For negative symptoms, two main dimensions can be defined: Apathy (reduced drive, social withdrawal, joylessness) and reduced expression (impoverishment of speech, flattening of affect). Negative symptoms severely limit the everyday functioning and quality of life of patients with schizophrenia. For therapy and diagnostics, the distinction between primary and secondary negative symptoms is relevant. Treatment of primary negative symptoms is difficult and cognitive-behavioral, social psychiatric, medication, and alternative therapies should be explored and applied as appropriate.
Negative symptoms were already counted among the central symptoms of patients with schizophrenia in the times of Kraepelin and Bleuler, the latter describing them as a “lowering of the will drive.” To this day, negative symptoms have lost none of their importance, as they have a strong impact on patients’ level of functioning and quality of life. At the same time, treatment approaches are very limited.
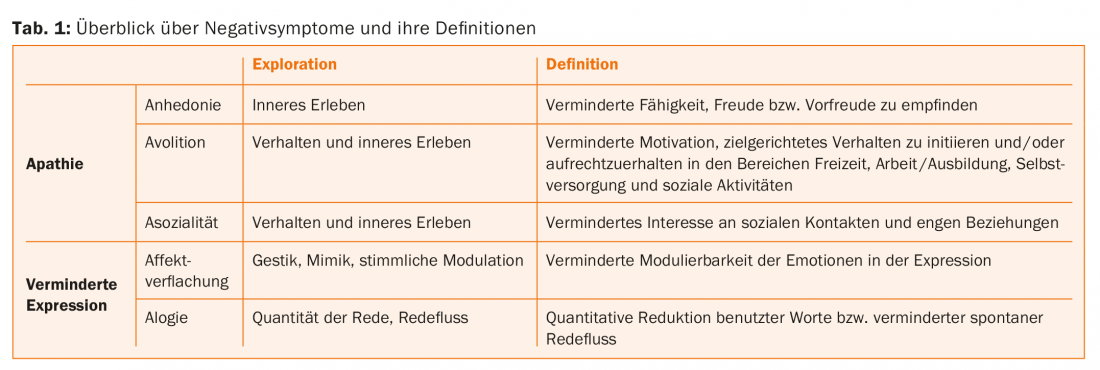
Although negative symptoms have played a role since the early days of schizophrenia research, it is only in the last decade that a clearer picture of their expression and significance has emerged. Two main dimensions can be defined (tab. 1): Apathy consists of reduced drive (avolition), social withdrawal (asociality), and joylessness (anhedonia), possibly mainly reduced memory and anticipation (expectation) of joyful events rather than effective experience in the moment. Reduced expression includes impoverishment of speech (alogy) as well as flattening of affect. The individual dimensions of apathy should be carefully inquired of the patient. The reduction in expressive abilities should be observed and included in an overall assessment in terms of severity and expression.
Distinction between primary and secondary negative symptoms
For therapy and diagnostics, the distinction between primary and secondary negative symptoms is relevant. Primary negative symptoms are considered part of the disease process of schizophrenia and are characterized by greater persistence over time and poorer treatability [1]. Secondary negative symptoms are due to effects of positive symptoms, depression, side effects of antipsychotic medication, or environmental factors such as social deprivation [2]. In the clinical exploration, it is important to carefully identify these secondary causes and, if necessary, to initiate appropriate interventions.
Secondary negative symptoms
An important cause of secondary negative symptoms is comorbid depression, which is common in patients with schizophrenia. However, the demarcation in clinical routine is often difficult. Psychopathological overlaps are evident in joylessness, listlessness, and reduced affect, which can be symptoms of depression as well as expressions of negative symptomatology. In the case of depression, depressed mood is often added as a cardinal symptom. Furthermore, typical depressive cognitions such as hopelessness, pathological guilt, and self-deprecation are absent from the negative symptoms. Equally less pronounced are vegetative symptoms such as palpitations, sweating or gastrointestinal complaints as well as circadian rhythms with morning or evening lows [3].
Because studies are insufficient and clear treatment recommendations for depression in patients with schizophrenia are lacking, each case must be assessed individually. However, targeted treatment for depression should also be considered in borderline cases. Psychopharmacologically, there is evidence for an antidepressant effect of atypicals that exceeds that of typicals. The use of antidepressants must be judged on a case-by-case basis and may potentially result in additional benefit [4]. In all cases, pharmacotherapy should be supplemented by depression-specific psychotherapy.
Positive symptoms can also lead to social withdrawal due to experiences of persecution and impairment and resulting anxiety and fear. A whole series of studies proves that negative symptoms are reduced under antipsychotic medication in parallel with positive symptoms [5]. If negative and positive symptoms are present at the same time, antipsychotic medication should be adjusted. In this case, a dose increase or a change of the preparation may be useful. If positive symptoms (and secondary negative symptoms) are resistant to treatment with medication, the indication for clozapine should be considered in all cases. Cognitive behavioral therapy has also been shown to be effective for treating treatment-resistant positive symptoms in combination with antipsychotics [6].
However, antipsychotics may not only lead to an improvement of negative symptoms by reducing positive symptoms, but may also cause them secondarily due to their side effect profile [1]. Of relevance here are extrapyramidal side effects, which can lead to flattening of affect and reduced drive as a result of motor impairment. If akinesia occurs during treatment, consider dose reduction or switching to another drug with lower risk of extrapyramidal side effects. A second potential side effect that may impact negative symptoms is sedation. In this context, the temporal relationship between the start or increase of medication and the occurrence of negative symptoms, as explained by the patient, plays a particularly important diagnostic role. If a reduction in drive due to sedation from the antipsychotic medication can be assumed, a dose reduction or switch to another drug with a lower risk for sedation should be considered.
