Numerous procedures are available for the treatment of pathological scars. There is still no patent remedy to get rid of these skin changes. Individual and interdisciplinary approaches are most promising. This is also a core message of the new guideline issued this year.
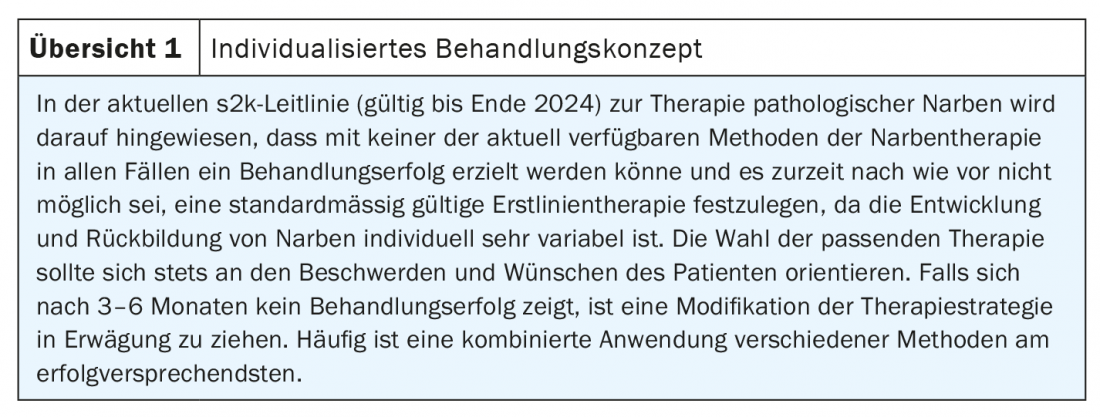
An indication for treatment is given when patients suffer from itching or pain, as well as functional limitations and impairment of quality of life related to potentially stigmatizing aesthetic aspects. Multiple sessions and a combination of procedures are often necessary to effectively treat scars. The new version of the s2k guideline on the therapy of pathological scars published this year was created under the aegis of Prof. Alexander Nast, MD, Clinic for Dermatology, Venereology and Allergology at Charité Universitätsmedizin Berlin. As a general treatment principle, it is recommended to adapt the therapy to the individual requirements of the respective patient (overview 1). There is also a high degree of consensus for the recommendation to modify the therapy strategy if no satisfactory therapy result is seen after three to six treatments or three to six months.
Treatment algorithms for hypertrophic scars vs. keloids
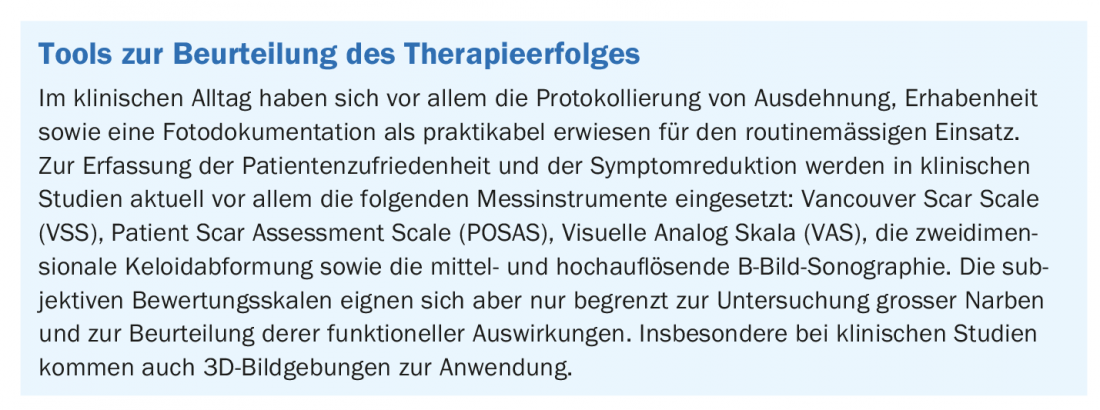
In the updated guideline, an algorithm is formulated for keloids and hypertrophic scars, and the individual measures are evaluated. Various measurement tools exist for assessing treatment success, which are also used in clinical trials (box).
