Case report: The 53-year-old, previously healthy woman was clarified by CT imaging due to a tripping fall with commotio. Here, no intracranial trauma sequelae were evident. However, a large right parieto-occipital mass was presented as an incidental finding, which was further characterized by MRI. Clinically neurologically our patient presented unremarkable.
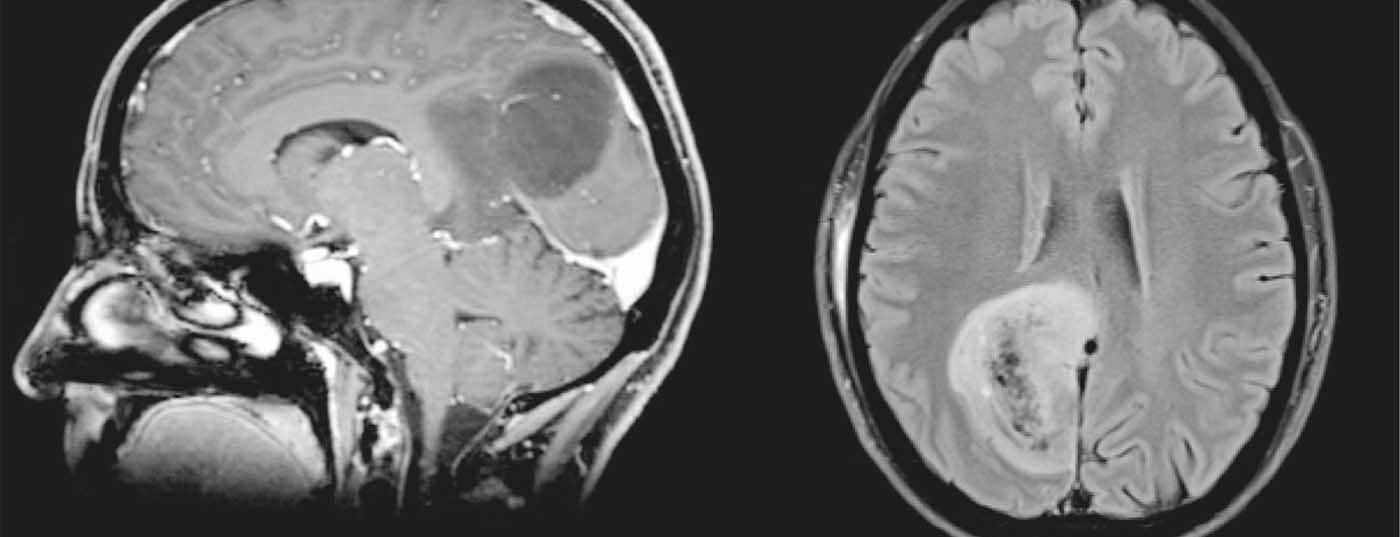
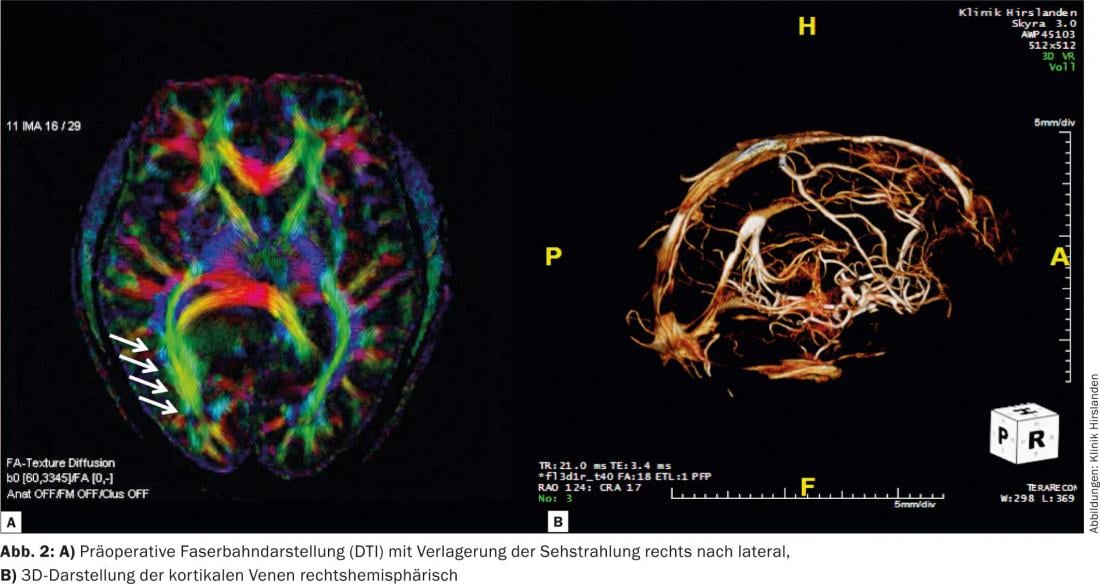
MRI diagnosis: T2 and FLAIR weighting reveals a 4×5×4 cm inhomogeneous hyperintense mass with cystic portions. In T1-weighted images after i.v. gadolinium administration, the hypointense mass shows no contrast enhancement (Fig.1) . Fiberoptic tract imaging (DTI) shows tumor-related displacement of visual radiation (Fig. 2a) without evidence of infiltration. 3D reconstruction of contrast-enhanced TOF angiography reveals no bridging veins relevant to an interhemispheric occipital access pathway (Fig. 2b). 1-H spectroscopy shows a strong decrease of the physiological nerve cell marker NAA and a moderate increase of the proliferation marker choline by 55% compared with the opposite side. In addition, a lactate peak, the marker for anaerobic glycolysis, can be seen. The image morphologic aspect resembles an oligodendroglioma, and the spectrum is suggestive of a grade III tumor.

