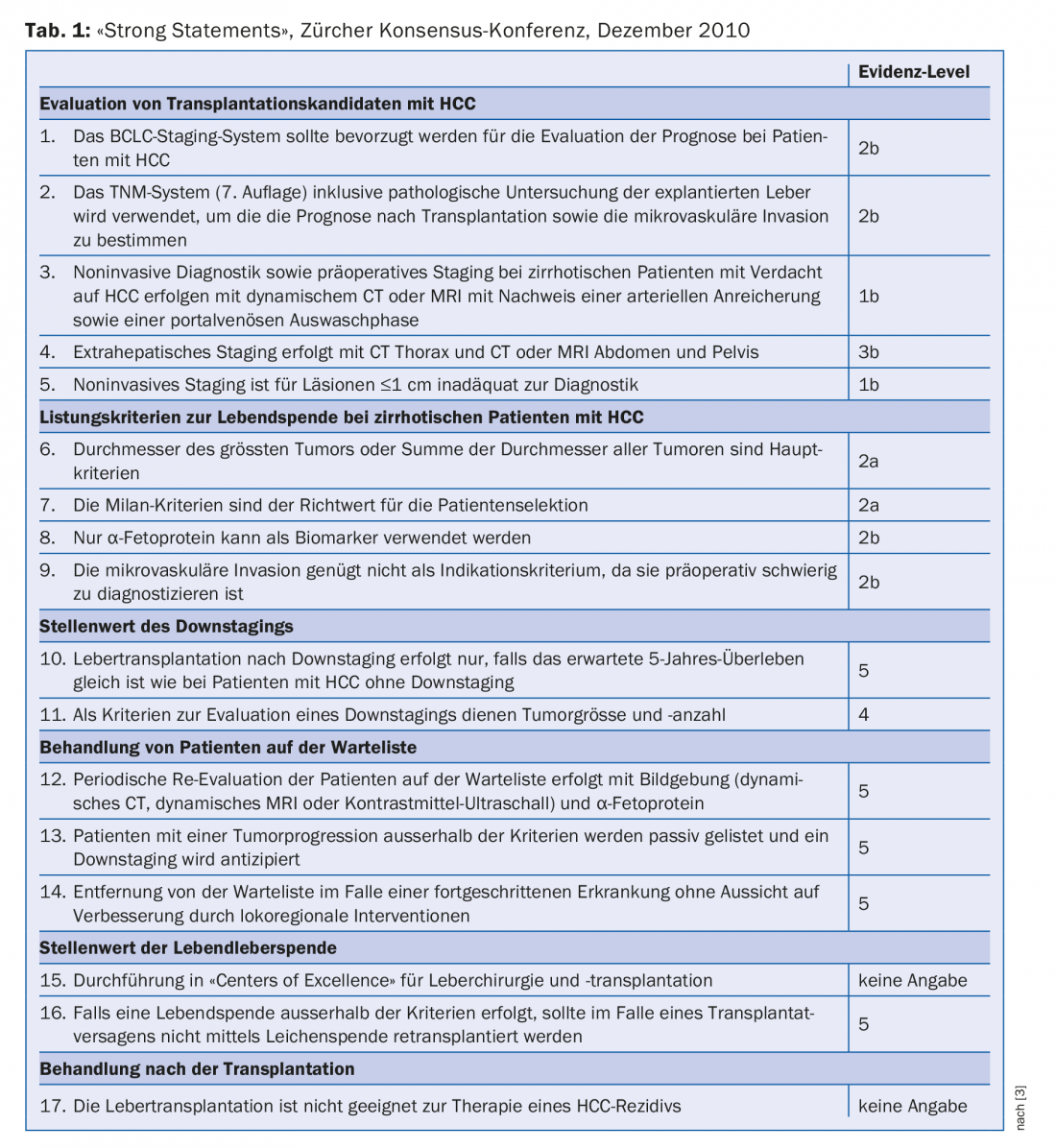
In December 2010, a consensus conference with international experts was held in Zurich. The goal was to elaborate the current practice of liver transplantation for HCC and to develop internationally accepted guidelines. A total of 37 statements and recommendations were formulated. These address the areas of: Evaluation of liver transplant candidates, criteria for listing cirrhotic and non-cirrhotic patients, the role of tumor downstaging, treatment of patients on the waiting list, the value of living liver donation, and post-transplant treatment. The most weighty 17 recommendations (“strong statements”) are summarized in Table 1 [3].
