The central task of the European Society for Medical Oncology (ESMO) is to improve the quality of cancer treatment, cancer prevention and diagnosis as well as palliative care and aftercare for patients. The aim is to keep doctors up to date with best practices and the latest advances and developments in the field of cancer medicine.
Metastases are primarily responsible for cancer-related deaths. Therefore, blocking the metastatic cascade has a decisive clinical impact. However, the development of cancer drugs, including cancer immunotherapies, is largely evaluated on their ability to cause tumor shrinkage. The effect on metastasis is largely neglected, as it has proven difficult to address. There is therefore an urgent need for new therapeutic strategies and agents that target metastasis.
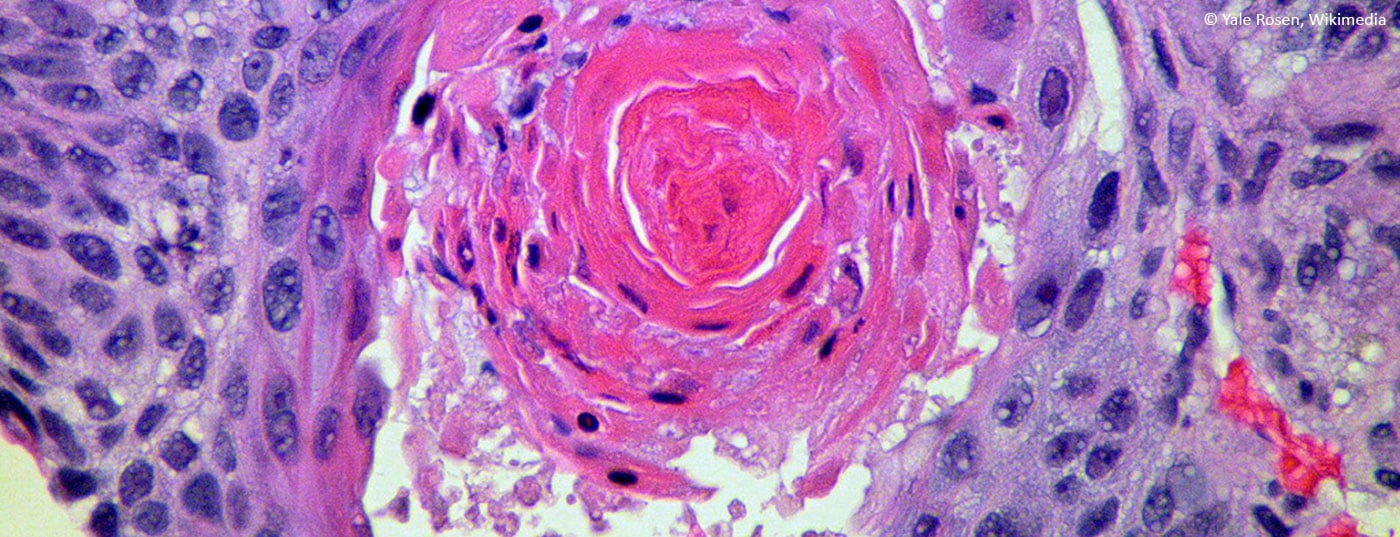
Using an attenuated Salmonella Typhimurium strain YB1 developed in the laboratory, it was found that attenuated Salmonella strongly suppressed cancer metastasis regardless of cancer type and genetic background by eliciting a strong anti-metastatic immune response. Mutant mice and antibody-mediated cell depletion were used to determine the genetic and cellular requirements of the host for bacterial suppression of cancer cell metastasis [1]. The study has shown that the suppression of cancer metastasis by attenuated Salmonella only requires the innate immune response. Among the many induced cytokines, IFN-γ has been identified as an indispensable factor for the inhibition of cancer metastasis. CyTOF- and antibody-mediated cell depletion analysis of innate immune responses after Salmonella treatment revealed that NK cells are the major factor involved in suppression of Salmonella-induced metastasis. It was shown that IFN-γ was mainly produced by NK cells during early Salmonella infection and IFN-γ in turn promoted the accumulation, activation and cytotoxicity of NK cells. The IFN-γ-dependent NK cells directly eliminated newly accumulated cancer cells in the lung to block the cancer metastasis cascade in response to Salmonella treatment.
