The national S3 care guideline on bronchial asthma in Germany was updated in 2020. This guideline also has acceptance in Switzerland and has a very high level of evidence, but is designed for broad care among primary care physicians and non-specialists. For pneumological specialists, however, there are also aspects that are not included in the NVL. A specialist S2k guideline on the diagnosis and treatment of asthma has now been developed for them and will be published in March 2023.
Type 2 biomarkers are becoming increasingly important in the diagnosis of asthma. According to GINA, indications for the presence of type 2 inflammation are given if the number of eosinophilic granulocytes in the blood is ≥150/μl and/or the nitric oxide in the exhalate (FeNO) is ≥20 ppb and/or the eosinophilic granulocytes in the sputum are ≥2% and/or there is clinical evidence of an allergic pathogenesis (positive medical history in connection with evidence of a corresponding sensitization to typical aeroallergens). “So much evidence has accumulated on exhaled NO in particular in recent years that we have come to the conclusion that it is no longer possible to imagine asthma diagnostics without FeNO,” explained Prof. Dr. Marek Lommatzsch, senior physician in charge of the Department of Pneumology at the University Medical Center Rostock (D), at this year’s DGP congress in Düsseldorf [1].
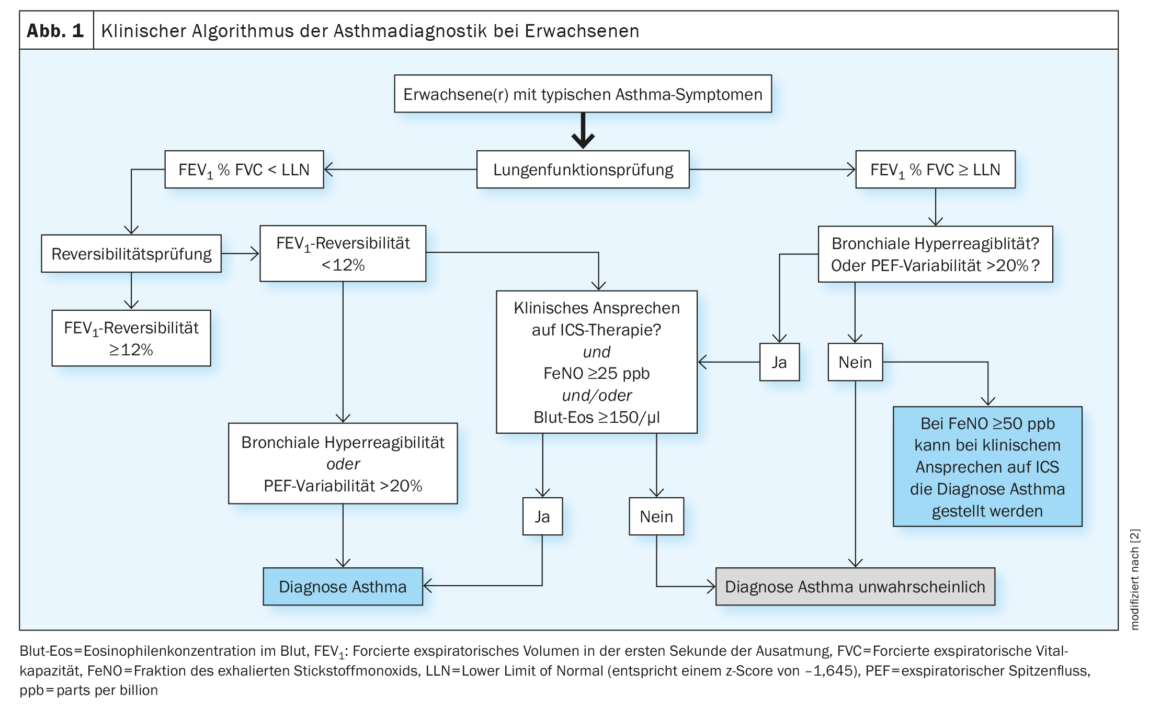
Prof. Lommatzsch is first author of the S2k guideline on specialist diagnosis and treatment of asthma [2]. With regard to the diagnostic procedure, the new guideline establishes an algorithm in which patients are first divided into obstructive and non-obstructive after a pulmonary function test as usual. If an obstructive patient has a reversibility of ≥12%, a diagnosis of asthma can be made with a typical history. However, there are also affected individuals who are not reversible (to salbutamol, for example) with a typical history. For these, an alternative pathway has been established, either demonstrating that patients have hyperresponsiveness or peak flow variability >20%. Or you can go by the type 2 markers: if they are elevated and there is a clinical response to ICS, you can also be said to have asthma (Fig. 1). The “biggest revolution” in this algorithm, according to Prof. Lommatzsch, concerns patients with normal lung function: in such cases, bronchial hyperresponsiveness testing with metacholine is typically performed first. Cases with a typical history, normal lung function, but no positive metacholine test are now being “bypassed” where a patient with an FeNO value >50 ppb and ICS response can also be considered an asthma case.
