In newly diagnosed type 2 diabetes, the risk of diabetic complications and death can be delayed by many years with the best possible glycemic control. That blood glucose levels early in the course of the disease have a much greater impact on future prognosis than previously thought is clear from a recently published secondary analysis. In addition, current treatment guidelines indicate that patients may benefit from early use of SGLT-2 inhibitors and GLP-1 receptor agonists in many cases.
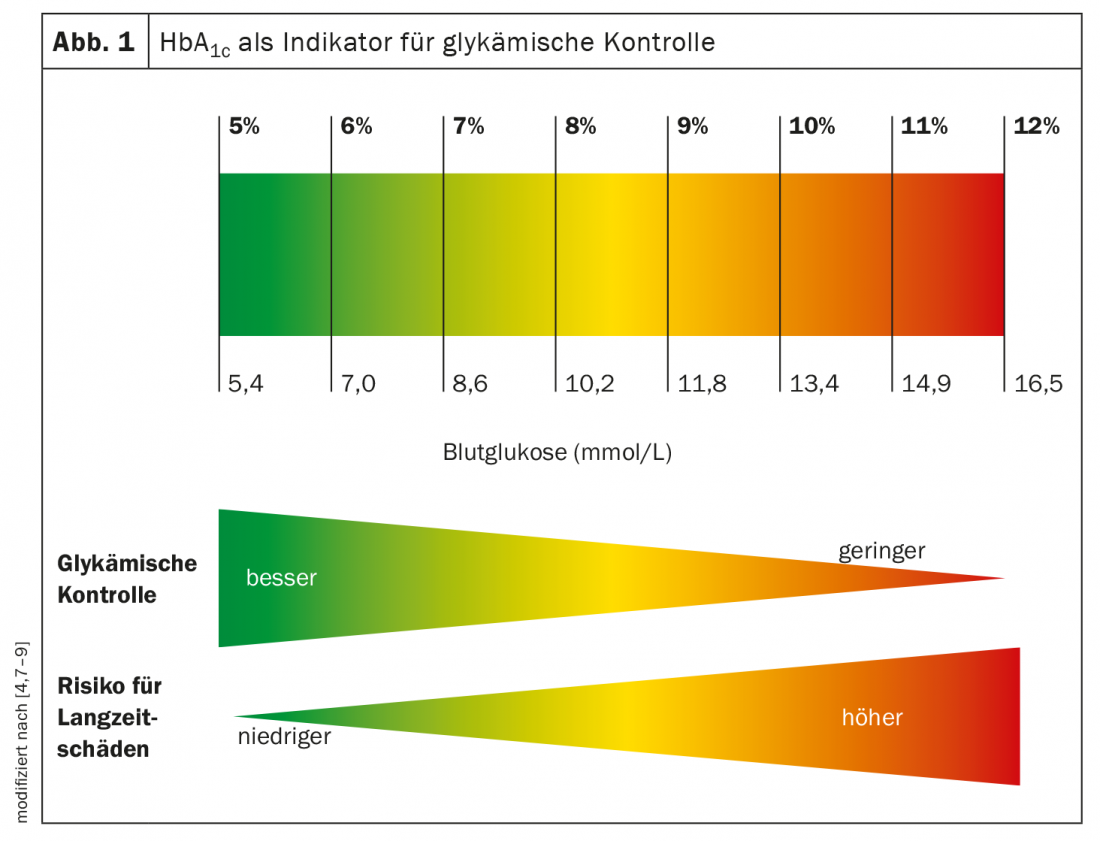
A good HbA1c is important to avoid microvascular and macrovascular complications. In a study led by Prof. Dr. Marcus Lind, Gothenburg, and Prof. Dr. Rury Holman, Oxford, based on data from the UK Prospective Diabetes Study (UKPDS), the importance of blood glucose levels from the time of diagnosis of type 2 diabetes on the risk of myocardial infarction and death 10-20 years later was investigated [1–3].
