TIA and stroke patients with advanced intracranial stenoses should generally not be stented – according to a 2016 G-BA decision. A recent randomized trial [1] shows: clinically stable patients do not benefit from the intervention. However, the benefit of stenting in high-risk patients remains open. According to the G-BA, affected individuals “qualify” for the use of stents by having a second event. According to DGN experts, this can sometimes be too late – a more precise patient selection is needed in order to be able to give those affected a preventive therapy in time.
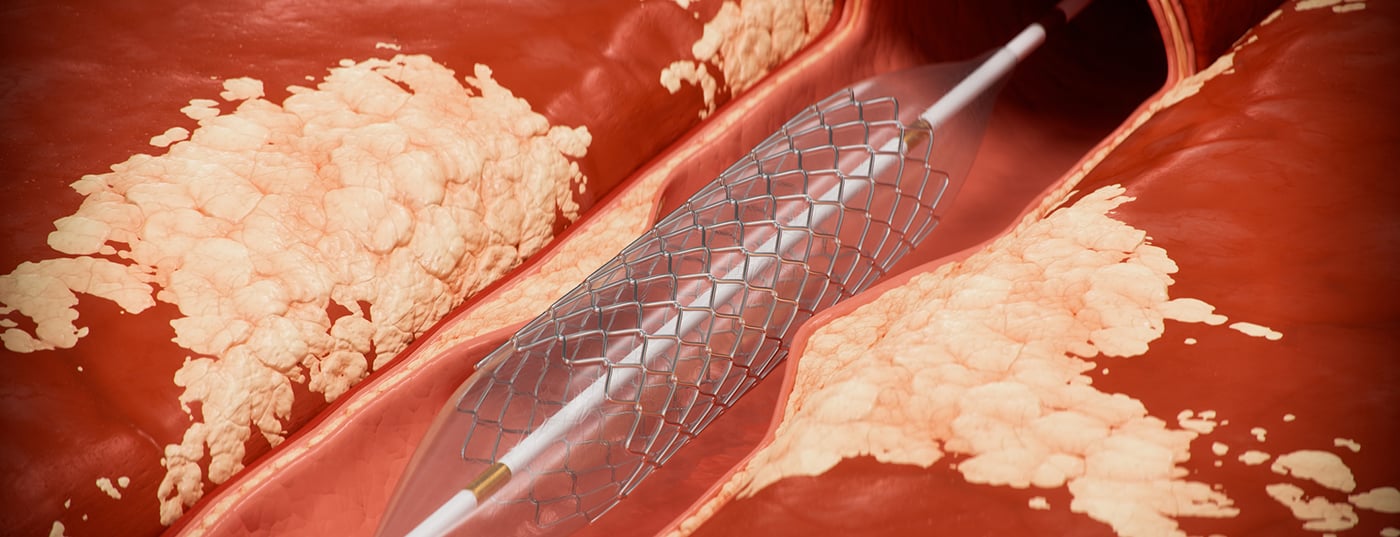
A possible cause of ischemic stroke is so-called atherosclerotic intracranial stenoses. These are constrictions of the vessels within the skull due to deposits of fats such as cholesterol in the inner layer of the vessel walls. Colloquially, the term “vascular calcification” is often used. The storage of fats and other substances in the vessel walls constricts the vessels – to the point of occlusion. In “people of color” and in people of Asian origin, one third of all ischemic strokes are due to atherosclerosis localized here. In Caucasians, atherosclerotic stenoses in the brain were found in 12% of all who suffered an ischemic stroke or an “ischemic mini-stroke” called a transient ischemic attack (TIA), especially in the elderly.
The consideration to provide these patients with stents in addition to drug prophylaxis (dual platelet inhibition) to prevent secondary strokes, in order to keep the vessels permanently open even after an acute ischemic stroke, thus had a comprehensible rationale. However, in 2014/2015, several randomized trials, including SAMMPRIS [2] and VISSIT [3], then led to doubts about the effectiveness of intracranial stents for secondary prevention of stroke in symptomatic intracranial stenosis. The stented patients had a worse outcome. The German Stroke Society, the Professional Association of German Neuroradiologists (BDNR), the German Society of Neuroradiology (DGNR) and the DGN criticized these studies at the time [4]: Thus, affected persons with an unstable neurological condition who might require acute intervention had been explicitly excluded. The hemodynamic relevance of vasoconstriction was also not considered. The professional societies took the position that the data situation speaks against an unselective, but not generally against the use of this treatment method. In 2016, the Federal Joint Committee (G-BA) decided to largely exclude the use of stents in the treatment of patients with intracranial stenosis [5].
