Metabolites in serum, urine and stool samples can identify those with acute-on-chronic liver failure among patients with acute decompensated liver cirrhosis as a basis for early diagnostic and therapeutic measures. This is the conclusion of a current study project. In a project by another research team, the “EXSISERS” reporter system provided interesting insights into the relevance of p53 status in spontaneous bacterial peritonitis, an infectious complication associated with liver cirrhosis.
Advanced liver fibrosis and cirrhosis are summarized as “advanced chronic liver disease” (ACLD). Advanced chronic liver disease is characterized by persistent damage and increasing scarring of the liver. The final stage of liver fibrosis is liver cirrhosis. Patients with cirrhosis with acute decompensation (AD) have an increased risk of developing acute-on-chronic liver failure (ACLF). ACLF is characterized by extrahepatic organ failure and systemic inflammation. ACLF is associated with a serious risk of infectious complications and high short-term mortality. In order to improve the prognosis of affected patients, early diagnostic and therapeutic measures are required in ACLF [1]. Dechaumet et al. presented a research project at this year’s EASL congress in which metabolomic signatures were identified to differentiate between AD patients with or without ACLF. The following is a summary of this and another research project in the field of advanced liver disease [2,3].
Analysis of data from the MUCOSA-PREDICT cohort
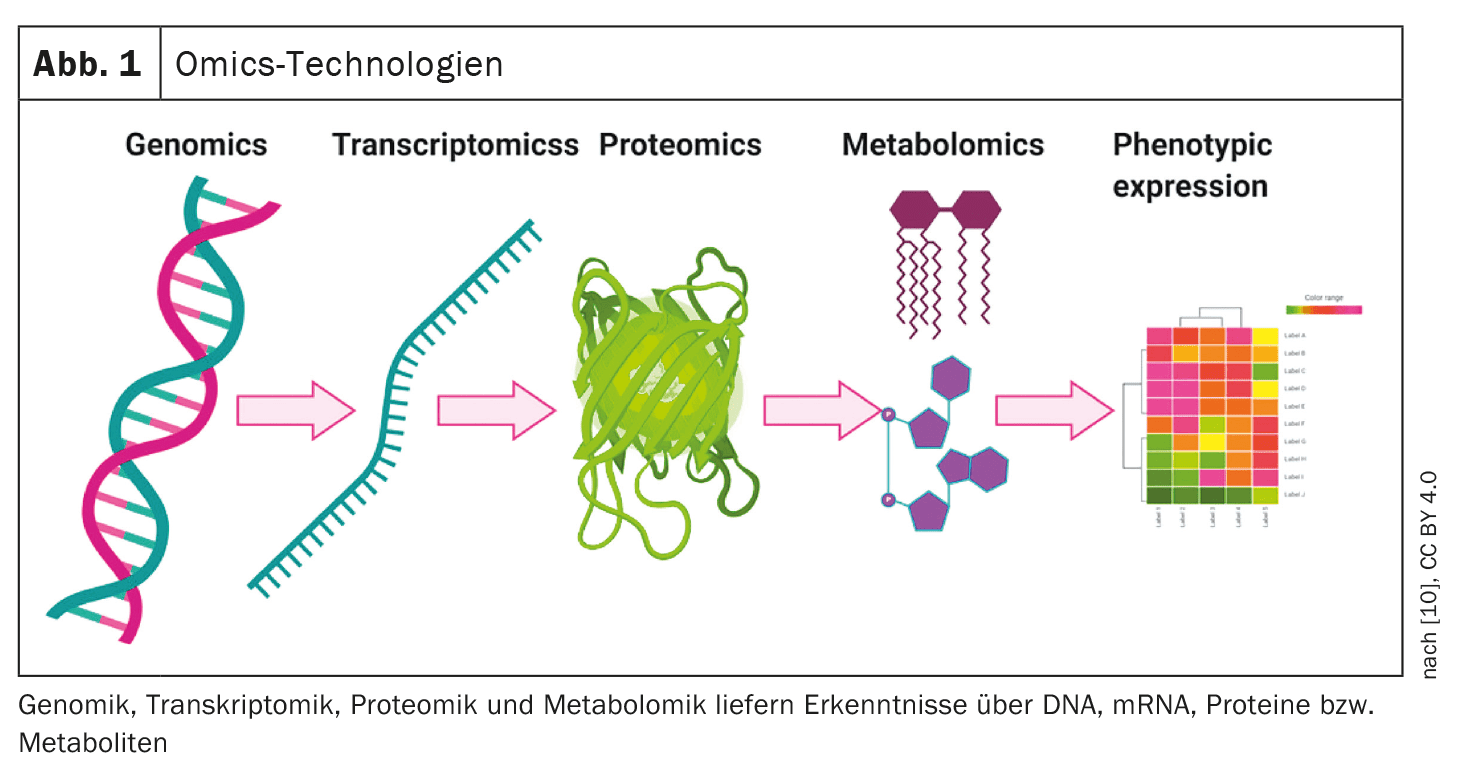
The entirety of low-molecular substances (metabolites) is called the metabolome. The metabolome can be measured by chromatography, mass spectrometry or nuclear magnetic resonance spectroscopy, for example. The liver is a metabolically highly active organ and liver diseases are increasingly being researched using multi-omics methods (Fig. 1) [10]. Moreau et al. reported in 2020 in the Journal of Hepatology that they were able to identify an ACLF-specific fingerprint of 38 metabolites in the blood using a multi-omics approach in tissue samples, which correlates with systemic inflammation and acts as an indicator of mitochondrial dysfunction in peripheral organs [4].
Study objectives and methodology: The project by Dechaumet et al. aimed to, (i) investigate whether the analysis of metabolites in urine and stool samples has added value for the characterization of the metabolome in decompensated cirrhotic patients and (ii) to evaluate how multimatrix metabolomics contributes to improving the stratification of patients with decompensated cirrhosis [2]. To this end, the researchers analyzed serum, urine and stool samples from the MUCOSA-PREDICT cohort, in which 93 cirrhotic patients with acute decompensation are followed up, using liquid chromatography coupled with high-resolution mass spectrometry. A total of 402 metabolites were detected and identified in the three biological matrices.
