Systemic sclerosis (SSc) is one of the most serious diseases because it occurs everywhere in the body, but there is a solution for few problems and virtually every organ must be treated individually. There is still no universal medication for them as there is for other diseases, so there is not one biologic or one particular immunosuppressant.
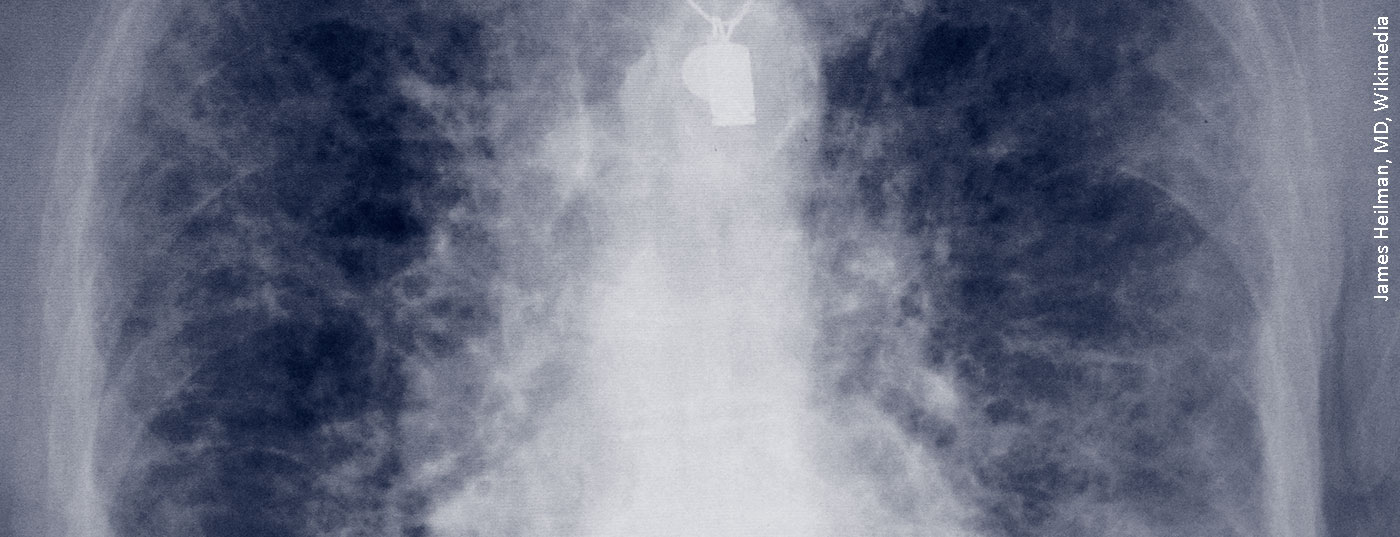
Mandatory for any patient presenting with systemic sclerosis is pulmonary examination, for two components: pulmonary fibrosis, which is worse, and pulmonary arterial hypertension (PAH), for which at least there are more medications. Loss of distensibility of the lung and loss of its gas exchange function are the two pathomechanisms of the disease pattern of pulmonary fibrosis. It is 100 times less common, but requires more deaths annually than asthma. The dilemma is that there are more than a hundred different conditions that can result in the end stage of pulmonary fibrosis.
“The deterioration can be very rapid in systemic sclerosis, and that’s the dangerous part,” warned Professor Ulf Müller-Ladner, MD, of the Department of Rheumatology and Clinical Immunology at the Kerckhoff Clinic in Bad Nauheim, Germany. “Patients don’t have a lot of antecedents, maybe a digital ulcer, and suddenly pulmonary fibrosis or pulmonary hypertension is already there.” The patients themselves don’t notice until dyspnea symptoms start. Therefore, according to the rheumatologist, it is also elementary in his discipline to always examine the lungs of a patient, regardless of whether he or she is symptomatic or not.
In SSc, pulmonary fibrosis has become increasingly important in the list of organ manifestations. Not least because other complications such as renal crises or cardiovascular or gastrointestinal problems have become more treatable over time – whereas SSc-associated pulmonary fibrosis (SSc-ILD) has not. “If you stratify it based on the dimensions on HRCT, patients with SSc show fibrosis on CT in more than 30%,” said Professor Andreas Günther, M.D., head of the Fibrosing Lung Disease Focus, Giessen Marburg University Hospital. “So it’s already more of a severe disease with a poor outcome.”