The current study reported here [1] included only TIA and stroke patients with advanced intracranial stenoses (70-99 luminal narrowing). However, again, these were affected individuals in whom the ischemic stroke had not resulted in relevant clinical impairment (Modified Rankin Score of 0-2). The old studies also included only patients who were clinically stable.
In the current study, 358 affected individuals were randomized to receive either dual antiplatelet therapy or interventional stenting by neuroradiologists in addition to this drug therapy. The primary endpoint included the risk of subsequent stroke and/or death and it was found that there was no significant difference between the two treatment groups in this regard (8.0% vs. 7.2%; p= 0.80). The study groups also did not differ with regard to secondary end points, including the occurrence of subsequent strokes in the area of the stenosis. In addition, there was a trend toward increased mortality in the intervention group. The 3-year mortality was 4.4% in the stent group and 3.2% in the conventionally treated group (p=0.08).
“The result confirms that of studies that appeared eight years ago and shows: In patients with intracranial stenoses who are in a clinically stable condition and whose stenoses thus have no hemodynamic relevance, stents provide no additional benefit – and again we can conclude that interventional procedures should not be performed in an unselected manner. As then, however, we must again state: There are indications in which intervention may nevertheless be justified,” explains Professor Dr. Hans-Christoph Diener, press spokesman of the DGN. As the expert continues, this is the case, for example, with strokes triggered by hemodynamically relevant stenoses that prove resistant to drug treatment. This means that despite antithrombotic therapy, further TIAs or another ischemic stroke will occur. The G-BA also sees an indication for stent implantation in patients with an intracranial stenosis with a degree of stenosis of at least 70% who have suffered at least one further infarction after a stenosis-related infarction despite subsequent intensive drug therapy.
“Of course, studies that examine the benefits and risks of stent implantation in more detail are desirable – but not treating affected individuals with progressive neurological symptoms at all because of a lack of data and waiting until a subsequent event occurs still seems questionable to us,” Diener said. “We therefore need more precise patient selection in order to be able to get those affected into treatment in a timely manner.”
DGN Secretary General Professor Dr. Peter Berlit adds: “The present study has confirmed what we know, but has not investigated the open question of the extent to which high-risk patients benefit from early intervention. A second event should be prevented and not waited for as an indication criterion. What is also certain is that the data in no way support the general exclusion of the use of stents in inpatients with intracranial stenosis.”
Literature
[1] Gao P, Wang T, Wang D, et al. Effect of Stenting Plus Medical Therapy vs Medical Therapy Alone on Risk of Stroke and Death in Patients With Symptomatic Intracranial Stenosis: The CASSISS Randomized Clinical Trial. JAMA. 2022;328(6):534-542. doi:10.1001/jama.2022.12000
[2] Derdeyn C, Chimowitz M, Lynn M et al. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet 2014; 383: 333-341
[3] Zaidat O, Fitzsimmons B, Woodward B et al. Effect of a balloon-expandable intracranial stent vs. medical therapy on risk of stroke in patients with symptomatic intracranial stenosis – rhe VISSIT randomized clinical trial. JAMA 2015; 3013: 1240-1248
[4] Benefit assessment of stents for the treatment of symptomatic intracranial stenosis.
Commentary on the Rapid Report of the Institute for Quality and Efficiency in Health Care (IQWiG) by BDNR, DGNR, DGN, and DSG. Available at https://www.dsg-info.de/nachrichten/stellungnahmen-der-dsg/421-nutzenbewertung-v…
[5] G-BA decision: Guideline Methods Hospital Treatment:Use of stents for the treatment of intracranial arterial stenoses. Date of decision: 15.09.2016, available at https://www.g-ba.de/beschluesse/2718/
Original publication:
doi:10.1001/jama.2022.12000