Remission formulated as a therapeutic goal
In the short term (i.e., within weeks), asthma control remains the first therapeutic goal. New in contrast to other guidelines, however, is the long-term (over years) formulated goal of clinical asthma remission, which has not been formulated so clearly in any previous guideline worldwide, as Prof. Lommatzsch emphasized. “Fifty years ago, we would never have been able to declare such ambitious goals. But thanks to modern drugs, we now have the opportunity to formulate them.” The expert referred to the different types of remission, first and foremost spontaneous remission, which can occur especially in children and adolescents, and “off treatment” remission, which can develop after allergen immunotherapy, for example. In addition, there are also patients who are in remission “on treatment”, i.e. under treatment.
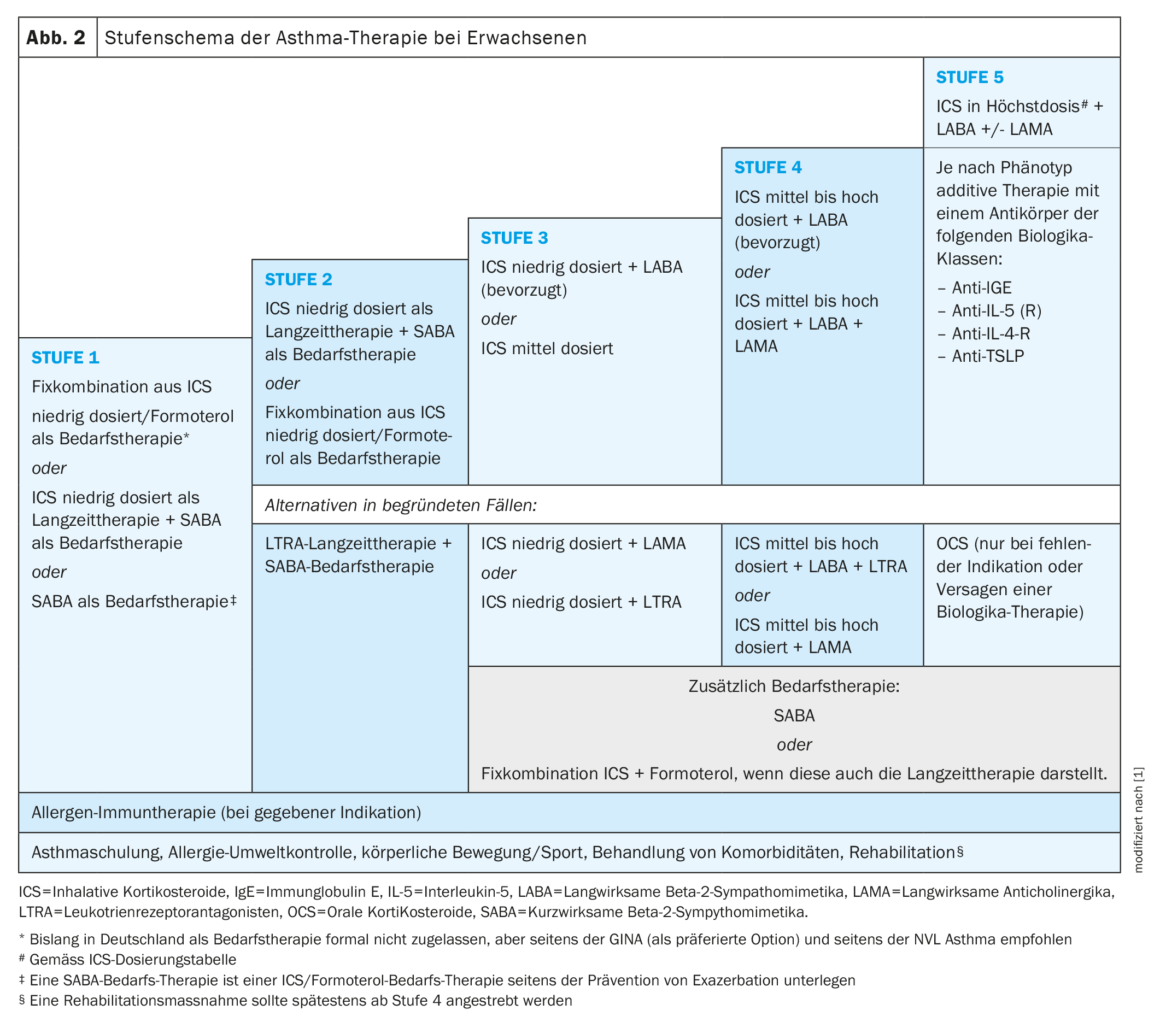
The grading scheme of the new guideline is largely similar to that of the NVL, but with minor nuances and accentuations. Again, the general recommendation for allergic asthma at all stages is to consider allergen immunotherapy. This includes patients who are already receiving a biologic. Contraindications, on the other hand, are uncontrolled asthma and/or an FEV1 <70% of the target value.