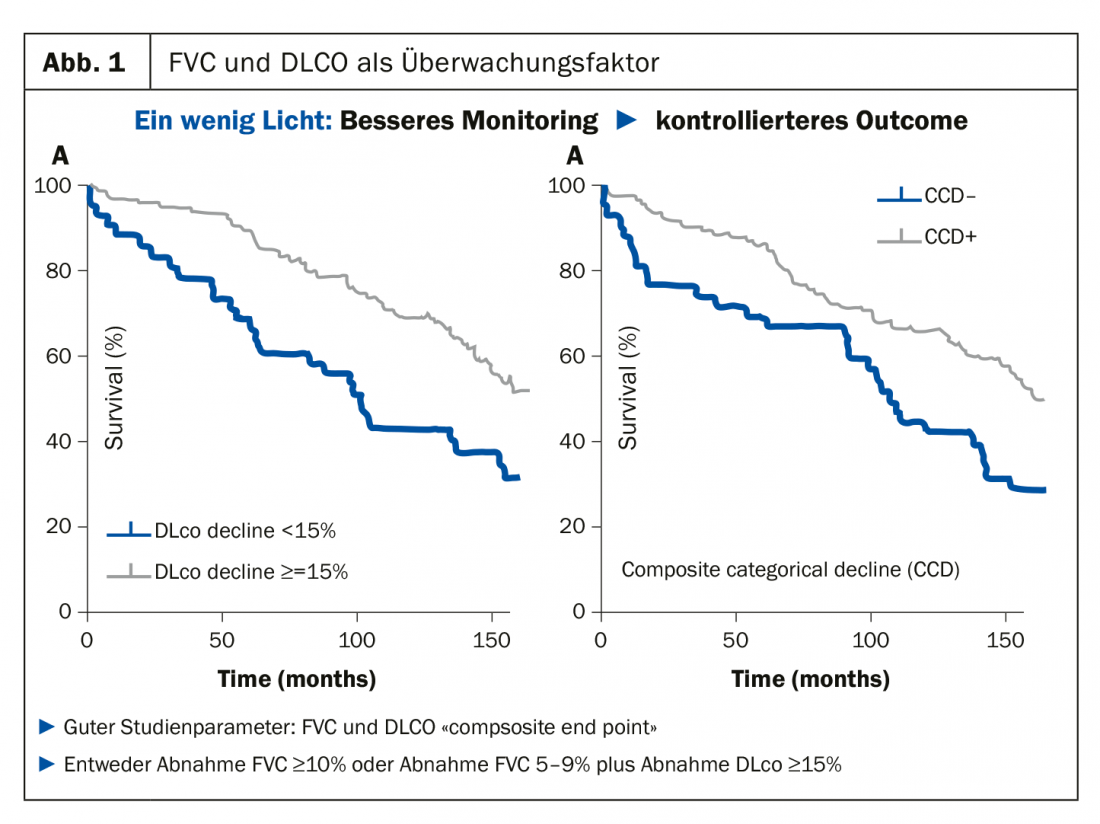
Better monitoring = more controlled outcome
As a rheumatologist who has to keep an eye on and monitor the lungs, Prof. Müller-Ladner always advises his colleagues to stick to the parameters that are relatively easy to measure, i.e. vital capacity (FVC) and diffusion capacity (DLCO), as it is this combination that has proved very positive as a monitoring factor in studies. “If the combination of these two parameters progresses very quickly, then the curves also diverge” (Fig. 1). This composite end point is now also established in studies. A decrease in FVC ≥10% or a decrease of 5-9% plus a decrease in DLCO of ≥15% were to be considered decisive. “As rheumatologists, we may smile at these small numbers, but with regard to the lungs, they are absolutely worthwhile,” the specialist made clear a factor that his specialist colleagues tend to underestimate: “A small change to the lungs can have a big impact, and patients notice that too.”