Results: The largest number of metabolites whose concentrations are affected by ACLF was observed in serum samples [2]. Interestingly, the concentrations of some metabolites in urine and feces that were not detected in serum were also found to be affected by ACLF. However, ROC curve analyses performed for the metabolomics signatures in single or combined matrices showed that the serum signature performed best in discriminating between AD and ACLF. This is a clinically relevant finding, as both clinical pictures overlap in individual cases, but are different entities in terms of pathophysiology and therapy.
Implementation of the “EXSISERS” reporting system
The gut-liver axis describes the diverse interactions between the gut and liver, including the exchange of cellular and molecular components, and is of central importance for the regulation of essential (patho)physiological processes. Patients with liver cirrhosis have reduced mucosal thickness, which facilitates direct contact of bacteria with epithelial cells and the degradation of cellular compounds [5]. Bacterial translocation is considered a crucial step in the pathogenesis of bacterial infections [6]. For example, translocation of intestinal bacteria into mesenteric lymph nodes is a key event in spontaneous bacterial peritonitis. Spontaneous bacterial peritonitis** is an inflammation of the ascitic fluid that occurs particularly frequently in liver cirrhosis and can have serious consequences.
** The most common bacteria that cause spontaneous bacterial peritonitis are Gram-negative Escherichia coli and Klebsiella pneumoniae and Gram-positive Streptococcus pneumoniae [11].
Study objectives and methodology: According to Ernst et al. the cellular stress triggered by direct contact with the bacteria affects the p53 family of transcription factors, which act as key regulators of the cell cycle, repair mechanisms and cell death (apoptosis) [3]. In its wild-type form, p53 (wtp53) acts as a central tumor suppressor [7]. The structurally and functionally homologous proteins p63 and p73 are subsumed into the p53 family of transcription factors. The function of p53 is altered in a large number of tumors (TP53 mutations). In their study, Ernst et al. investigated the effects of ascites bacteria on the expression of p53 isoforms$ in relation to the induction of cell death in epithelial cells. They applied a novel biotechnological reporter system [3]. The reporter system called EXSISERS can track the expression of isoforms over time in living cells [8].
$ Isoforms are variants of proteins that arise from a single gene.