In hypertrophic scars , which are associated with tension, surgical tension relief by local flap plasty or graft is advised. If the aesthetic component is the primary concern, excision and, depending on the risk-benefit ratio, subsequent conservative topical therapy are suggested. For large-area or disseminated scars, compression, laser or microneedling can be used, as well as additional conservative topical treatment if necessary. If the scars are smaller, there is a diverse selection of possible methods, which can also be used in combination: Triamcinolone acetonide (TAC) injection, cryotherapy, compression, ablative or non-ablative laser treatment, and possibly additional conservative topical therapy. If these treatment methods fail, the use of multimodal conservative measures and/or a repeat surgical procedure may be considered as alternatives.
For the treatment of small keloids, the use of TAC or cryotherapy is recommended initially, or combined if necessary. If inactive, flat keloids are involved, therapy using ablative laser in combination with TAC injection or “laser assisted drug delivery” (LADD) should be considered. If treatment goals are not achieved by these methods, the guideline recommends a combination of TAC and cryosurgery plus 5-fluorouracil (5-FU) intralesionally. Alternatively, surgical intervention with subsequent follow-up treatment may be considered. If erythematous changes occur, laser treatment using dye lasers or IPL can be effective. In the case of larger keloids, the guideline advises excision, emphasizing the need for follow-up with compression, TAC, cryosurgery, or radiotherapy, if necessary in combination with conservative topical therapy or intralesional cryotherapy. If the keloids are disseminated over a large area, they can be treated like individual small keloids. The same applies to large-area confluent keloids, for which, analogous to smaller variants thereof, partial treatment of particularly growth-active portions is recommended.
Evaluation of individual therapy options
Glucocorticosteroids: The guideline recommends intralesional injection of glucocorticosteroids in isolation or in combination with cryotherapy for the treatment of hypertrophic scars and keloids. Triamcinolone acetonide (TAC) injection is also advised after surgical therapy for keloids. Here, TAC is most commonly injected at a concentration of 10-40 mg, maximum 5 mg/cm2) pure, diluted with NaCl 0.9% or lidocaine 1:2 to 1:4. The chances of therapeutic success are highest for bright red, possibly itchy or painful active scars. If necessary, further injections are possible at intervals of three to four weeks. By slowly increasing the concentration from an initial 10 mg/ml to 20 mg/ml and 40 mg/ml, respectively, over time, the risk of undesirable side effects and recurrences can be reduced. For pain reduction, superficial icing in an open spray procedure immediately before treatment can be helpful. If there is no improvement after three treatments, it is suggested to adjust the therapy concept, for example by combining it with 5-FU. As a prophylactic application, good efficacy was obtained by direct intraoperative injection into the wound margins (dosage of 1 mg TAC/cm2).
Cryotherapy: Cryotherapeutic treatment is recommended for both hyertrophic scars and keloids, especially combined with TAC injections, with brief cryotherapy facilitating the injection. Intensive cryotherapy results in complete freezing of the tissue. The recommended treatment interval is four to six weeks. In intralesional cryotherapy, the entire keloid is frozen by introducing nitrogen through a double hollow needle. With this rarely used form of treatment, the keloid regresses within four to six months.
Pressure treatment: Large-area hypertrophic scars, such as those that occur after burns or scalds, are particularly suitable for pressure treatment. This treatment method is also recommended after surgical interventions. The 24-hour treatment with 20-30 mmHg pressure, which is usually carried out by means of compression suits or bandages, should be started as early as possible or, in the case of a known tendency to pathological scarring, also as a preventive measure. Over the course of the six- to twelve-month treatment period, the pressure can be slowly reduced. As part of postoperative prophylaxis, pressure treatment should be continued for at least six to 24 months.
Surgical therapy: S urgical intervention is not recommended for hypertrophic scars that have existed for less than a year and are not associated with tension or aesthetic disfigurement. However, if scar contractures at joints or in mobile regions with functional limitations are involved, or if cosmetic disfigurement is present, prompt surgical therapy using stress-relieving plastics is recommended. Alternatively, grafts can also be used. In the case of keloids, the guideline experts urge caution with regard to the indication of surgical therapy in connection with the high risk of recurrence. It is important to pay attention to detailed preoperative patient education and postoperative long-term multimodality follow-up. If this is considered, surgical intervention is a possible option for keloids that have not been satisfactorily treated by conservative procedures, with extramarginal excision advised in conjunction with adjuvant therapies. With exclusive surgical treatment, the risk of recurrence in keloids is high (recurrence rates 45-100%). Because of this, special emphasis should be placed on undisturbed wound healing and reduction of tensile forces during surgical intervention, and all plastic procedures from primary closure to flap plasty can be used.