Take-Home Messages
- The incidence of hepatocellular carcinoma (HCC) is increasing worldwide.
- Curative therapeutic strategies include surgical resection, ablation, and liver transplantation.
- After sorafenib, lenvatinib can be used as first-line therapy.
- Liver transplantation via cadaveric or living donation is a potential therapeutic option for patients with HCC and end-stage liver disease (ESLD).
- Patients on the transplant waiting list benefit from bridging therapies consisting of transarterial chemoembolization (TACE), radiofrequency ablation (RFA), and percutaneous ethanol injection (PEI). The role of SIRT is the subject of current research.
- Internationally valid recommendations for liver transplantation in patients with HCC were formulated at the Zurich Consensus Conference in December 2010.
Literature:
- Parkin DM, et al: Global cancer statistics, 2002. CA Cancer J Clin 2005; 55: 74-108.
- Dutkowski P, et al: Challenges to Liver Transplantation and Strategies to Improve Outcomes. Gastroenterology 2015 Feb; 148(2): 307-323.
- Clavien PA, et al: Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. The Lancet Oncology 2012; 13: e11-22.
- Bruix J, Reig M, Sherman M: Evidence-Based Diagnosis, Staging, and Treatment of Patients With Hepatocellular Carcinoma. Gastroenterology 2016; 150: 835-853.
- Llovet JM, et al: Sorafenib in advanced hepatocellular carcinoma. The New England Journal of Medicine 2008; 359: 378-390.
- Bruix J, et al: Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017; 389: 56-66.
- Petrowsky H, Busuttil RW: Resection or ablation of small hepatocellular carcinoma: what is the better treatment? Journal of Hepatology 2008; 49: 502-504.
- Mazzaferro V, et al: Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Annals of Surgery 2004; 240: 900-909.
- Vilgrain V, et al: Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. The Lancet Oncology 2017; 18: 1624-1636.
- Capussotti L, et al: Liver resection for hepatocellular carcinoma on cirrhosis: analysis of mortality, morbidity and survival – a European single center experience. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 2005; 31: 986-993.
- Cucchetti A, et al: Is portal hypertension a contraindication to hepatic resection? Annals of surgery 2009; 250: 922-928.
- Abu Hilal M, et al: The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Annals of surgery 2017. DOI: 10.1097/SLA.00000000002524 [Epub ahead of print].
- Vivarelli M, et al: Surgical resection versus percutaneous radiofrequency ablation in the treatment of hepatocellular carcinoma on cirrhotic liver. Annals of Surgery 2004; 240: 102-107.
- Guglielmi A, et al: Radiofrequency ablation versus surgical resection for the treatment of hepatocellular carcinoma in cirrhosis. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 2008; 12: 192-198.
- Clavien PA, et al: Strategies for safer liver surgery and partial liver transplantation. N Engl J Med 2007; 356: 1545-1559.
- Chua TC, et al: Hepatic resection for transplantable hepatocellular carcinoma for patients within Milan and UCSF criteria. Am J Clin Oncol 2012; 35: 141-145.
- Bismuth H, et al: Liver resection versus transplantation for hepatocellular carcinoma in cirrhotic patients. Annals of surgery 1993; 218: 145-151.
- Mazzaferro V, et al: Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996; 334: 693-699.
- Yao FY, et al: Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001; 33: 1394-1403.
- Mazzaferro V, et al: Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. The Lancet Oncology 2009; 10: 35-43.
- Agopian V, Petrowsky H: Liver transplantation for malignant tumors. In: Fong Y, et al. (Eds.): Hepatobiliary cancer. People’s Medical Publishing House 2014; 293-316.
HAUSARZT PRAXIS 2018; 13(1): 14-19