Three exon-specific intein luciferase reporter systems (EXSISERS) have been integrated into exons 2, 4 and 7 of the TP53 gene. Cleaved inteins allow the cleavage of the enzyme luciferase from the p53 polypeptide while maintaining the structural integrity of the p53 isoforms [9]. This method can be used to precisely quantify the ratios of p53 protein isoforms at the cellular level. HCT116-EXISERS cells were co-cultured with patient-derived Escherichia coli , and the three major groups of p53 isoforms – full-length cell cycle arrest-inducing p53, cell death-inducing Δ40p53, pro-proliferative Δ133p53/Δ160p53 – were measured. At the same time, bacterial-induced cell death was quantified in HCT116 p53 wild-type and p53 knockout cells. Electron microscopy was used to determine the type of cell death.
Results: Co-cultivation of patient-derived bacteria with HCT116-EXISERS cells initially led to increased production of the cell death-inducing p53 isoform Δ40p53 within 15 minutes [3]. This was followed by a decrease in the pro-proliferative p53 isoforms Δ133p53/Δ160p53. At the same time, apoptosis was observed in response to bacterial contact, which showed morphological features of paraptosis, including mitochondrial swelling and cytoplasmic vacuolization. In parallel to the observed morphological changes, flow cytometry confirmed mitochondrial and plasma membrane damage. The known paraptosis inhibitor acinomycin D efficiently blocked bacterial-induced cell death. In agreement with the measured induction of the Δ40p53 isoform, the induction of cell death was significantly delayed by a CRISPR/Cas9-mediated p53 knockout.
| Summary |
| In liver cirrhosis with acute decompensation (AD), the risk of developing acute-on-chronic liver failure (ACLF) is increased. In the study by Dechaumet et al. showed that metabolic signatures from the blood, but also from urine and faeces, differentiate between AD patients with and without ACLF. The data obtained from the blood compartment appears to provide the best stratification performance. |
| In patients with liver cirrhosis, bacterial translocation occurs due to impaired epithelial integrity. The cellular responses to bacterial stress are regulated by specific p53 isoforms. The study by Ernst et al. shows that the p53 status exerts a decisive influence on susceptibility to paraptosis. Targeted induction or stabilization of specific p53 isoforms could therefore represent a therapeutic option for the treatment of spontaneous bacterial peritonitis. |
| to [2,3] |
Congress: EASL Congress 2024
Literature:
- Hübener P, Braun G, Fuhrmann V: Med Klin Intensivmed Notfmed 2018; 113(8): 649-657.
- Dechaumet S, et al: Multi-compartment metabolomics for stratifying cirrhotic patients with acute decompensation, WED-083, EASL Congress, Milan, June 5-8, 2024.
- Ernst M, et al: Liver cirrhosis and epithelial damage – The gut-liver axis in spontaneous bacterial peritonitis and its modulation by p53, WED-106, EASL Congress, Milan, June 5-8, 2024.
- Moreau R, et al: J Hepatol 2020; 72: 688-701.
- Haderer, M. et al: Gut 2022; 71: 580-592.
- Rayes N: Experimental and clinical investigation of the influence of pre- and probiotics on bacterial translocation and postoperative infections after abdominal surgery, Habilitationsschrift, 2004, https://core.ac.uk,(last accessed 27.08.2024)
- Weilbacher A: The role of p53 status for the sensitivity of tumors to different p53 activators, Dissertation, 2017, https://elib.uni-stuttgart.de,(last accessed 27.08.2024) .
- “New designer proteins make isoforms non-invasively visible”, Helmholtz Munich, 04.06.2021.
- Truong, D-JJ, et al: Non-Invasive and High Throughput Interrogation of Exon-Specific Isoform Expression. Nature Cell Biology 2021, doi:10.1038/s41556-021-00678-x
- Raja G, et al.: Recent Advances of Microbiome-Associated Metabolomics Profiling in Liver Disease: Principles, Mechanisms, and Applications. International Journal of Molecular Sciences 2021; 22(3): 1160. www.mdpi.com/1422-0067/22/3/1160#, (letzter Abruf 27.08.2024)
- “Spontaneous Bacterial Peritonitis (SBP),” Danielle Tholey, MD, www.msdmanuals.com/de,(last accessed 8/27/2024).
HAUSARZT PRAXIS 2024; 19(9): 38-39 (published on 18.9.24, ahead of print)