For the diagnosis of secondary negative symptoms due to social deprivation, an exact survey of the environmental conditions including external anamnesis is necessary. A promising treatment approach is the expansion of activity options, for example in day clinics, low-threshold meeting places, with psychosocial Spitex, work in a sheltered area or living in an assisted living facility. The patient’s level of functioning must be taken into account so as not to create frustration experiences by overtaxing, which may result in additional withdrawal.
Amotivational syndrome and joylessness can also occur in the context of substance use. Cannabis and other substances play an important role. In this case, concepts for the treatment of comorbid substance disorders such as psychoeducation, motivational interviewing as well as behavioral therapy approaches should be applied.

Primary negative symptoms
If no secondary factors are found for the development of negative symptoms, a primary event, due to the disease process, can be assumed. Treatment of primary negative symptoms is difficult, and no clear treatment recommendations can be made based on the current state of studies. However, this should not prevent one from examining the various therapeutic options in individual cases and making appropriate suggestions to the patient.
Cognitive-behavioral therapy studies with the primary endpoint of positive symptoms did show a reduction in negative symptoms, but whether this effect was specific or due to a reduction in productive symptoms cannot be separated [7]. Only two cognitive-behavioral therapy randomized controlled trials examined negative symptoms as a primary endpoint. In the study by Klingberg et al. showed no advantage for cognitive behavioral therapy compared with cognitive training, with both groups improving over the course of the study [8].
Of interest to practitioners are recent findings that underscore the importance of dysfunctional beliefs in the development of negative symptoms. Limited performance and impairments in the context of psychosis result in setbacks and experiences of frustration, which in turn promote dysfunctional beliefs, low self-esteem, and diminished belief in future success. In a study by Grant et al. a significant reduction in listlessness was achieved through targeted restructuring of these beliefs and attitudes, but the intervention had no effect on joylessness and reduced expression [9].
In practice, the recommendation is therefore to explore the individual symptom dimensions in detail, to record the underlying cognitions, and to address these in a targeted manner using cognitive-behavioral therapy. Among other things, keeping diaries and agreeing on specific weekly goals have proven effective. Here, too, it is important to adapt the tasks to the patient’s functional level in order not to generate further frustration experiences through new setbacks.
Psychopharmacologically, atypicals appear to reduce negative symptoms compared with placebo, but most studies made no distinction between primary and secondary negative symptoms. For the treatment of primary negative symptoms, there is evidence for the efficacy of amisulpride (up to 300 mg) and olanzapine (up to 5 mg) over placebo. In addition, augmentation therapy with an antidepressant (e.g., fluoxetine or trazodone) appears to have a moderate effect on reducing prominent negative symptoms, although again this is not specific for primary negative symptoms [10]. Studies that have attempted to treat negative symptoms as a primary endpoint, including modulation of NMDA receptors or stimulants, have not yet yielded a significant positive effect.
Lastly, alternative therapies such as animal-assisted therapy (e.g., with dogs), body-oriented therapies (dance and movement, physical therapy), and music therapies should be mentioned. In individual cases, these can also lead to an improvement in symptoms.
Conclusion
Overall, the treatment of negative symptoms continues to be a major challenge. The division into primary and secondary negative symptoms facilitates a pragmatic approach, but remains under scientific debate. A stepwise approach with initial recording and treatment of secondary negative symptoms seems reasonable. Treatment of primary negative symptoms is difficult, and cognitive-behavioral, social psychiatric, medication, and alternative therapies should be considered and applied on a case-by-case basis.
The differentiation of primary and secondary negative symptoms is a great challenge in practice and often mixed pictures appeared, which make an exact differentiation difficult. Considering the fact that the symptoms cause great losses in everyday function and quality of life, the detailed exploration and individualized treatment is worthwhile in any case.
Literature:
- Kirkpatrick B, Galderisi S: Deficit schizophrenia. an update. World Psychiatry. Official Journal of the World Psychiatric Association (WPA) 2008; 7(3): 143-147.
- Kirkpatrick B: Developing concepts in negative symptoms. Primary vs secondary and apathy vs expression. The Journal of Clinical Psychiatry 2014; 75 Suppl 1: 3-7.
- Lako IM, et al: (2012). A systematic review of instruments to measure depressive symptoms in patients with schizophrenia. J of Affective Disorders 2012; 140(1): 38-47.
- Hasan A, et al: Guidelines for Biological Treatment of Schizophrenia Part 3. Update 2015 Management of special circumstances. Depression, suicidality, substance use disorders and pregnancy and lactation. World J Biol Psychiatry 2015; 16: 142-170.
- Chen L, et al: The longitudinal interplay between negative and positive symptom trajectories in patients under antipsychotic treatment. A post hoc analysis of data from a randomized, 1-year pragmatic trial. BMC Psychiatry 2013; 13: 320.
- Burns MN, et al: Cognitive-behavioral therapy for medication-resistant psychosis. A meta-analytic review. Psychiatric Services 2014; 65(7): 874-880.
- Wykes T, et al: Cognitive behavior therapy for schizophrenia. Effect sizes, clinical models, and methodological rigor. Schizophrenia Bulletin 2008; 34(3): 523-537.
- Klingberg S, et al: Negative symptoms of schizophrenia as primary target of cognitive behavioral therapy. Results of the randomized clinical TONES study. Schizophrenia Bulletin 2011; 37 Suppl 2: S98-110.
- Grant PM, et al: Randomized trial to evaluate the efficacy of cognitive therapy for low-functioning patients with schizophrenia. Arch Gen Psychiatry 2012; 69(2): 121-127.
- Arango C, et al: Pharmacological approaches to treating negative symptoms. A review of clinical trials. Schizophrenia Research 2013; 150(2-3): 346-352.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(2): 4-7.