In mild asthma, the anti-inflammatory strategy is underscored that ICS should be used at low doses as early as possible in therapy. “Because inhaled steroids are the main driver of decreasing mortality.” The innovation from the NVL states that even for the mildest forms of asthma, one can think of ICS at low doses as long-term therapy as an alternative to ICS/formoterol if needed (Fig. 2). SABA on demand was also included, “even though we know it will probably be banned in ten years.”
ICS/LABA as long-term therapy
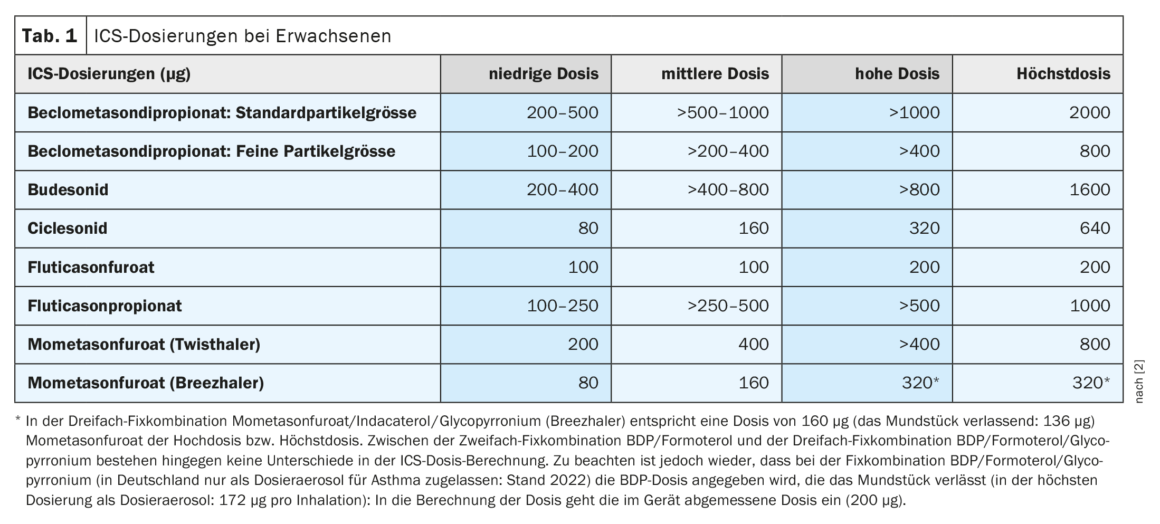
If this early use of ICS is not sufficient, the clear recommendation is to use an ICS/LABA fixed combination as long-term therapy. Prof. Lommatzsch sees the clear formulation of ICS doses with definition of a low, medium and high dose as well as the maximum dose for each inhaled steroid as a major advance of the new guideline (Tab. 1).
When diagnosing severe asthma, it should first be clarified whether the patient has asthma at all or is not suffering from a completely different disease (pulmonary embolism, tumor, etc.). “Once the asthma is established, we first call it ‘difficult-to-treat asthma’ and clarify various aspects,” the pulmonologist enumerated:
- Does the patient have the optimal inhaler and can he use it correctly?
- Are avoidable triggers eliminated?
- Were co-morbidities identified and treated?
- Has training been provided or is an asthma action plan in place?
- Have rehabilitation measures been examined?
Nowadays, only when all these basic measures have been queried and answered with yes, one speaks of severe asthma and can consider phenotype-specific additional therapy options.
At level 5, anticholinergics are available as adjunctive therapy. However, unlike in the NVL, a +/- recommendation is now made for ICS in maximum dose + LABA. So LAMA can be used and should be tried in most cases, but it is not a mandatory requirement as some patients do not respond to LAMA. In addition, the announcement “biologics before prednisolone” is emphasized even more than in the NVL: “We have to choose the biologic well, but we have to justify the prednisolone!”
