Breast cancer is as heterogeneous as the patients affected. The forecast varies accordingly. Several analyses have now examined the impact of, for example, autoimmune diseases or socioeconomic status on overall survival. In addition, progression-free survival and time to next line of therapy were assessed under real-world conditions.
Patients with autoimmune diseases – particularly systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and Sjogren’s syndrome – have a lower risk of developing breast cancer than patients without a history of autoimmune disease. Therefore, little attention has been paid to this clientele and little is known about survival of patients with concurrent autoimmune disease and breast cancer. Therefore, a retrospective analysis compared outcomes in patients with breast cancer with and without autoimmune disease [1]. Data are based on SEER-Medicare databases from 2007-2014 with breast cancer. Patients with a history of autoimmune disease were identified by ICD-9 codes. The effects of autoimmune disease on overall survival (OS) and cancer-specific survival (CSS) were estimated using multivariable Cox regression and Gray’s method, respectively, controlling for the effects of age, race, and chronic kidney disease (CKD). Cumulative CSS was estimated, with death considered as a competing risk.
The overall prevalence of autoimmune diseases studied among the 137 324 patients with breast cancer was 26.69%. The most frequently identified autoimmune diseases were RA (23.35%), psoriasis (2.41%), and SLE (1.12%). In stage IV breast cancer patients, OS and CSS were significantly higher in patients with autoimmune disease (p-values <0.0001), with a median OS of 36 months compared to 30 months in patients without autoimmune disease. After adjusting for the effects of age, race, and CKD, autoimmune disease remained predictive of higher OS (HR: 1.46, 95% CI: 1.37-1.57, p<0.0001) and CSS (HR: 1.39, 95% CI: 1.29-1.5, p<0.0001). Patients with autoimmune disease and stage I-III breast cancer had lower OS (p<0.0001, p<0.0001, and p=0.026, respectively) compared to patients without autoimmune disease.
The researchers found a higher prevalence of RA, Crohn’s disease, ulcerative colitis, and SLE in patients with breast cancer compared with cohorts of similar age groups in the general population. A history of autoimmune disease significantly improved OS and CSS in patients with stage IV breast cancer, even after accounting for age, race, and CKD in this pre-immunotherapy cohort. These results suggest that anti-tumor immunity plays an important role in late-stage breast cancer and could potentially be used to improve the efficacy of immunotherapy. Further investigation into the association between autoimmunity and breast cancer is warranted.
Tell me where you come from
Socioeconomic status (SES) and ethnicity are important determinants of health outcomes-particularly in the United States. Therefore, the effects of SES, as measured by the Neighborhood Deprivation Index (NDI), and race on treatment outcomes of patients with metastatic breast cancer were examined in more detail [2]. To do this, NDI scores for 1246 patients with metastatic breast cancer between 2000 and 2017 were obtained from the Neighborhood Atlas based on their zip code. SES groups were defined as low deprivation with an NDI score in the lower tertile and high deprivation with an NDI in the upper or middle tertile. Baseline characteristics were compared between SES groups after Bonferroni correction. Univariate and multivariate survival analyses were performed with the R packages “survival” and “survminer.” Race was found to be the only baseline characteristic that differed significantly between SES groups. The high deprivation group had a higher proportion of African Americans (10.5%) than the low deprivation group (3.7%). In univariate Kaplan-Meier survival analysis, both social status and race had a significant effect on overall survival, such that the high deprivation group had worse survival than the low deprivation group and African Americans had worse survival than Caucasians. In the multivariate Cox proportional hazard model, social status, but not race, had a significant effect on overall survival. Progression-free survival after first-line chemotherapy did not differ between SES groups or racial groups in both univariate and multivariate analyses.
The current study shows that patients from the high deprivation group (i.e., low SES) have poorer survival in metastatic breast cancer. Race was no longer a significant predictor of survival when SES was included in the analysis. This may suggest that the poorer survival in the African American population is explained by the association between low SES and African American race, experts said.
Real-world endpoints in focus
Real-world progression-free survival (rwPFS) and time to next line of therapy (TTNT) are two endpoints of clinical interest in patients with metastatic breast cancer (MBC). However, their validation as intermediate endpoints for overall survival (OS) in a real-world setting had not yet been fully elucidated. Therefore, a retrospective cohort study was conducted using the US nationwide de-identified Flatiron Health database derived from electronic health records [3]. The study population included patients diagnosed with MBC between January 1, 2011 and February 30, 2021. rwPFS was defined as the time from initiation of first-line systemic therapy for MBC to disease progression or death. TTNT was defined as the time from the start of first-line systemic therapy to the start of the next line of therapy.
