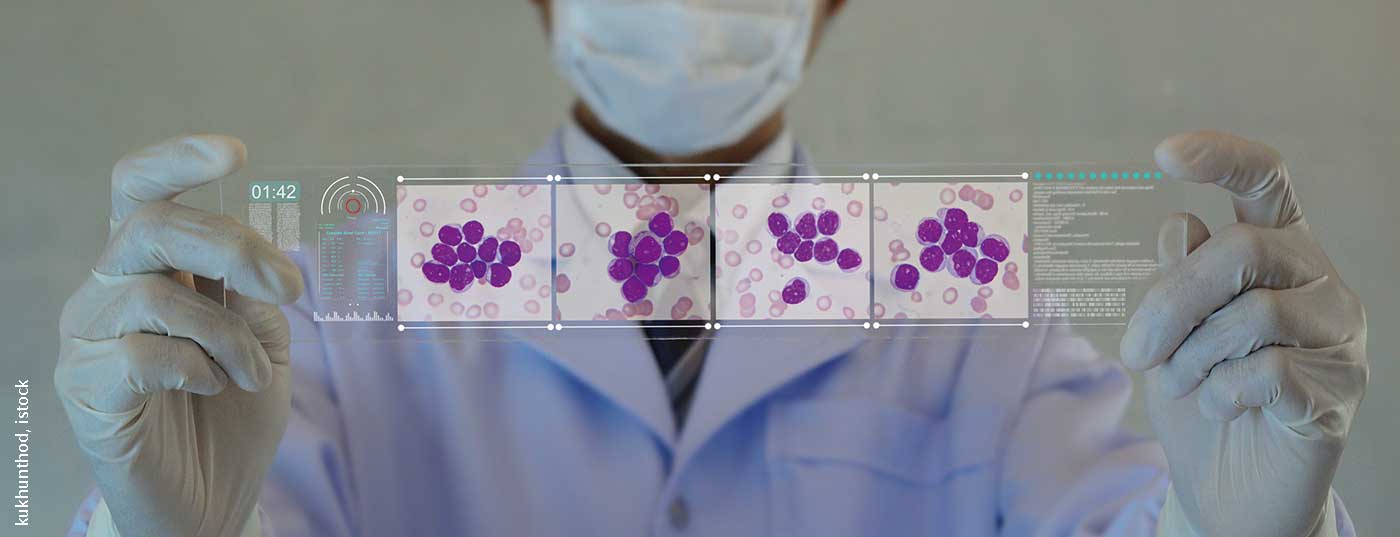
Understanding about myeloid diseases, such as acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), is becoming more concrete thanks to intensive research. Recent study results have shown that there is much movement in the field of myeloid diseases. Now immunological therapies are also entering the armamentarium of treatment options.
Immunotherapeutic approaches such as CAR-T cell therapy, checkpoint inhibitors and antibodies are opening a new chapter in the therapy of myeloid diseases. AML is primarily a disease of older adults. However, previously commonly used standard low-intensity therapies, such as azacitidine (AZA) or decitabine, have had limited efficacy. However, AML patients who cannot receive intensive treatment have an unfavorable prognosis. Therefore, in a phase III study, the combination of AZA with the BCL-2 inhibitor venetoclax (VEN) was investigated in more detail. Included were 431 patients with initial diagnosis of AML who were unable to receive intensive therapy due to age ≥75 years or comorbidities. Randomized in a 2:1 ratio, patients received either AZA+VEN or AZA+placebo (PBO). With a median follow-up of 20.5 months, the AZA+VEN arm showed a median overall survival (mOS) of 14.7 months versus 9.6 months with AZA+PBO. Complete remissions, or complete remissions with incomplete hematologic recovery (CRi) were achieved in 66% versus 28% at 1.3/2.8 months.
Targeting AML
Another advance was highlighted in more detail with the combination of AZA with the IDH2(isocitrate dehydrogenase 2) inhibitor enasidenib (ENA) in a phase II study. ENA is already approved in the U.S. for the treatment of AML patients with relapsed or refractory disease when the driver mutation in the IDH2 gene is detected, and has also effectively demonstrated efficacy in monotherapy in older patients with an initial diagnosis of IDH2-mutated AML. In the present study of 101 patients, the combination of ENA+AZA now scored significantly over AZA monotherapy in terms of response and CR rate (53% vs. 12%). Duration of response increased to 24.1 months with combination treatment versus 12.1 months with monotherapy. Median event-free survival (mEFS) was also higher with ENA+AZA at 17.2 months compared with AZA monotherapy at 10.8 months. However, no improvement in overall survival (OS) was shown. The experts speculated that the encouraging results could lead to consideration of the use of targeted combination therapies for fit AML patients, but also as part of triple combination approaches such as ENA+VEN+AZA for elderly patients.
Curative AML treatment
However, despite all developments, immunologic therapy by allogeneic stem cell transplantation (SCT) remains the only option for curative therapy in AML patients with intermediate- or high-risk profiles or relapses. However, to date, the lack of suitable target antigens has prevented the establishment of CAR-T cell therapy in AML. Therefore, in a phase I study, CLL1(human C-type lectin-like molecule-1) antigen expressed in leukemic stem cells (LSC) and CD33 (Siglec-3; sialic acid-binding Ig-like lectin 3) broadly myeloid expressed antigen were used to generate bispecific CAR-T cells. When used in relapsed and refractory AML patients, minimal residual disease (MRD) negativity was achieved in 7 of 9 patients at 4 weeks. 6 patients underwent allogeneic SCT during the course. An encouraging sign that CAR-T cell therapies may also find their place in myeloid diseases.
Source: EHA 2020
Further reading:
- https://library.ehaweb.org/eha/2020/eha25th/303390 (last accessed 9/11/2020)
- https://library.ehaweb.org/eha/2020/eha25th/294959 (last accessed 9/11/2020)
- https://library.ehaweb.org/eha/2020/eha25th/294969 (last accessed 9/11/2020)
InFo ONCOLOGY & HEMATOLOGY 2020; 8(4): 29 (published 9/22/20, ahead of print).