| ABCD rule Medical history(e.g. age at onset, clinically relevant allergies) Biomarker expression(e.g., blood eosinophil count, FeNO, IgE levels). Co-morbidities(e.g. urticaria, CRSwNP, allergic rhinitis). Dosing interval/otherspecifics of biologics (e.g., route of administration). |
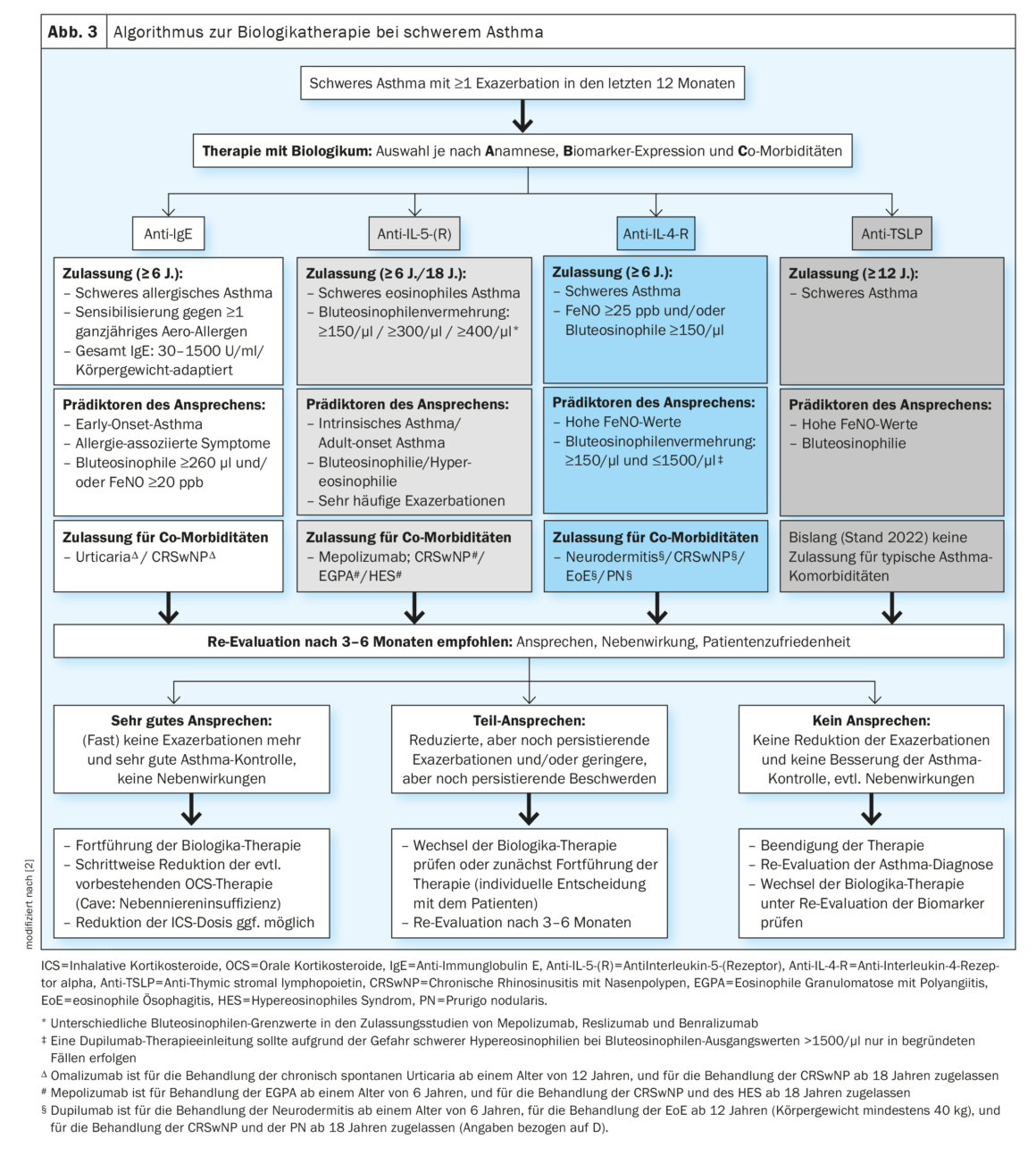
Currently, six biologics from four different classes are available for the treatment of severe asthma. The authors of the guideline have developed the so-called “ABCD rule” to support physicians in the initial selection of biologics (box). The selection should be made at the moment when a patient with severe asthma has exacerbated at least once. It is based on the criteria of approval, predictors of response and approval for co-morbidities (Fig. 3). In this way, typical patients can be “singled out” and directed to the best possible biologic, Prof. Lommatzsch concluded.
Congress: DGP 2023
Sources:
- Lommatzsch M: Vortrag «Die neue fachärztliche Asthma-Leitlinie (inkl. Differentialtherapie mit Biologika)» im Rahmen des Symposiums «State of the Art Asthma». 63. Kongress der Deutschen Gesellschaft für Pneumologie und Beatmungsmedizin e.V. in Düsseldorf, 31.03.2023.
- Lommatzsch M, Criee CP, De Jong C, et al.: S2k-Leitlinie zur fachärztlichen Diagnostik und Therapie von Asthma 2023, herausgegeben von der Deutschen Gesellschaft für Pneumologie und Beatmungsmedizin e.V.; März 2023; AWMF-Registernr.: 020-009.
InFo PNEUMOLOGIE & ALLERGOLOGIE 2023; 5(2): 22–26