“The main thing is to do something”
In many rheumatological diseases, the therapy is similar: there are inflammatory cells, which are immobilized, and then everything is fine – side effects left out. The situation is different for the SSc. “Because you’ve got multiple components going on here in parallel, and nobody quite knows what it starts with – immune system, fibrosis, vascular?” And if you turn down one of those switches, you may use it to turn up something elsewhere, which doesn’t improve the overall condition. At the same time, we are dealing with fibrosis, “and antagonizing fibrosis is one of the most difficult tasks of all. So the question remains, how to proceed in treatment: take away the trigger or direct binding?
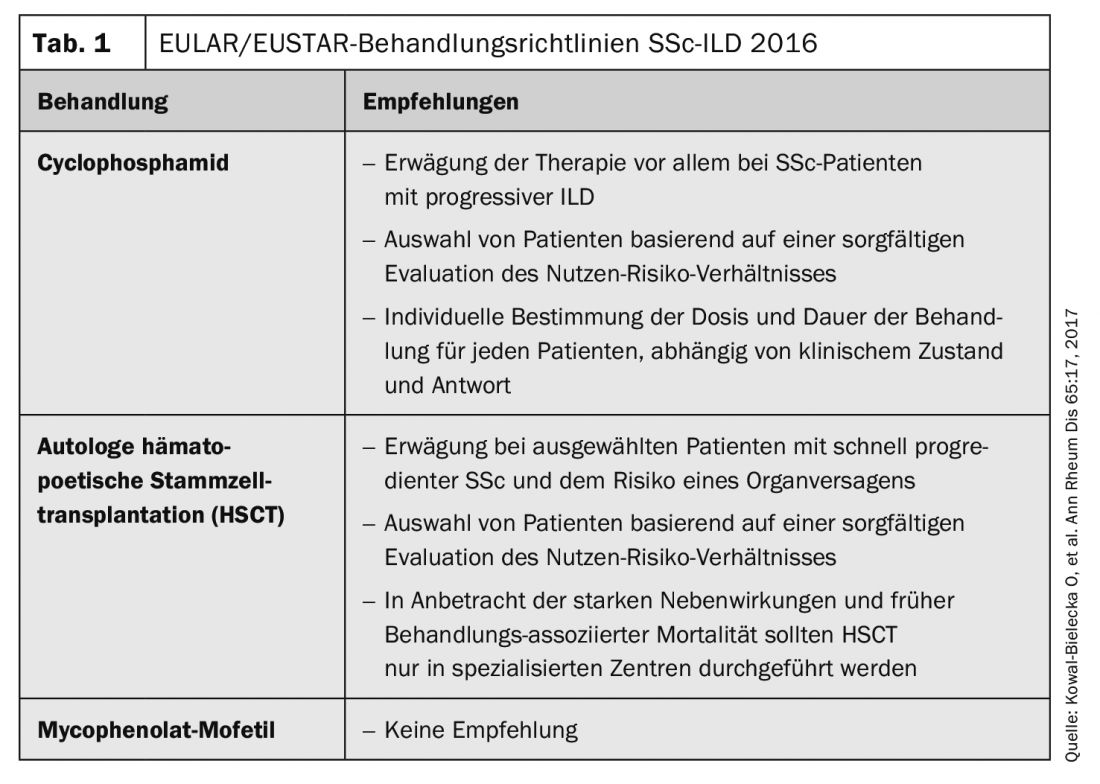
Rheumatologists answer this question by doing what they can and know how to do, according to Prof. Müller-Ladner: they take methotrexate or penicillamine, “the main thing is to do something.” But sometimes actionism can also cause damage, for example if the diagnosis is not correct. If the findings are unclear, the expert says, one should always consult a pulmonologist in case of doubt. Prof. Günther referred to the EULAR/EUSTAR treatment guidelines SSc-ILD from 2016, which recommend cyclophosphamide or autologous hematopoietic stem cell transplantation (HSCT) (tab. 1). Mycophenolate mofetil (MMF), the pulmonologist commented, is certainly no less effective than cyclophosphamide, but less toxic, which is why it is still readily prescribed.