Early glycemic control is relevant for longer-term prognosis
From the results of the data analyses, glycemic control early in the course of the disease has a significant impact on future prognosis. Thus, the researchers demonstrated that targeting according to treatment guidelines (HbA1c ≤6.9% and ≤52 mmol/mol, respectively) from the time of diagnosis was associated with an approximately 20% lower risk of death 10-15 years later, compared with higher blood glucose levels (HbA1c ≤7.9% and ≤63 mmol/mol, respectively) [1–2]. “These latest results are evidence that appropriate early glycemic control in type 2 diabetes is critical for optimizing diabetes care. Previously, we have not done this type of analysis or understood how important early glycemic control is to prognosis. They also mean that there needs to be a greater focus on detecting type 2 diabetes as early as possible to prevent people from living with undetected high blood glucose levels for several years,” said Prof. Lind [1]. And Prof. Holman of Oxford University said, “These new results provide a mechanistic explanation for the glycemic ‘legacy effect’ first identified in the UKPDS, whereby the establishment of good glycemic control in newly diagnosed type 2 diabetes was shown to reduce the risk of diabetic complications and death for up to 30 years. The discovery of the ‘legacy effect’ has led to treatment guidelines worldwide that recommend achieving good glycemic control as soon as possible” [1].
Taking advantage of SGLT-2 inhibitors and GLP-1 agonists.
The Swiss Society of Endocrinology and Diabetology (SGED) currently recommends the following substances for drug treatment [5]: Metformin, DPP-4 inhibitors, SGLT-2 inhibitors, and GLP-1 receptor agonists (RA). Sulfonylureas are now only rarely used. Currently, DPP-4 inhibitors are still the most commonly used in Switzerland after metformin. Although HbA1c reduction can be achieved, no effect in terms of reduction of major adverse cardiac events (MACE) has been demonstrated in the large endpoint studies (CVOTs). In contrast, both GLP-1-RA and SGLT-2 inhibitors have shown additional benefit in this regard. This is highly relevant because about 25% of all type 2 diabetes patients have cardiovascular disease or impaired renal function (eGFR <60 ml/min) each. In the large cardiovascular endpoint studies on both groups of compounds (SGLT-2 inhibitors: EMPA-REG-Outcome, CANVAS, DECLARE; GLP-1 receptor agonists: LEADER, EXSCEL, HARMONY, REWIND, SUSTAIN-6, PIONEER), the 3-point MACE was highly significantly reduced between 10-26% [6]. In addition, the CREDENCE and DAPA-CKD studies demonstrated improvement in renal endpoints for canagliflozin and dapagliflozin, and the DAPA-HF study prospectively demonstrated that SGLT-2 inhibitors have the potential to reduce hospitalization rates in heart failure patients. For the subpopulation of older type 2 diabetics with obesity and insulin resistance, GLP-1 analogues, which need to be given only once a week, are often very effective and without risk of hypoglycemia, but should be discontinued if weight loss is unintentional [6]. The lack of hypoglycemia risk of SGLT-2 inhibitors and GLP-1-RA is also favorable in terms of combinability with insulin. It should not be forgotten that around a quarter of all type 2 diabetics have an insulin deficiency. And with regard to lifestyle factors, in the spirit of multimodal diabetes management, all type 2 diabetics should be made aware of the health benefits of a balanced diet and regular exercise (at least 150 minutes weekly).
Literature:
- “Early blood-sugar levels in type 2 diabetes crucial for future prognosis”, University of Gothenburg, Faculty of Medicine, Sahlgrenska Academy, 8.7.2021.
- Lind M, et al: Long-term Effects of Earlier Glycemic Control. Historical HbA1c Values May Explain the Type 2 Diabetes Legacy Effect: UKPDS 88. Diabetes Care 2021; 44(10): 2231-2237.
- UK Prospective Diabetes Study (UKPDS) Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837-853.
- Lehmann R: The treatment of type 2 diabetes – advances, challenges and opportunities. Prof. Dr. med. Roger Lehmann, FomF Update Refresher, 18.11.2021
- SGED Recommendations Diabetology, www.sgedssed.ch/diabetologie/sged-empfehlungen-diabetologie (last accessed Dec. 15, 2021).
- German Health Report: Diabetes 2021: Taking Stock, German Diabetes Society (DDG) and diabetesDE (eds.), www.deutsche-diabetes-gesellschaft.de (last accessed Dec. 15, 2021).
- Nathan DM, et al: Translating the A1c assay into estimated average glucose values. Diabetes Care 2008; 31: 1473-1478.
- Starship NZ, https://starship.org.nz/long-term-goals-for-diabetes-management (last accessed Dec. 15, 2021).
- Kim KJ, et al: Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study. Diabetes Metab J 2021; 45(3): 368-378.
HAUSARZT PRAXIS 2022; 17(1): 20-22