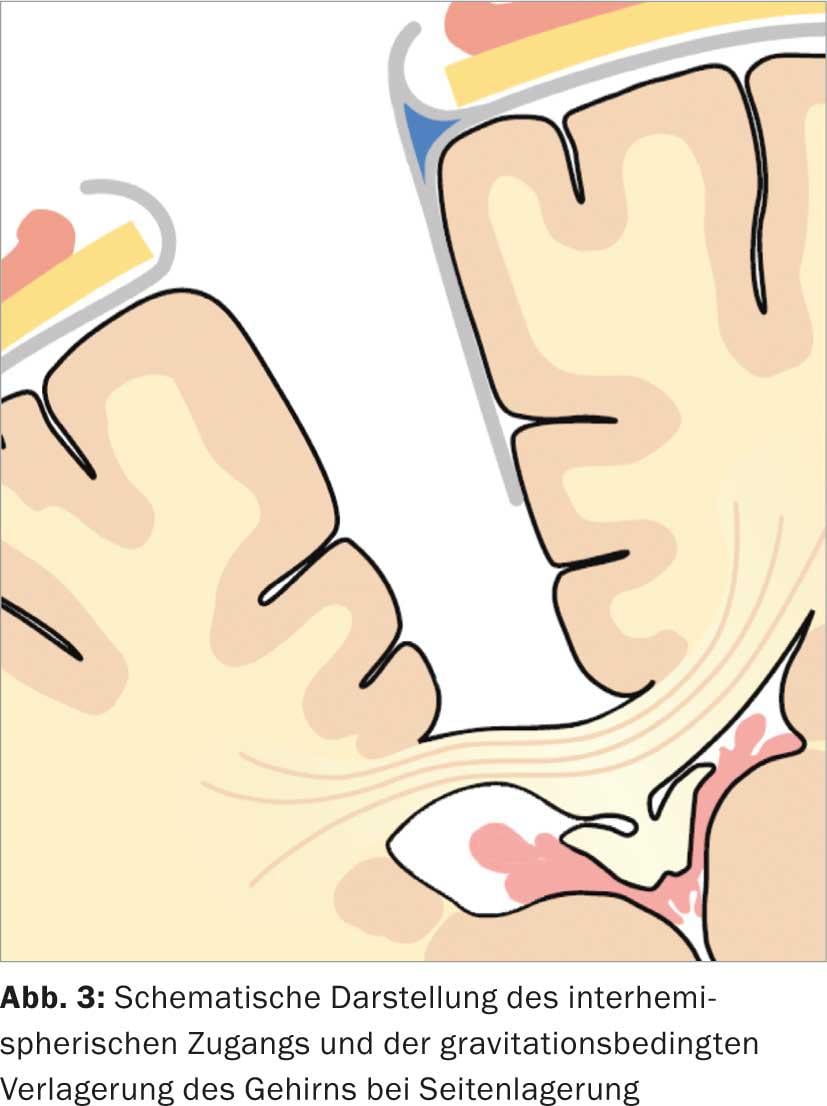
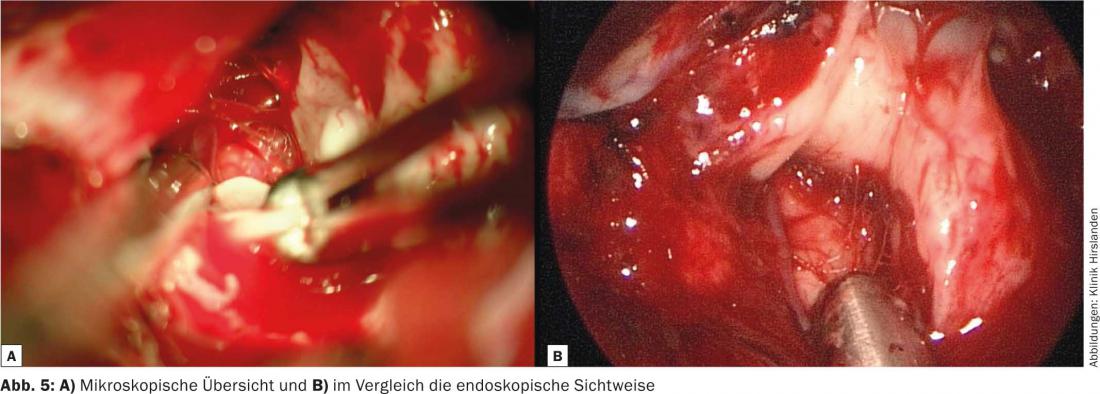
Surgery: To facilitate the surgical access route, our patient is positioned on the right side of the body. This causes a shift of the brain to the right, thus a traumatic brain retraction can be avoided (Fig. 3). After entering the interhemispheric space, the tumor is resected with endoscopic-assisted technique (Fig. 4). Using the neuroendoscope, the parts of the tumor that are not visible with the microscope can be viewed and removed. (Fig. 5a and b). Finally, resection control is performed with the aid of intraoperative MRI (iOP-Polstar). Contrast-enhanced T1-weighted sequence shows a suspicious approximately 0.5×0.5 cm lesion at the right lateral resection margin. The tumor-suspected lesion is