Laser treatment: Fractional ablative lasers (CO2, Er:YAG, Er:YSGG, thulium) or non-ablative lasers (dye, Nd:YAG, IPL) can be used to treat hypertrophic scars, especially after burns or scalds. The dye laser is particularly suitable for erythema reduction such as in fresh, vascularized, reddened hypertrophic scars and keloids. Ablative fractional laser can be used promptly after sutures are removed. At least six therapy series at intervals of four weeks are recommended, whereby the ablation channels introduced into the scar tissue can also be used for the application of active substances such as TAC or 5-FU (“laser assisted drug delivery”, LADD). Treatment with the non-ablative dye laser is usually performed with 5.5-7.5 J/cm2 for spot diameters of 5-7 mm or with 4.5-5.5 J/cm2 for spot sizes of 10 mm. At least two therapy sessions should be given at intervals of six to eight weeks. Especially for Nd:YAG lasers and IPL, the treatment protocols are not very standardized and the parameter settings also depend on the respective device-specific factors.
Microneedling: This technique is suitable for the therapy of hypertrophic scars. The treatment principle consists in creating microtrauma of the skin via a roller or stamp with a needle in the length of 1.5-3 mm, followed by a wound healing cascade. In this process, active substances can be introduced into the skin through the puncture channels (LADD). Microneedling treatment for keloids is not recommended.
Radiotherapy: A possible indication is the treatment after excision of recurrent, difficult to treat or large keloids. Radiotherapy should preferably be given in the form of HDR (“high-dose rate”) brachytherapy as an adjuvant measure, since the lowest recurrence rates have been achieved with this method (on average about 10%). The chances of success with postoperative radiation are best when started within seven hours of excision. Adjuvant radiotherapy should be started within 24 hours at the latest.
Silicone: The use of silicone-containing gels, creams, pads and films is usually done for 12-24 hours a day for a period of 12-24 weeks. If this technique is used for postoperative treatment, it is recommended to start the therapy shortly after the removal of the stitches or, in case of open wounds, after the complete epithelialization. Evidence for benefit in the treatment of hypertrophic scars and keloids exists with regard to the thickness and color of scars, he said. According to the guideline, there is little evidence regarding the benefit of silicone preparations for the prevention of hypertrophic scars and keloids.
Onion extract: The conclusion of the guideline experts is that, due to a lack of evidence of benefit, this treatment method should only be considered as an add-on therapy. Treatment of active hypertrophic scars or keloids or postoperative prophylaxis with onion extract is critically evaluated. In the case of repeated daily external application, contact allergic reactions are also feared.
5-Fluorouracil and bleomycin: There is also only a weak recommendation regarding 5-fluorouracil (5-FU) for the treatment of therapy-resistant hypertrophic scars and for prophylaxis, respectively. A ‘may’ recommendation for 5-FU is given for the treatment of refractory keloids. 5-FU is administered off-label at a concentration of 50 mg/ml and a maximum total dose of 50-150 mg per treatment each four weeks apart (intralesional injection into scar tissue). There is evidence that combined use of 5-FU plus TAC in a 9:1 or 3:1 ratio is superior to respective monotherapy. This combination reduces the risk of side effects from TAC. As an alternative to 5-FU, bleomycin is rarely used off-label, especially in dark-skinned patients, at a concentration of 1.5 IU/ml.
Other therapeutic approaches: With regard to calcium channel blockers, neither a recommendation for nor against their use for prophylaxis or therapy of hypertrophic scars or keloids can be given due to the limited and inconsistent data available. The same applies to hyaluronidase and also to plasma. The use of imiquimod for prophylaxis or therapy of hypertrophic scars or keloids is not recommended.
Source: Nast A, et al: S2k-Leitlinie Therapie pathologischer Narben (hypertrophic scars and keloids) – Update 2020. J Dtsch Dermatol Ges 2020, https://doi.org/10.1111/ddg.14279
DERMATOLOGY PRACTICE 2020; 30(6): 46-47