Promising studies
Another problem: Systemic sclerosis remains a rare disease, making large studies desirable but scarce. “Shaking it out of your wrist like you do with rheumatoid arthritis (RA) just doesn’t work because you just can’t get the numbers,” Prof. Müller-Ladner explained. That is why every publication is valuable. The rheumatologist first presented two studies (FaSScinate and FocuSSced) with relatively small numbers of participants, both of which focused on combating inflammation with interleukin-6 (IL-6) using tocilizumab. Especially in the FocuSSced study, it was seen that in the long-term range, the anti-inflammation related to FVC under IL-6 was promising.
The SENSCIS trial, in turn, evaluated the effect of nintedanib versus placebo with the primary endpoint of reduction in functional vital capacity (mL/year). It is geared toward a stably adjusted real-life baseline medication with MTX or MMF. Here, too, the results were positive after 52 weeks (Fig. 2). “We need a reasonable antifibrotic drug,” Prof. Müller-Ladner expressed his confidence, “because fibrosis can only be treated indirectly so far.”
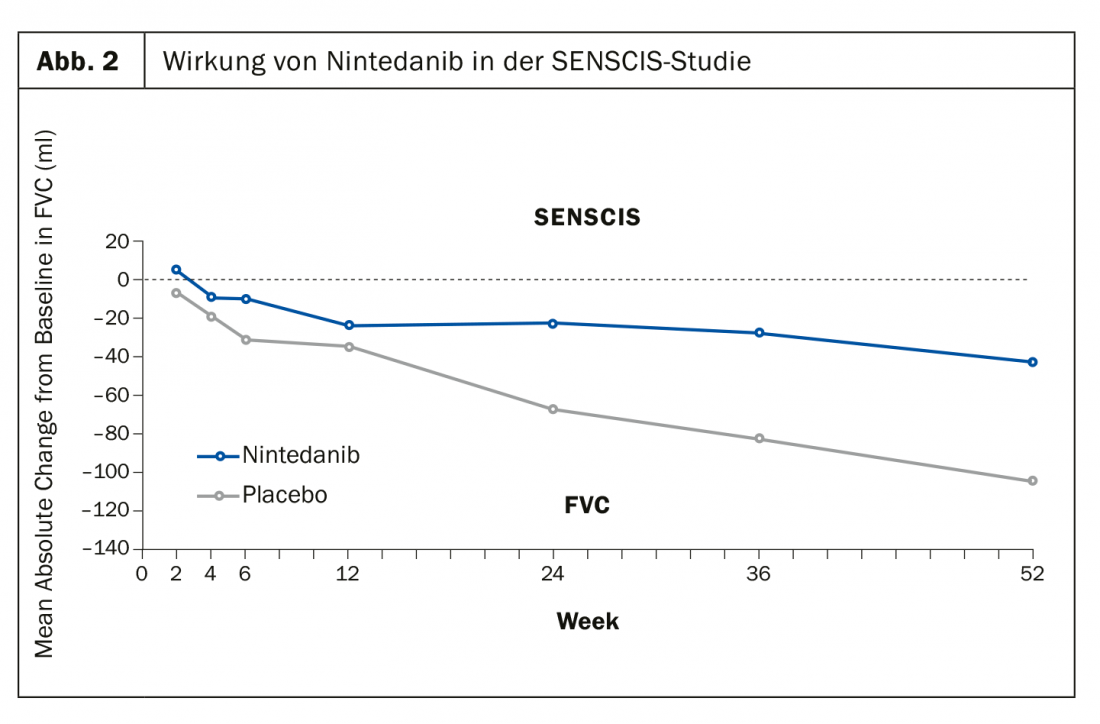
However, nintedanib is not currently approved for the treatment of SSc/SSc-ILD or other progressive interstitial lung disease (PF-ILD) outside of idiopathic pulmonary fibrosis (IPF). This makes it all the more important to obtain approval in the foreseeable future not only for the purely pulmonary fibrotic forms of the disease.
Source: Industry symposium “Pulmonary fibrosis: the challenge of SSc and other rheumatic diseases” at the DGRh; Organizer: Boehringer Ingelheim.
InFo PNEUMOLOGY & ALLERGOLOGY 2019; 3(1): 30-31 (published 11 Dec 19, ahead of print).