subsequently resected. Thus, complete tumor resection was achieved. Extubation of the patient from anesthesia was smooth. The histopathological diagnosis is ana-
plastic oligoastrocytoma.

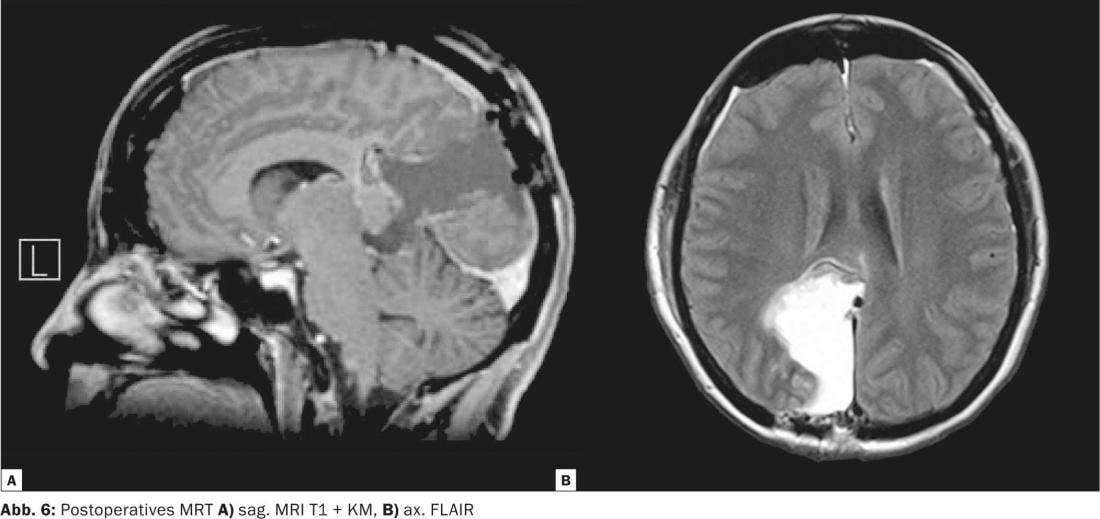
Postoperative course: On the following day, complete resection of the tumor was documented by MRI (Fig. 6) . Postoperatively, there was a minimal visual field defect on the left side; at discharge, the manipulation-related symptoms had completely disappeared.
CONCLUSION: Using multimodality tools such as accurate neuroradiologic imaging, use of targeted neuroendoscopy, and intraoperative resection control by iOR-MRI, complete removal of difficult-to-access tumors can be achieved. In our particular case, interdisciplinary teamwork was crucial to therapeutic success.