Blood test for early cancer detection
The use of a rapid liquid biopsy platform that can help clinicians diagnose different types of cancer – especially in patients who develop cancers that are not targeted by current screening programs – would create a paradigm shift in cancer diagnostics. Current liquid biopsies focus on single tumor-derived biomarkers, such as circulating tumor DNA (ctDNA), which limits the sensitivity of the test, especially in early-stage cancers that do not secrete enough genetic material. The Dxcover® Cancer Liquid Biopsy has now been tested for its ability to predict individual cancer types in organ-specific classifications: Brain, Breast, Colorectal, Kidney, Lung, Ovarian, Pancreatic and Prostate cancers [2]. The test uses Fourier transform infrared spectroscopy
(FTIR) to create spectral profiles of serum samples and machine learning algorithms to predict disease status. In addition, a further exploratory assessment was made of the ability to distinguish the signature of one of the eight cancer types from samples from patients without cancer. Test performance was assessed when cancer samples were grouped to mimic patients with non-specific symptoms where the site of cancer was uncertain. In addition, non-generative methods for data augmentation were investigated to improve the performance of machine learning.
The area under the receiver operating characteristic curve (AUROC) values were calculated for eight cancer types and symptomatic controls without cancer: Most classifiers achieved AUROC values above 0.85. The cancer vs. asymptomatic non-cancer classification detected 64% of stage I cancers with a specificity of 99% (overall sensitivity 57%). With a higher sensitivity, this model identified 99% of stage I cancers (with a specificity of 59%). For the colorectal cancer dataset, data augmentation with a WGAN resulted in an increase in AUROC from 0.91 to 0.96, demonstrating the impact of data augmentation on deep learning performance. The scientists conclude that this spectroscopic blood test can effectively detect cancer at an early stage and could facilitate the necessary earlier diagnosis.
Combined blockade for lung cancer
Although anti-PD-1/PD-L1 antibodies represent a major breakthrough in NSCLC therapy, the efficacy of this treatment is highly dependent on the tumor’s PD-L1 expression. The role of Id1 in lung adenocarcinoma and the efficacy of combined blockade of PD-1 and Id1 by RNA silencing in KRAS-mutated LUAD mouse models have already been reported. Trametinib, an oral MEK1/2 inhibitor, acts downstream of KRAS. Trametinib has now been investigated in a study as a pharmacological Id1 inhibitor that can improve the efficacy of immunotherapy through PD-L1 overexpression [3]. To analyze whether MEK1/2 inhibition reduces Id1 expression, in vitro and in vivo experiments were performed in NSCLC cells and in mouse models. RNAseq analysis was performed to elucidate the signaling pathways involved in Id1 inhibition. Apoptosis and PD-L1 expression were measured by flow cytometry. The synergy of the anti-PD1 combination of trametinib was investigated in KRAS-mutated LUAD models.
The experiments with KRAS-mutated NSCLC cells and mouse models showed an inhibition of Id1 after MEK1/2 blockade. Blocking proteasome activity with MG-132 restored Id1 levels. Trametinib-resistant (TR) cells showed no Id1 inhibition and silencing of Id1 restored sensitivity to trametinib in human and murine NSCLC TR cells. Flow cytometric analyses showed increased PD-L1 expression in NSCLC cell lines after trametinib administration. In contrast, Id1-overexpressing cells showed no PD-L1 upregulation after trametinib. In vivo experiments confirmed a synergistic therapeutic efficacy of the combination of trametinib and anti-PD-1, which reduced tumor growth and increased survival time of mice compared to trametinib or immunotherapy alone. In addition, the analysis of the immune population showed a significant increase in CD8+ T cells and a reduction in Treg cells in the tumors of the mice treated with the combination.