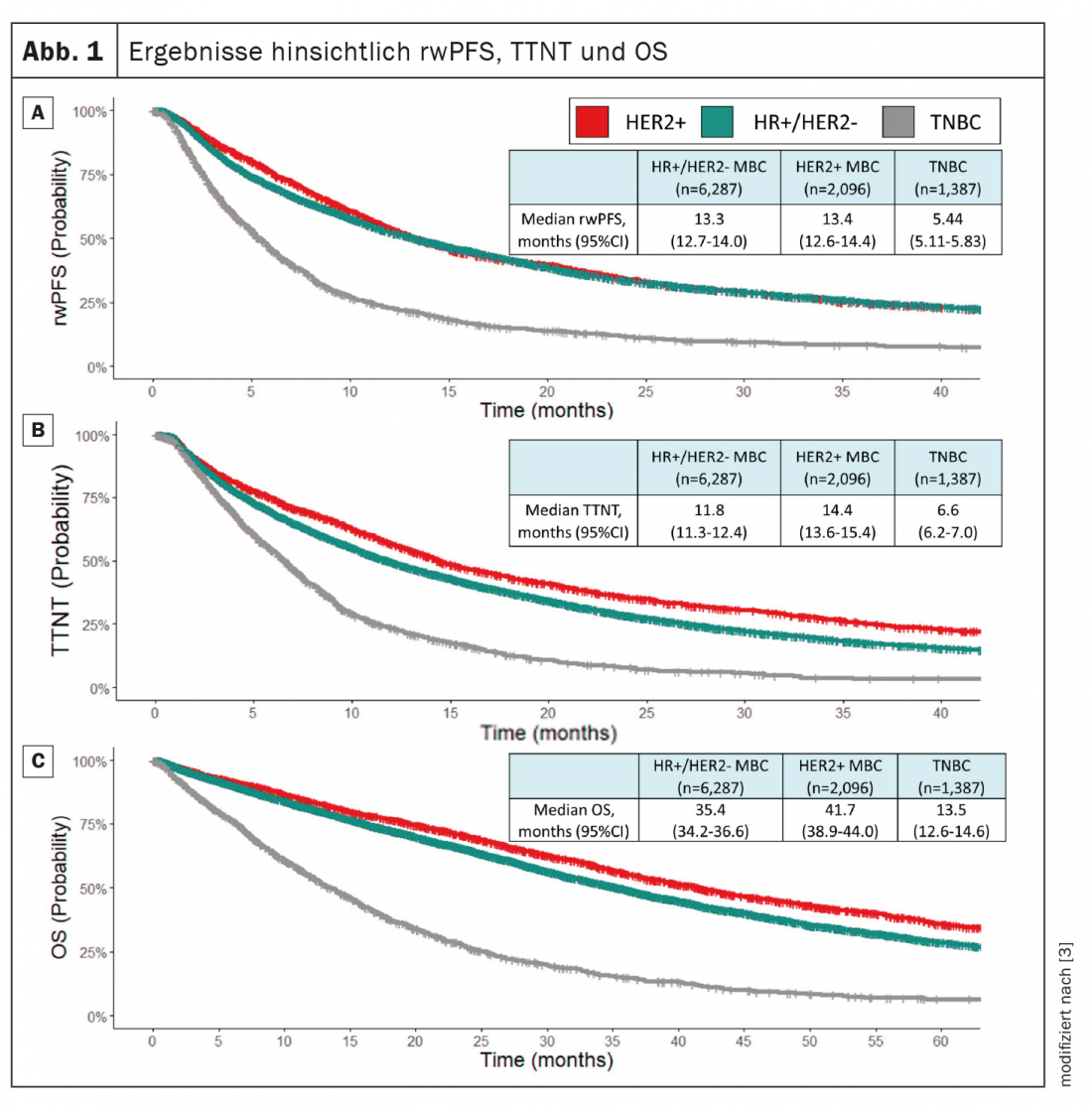
A total of 9770 patients with MBC were included. HR+/HER2 disease was the most common MBC subtype (64.4%), followed by HER2+ (21.5%) and triple-negative disease (14.2%). The median OS in the overall population was 32.4 months. The median rwPFS was 11.5 months and the median TTNT was 11.1 months. In the whole population, the correlation between rwPFS and OS was 0.54 (95% CI: 0.53-0.56), while the correlation between TTNT and OS was 0.47 (95% CI: 0.46-0.48). The investigators conclude that rwPFS and TTNT may represent meaningful intermediate endpoints for OS in patients with MBC overall and within different disease subgroups (Fig. 1).
Congress: ASCO Annual Meeting
Literature:
- Dedousis D, Zhang A, Vassiliou A, et al: Survival in patients with breast cancer and history of autoimmune disease. J Clin Oncol 40, 2022 (suppl 16; abstr 1020).
- Puthanmadhom Narayana S, Rosenzweig MQ, Ren D, et al: Effect of socioeconomic status as measured by Neighborhood Deprivation Index on survival in metastatic breast cancer. J Clin Oncol 40, 2022 (suppl 16; abstr 1013).
- Labaki C, Bakouny Z, Sanglier T, et al: Real-world progression-free survival (rwPFS) and time to next line of therapy (TTNT) as intermediate endpoints for survival in metastatic breast cancer: A real-world experience. J Clin Oncol 40, 2022 (suppl 16; abstr 6520).
InFo ONCOLOGY & HEMATOLOGY 2022; 10(3): 22-23 (published 6/20/22, ahead of print).