Treatment-related toxicity in UC
Enfortumab vedotin (EV) is approved for patients with advanced urothelial carcinoma (aUC), but the duration of treatment is often limited by toxicity. Therefore, patient characteristics and biomarkers associated with EV-related adverse events (EV AEs) were investigated [4]. UNITE is a multi-site retrospective study of aUC patients treated with EV. Patients who were treated with EV only and for whom AE and NGS (next generation sequencing) data were available were analyzed. EV-AEs were assessed according to CTCAE v5.0. For univariate analyses (UVA), Wilcoxon rank sum and chi-square tests were used to investigate associations between clinical characteristics or somatic genetic changes. Using Cox regression models, the GAs were evaluated individually in separate multivariate analysis models (MVA), taking into account relevant clinical factors.
Of 607 patients, 275 had EV AEs and NGS data. The median time from initial diagnosis to the onset of EV was 86 weeks, and the median time from the onset of EV to the appearance of SAR was 4 weeks. Most common SARs of all grades were neuropathy (46%), skin toxicity (41%), fatigue (25%), GI toxicity (22%), cytopenias (14%), anorexia (11%). In UVA, diabetes (DM), previous neuropathy, higher HgB and albumin at the onset of EV were associated with neuropathy. Hyperglycemia was associated with higher BMI, DM, lower NLR and male gender. These hypothesis-generating results suggest a limited role of somatic GA in predicting EV AEs and warrant further investigation of host- and tumor-related factors underlying EV toxicity.
Prognostic factor for pancreatic cancer
Sarcopenia and myosteatosis are associated with a poor prognosis. The Albumin Myosteatosis Gauge (AMG) is a novel integrated measure that has been proposed to assess myosteatosis along with serum albumin levels as a surrogate for systemic inflammation. The aim of one study was to investigate the prognostic value of AMG in patients with advanced pancreatic cancer (APC) [5]. Patients with APC who were treated with chemotherapy were evaluated. The skeletal muscle index (SMI) and skeletal muscle radiodensity (SMD) were calculated using computed tomography at the L3 level. The AMG was defined as SMD × albumin and expressed in arbitrary unit (AU). The patients were divided into two groups based on the gender-specific cut-off value for AMG. A total of 196 patients were included. At presentation, 79% of patients had metastatic disease and 21% had locally advanced disease. For the AMG value, 142.86 AU for men and 114.15 AU for women were defined as cut-off values. The patients with low AMG had a significantly worse OS than the patients in the high AMG group. In multivariable analyses, lower AMG scores, higher ECOG performance score and metastatic disease were associated with poorer OS. This study suggests a high prognostic value of AMG in patients with APC receiving first-line chemotherapy.
Literature:
- Huang J: Engineered salmonella blocks cancer metastasis by activating NK cells in an IFN-γ-dependent manner. E-Poster 7P. ESMO congress 2023.
- Baker MJ, et al.: A spectroscopic liquid biopsy for the earlier detection of multiple cancer types. E-Poster 1216P. ESMO congress 2023.
- Puyalto A, et al.: Trametinib and PD-1 combined blockade impairs tumor growth and improves survival of KRAS-mutant lung cancer through Id1 downregulation. E-Poster 2324P. ESMO congress 2023.
- Nizam A, et al.: Biomarkers of treatment (Tx)-related toxicity in advanced urothelial carcinoma (aUC) pts treated with enfortumab vedotin (EV): Analysis of UNITE study. E-Poster 2394P. ESMO congress 2023.
- Dizdar O, et al.: Albumin-myosteatosis gauge as a prognostic factor in patients with advanced pancreatic cancer undergoing first-line chemotherapy. E-Poster 1608P. ESMO congress 2023.
InFo ONKOLOGIE & HÄMATOLOGIE 2023: 11(6): 22–23