Many cancer patients are interested in complementary medicine measures. There is now evidence of efficacy for some of the supportive treatments. Good interdisciplinary cooperation is central to this.
Evidence-based medicine [1], i.e., orientation towards empirical evidence and clinical expertise while incorporating patients’ values and wishes, is also a very important paradigm for complementary medicine interventions. As early as 2000, 49% of patients were using complementary medicine treatments [2], and a significant increase in interest has been observed for several years. Since 2009, complementary medicine has been anchored in the Swiss constitution [3] and many treatments by qualified therapists can be covered by basic or supplementary insurance. Prof. Dr. med. Claudia Witt, Director and Professor at the Institute for Complementary and Integrative Medicine at the University Hospital Zurich and Professor at the University of Maryland and at the Charité Berlin, presented current findings from research and practice.
Evidence-based integrative oncology
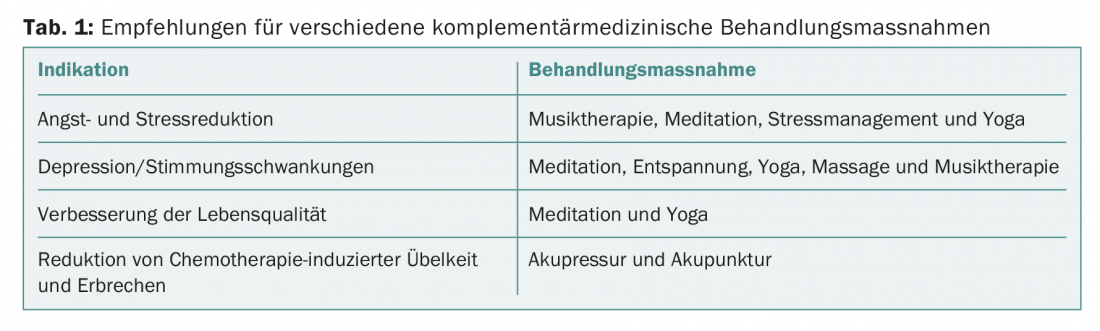
Integrative oncology is a patient-centered, evidence-informed field of cancer treatment that uses mind-body practices, natural products, and/or lifestyle changes from a variety of traditions to accompany conventional cancer therapies. Integrative oncology seeks to optimize health, quality of life, and clinical outcomes across the treatment continuum, empowering people to prevent cancer and become active participants before, during, and beyond cancer treatment [4,5]. There is now an interesting evidence base for many complementary medicine interventions. Some of these were presented in the lecture and others were found in the literature, which are also mentioned here. For example, the American Society for Integrative Oncology has published evidence-based recommendations for indications of various treatment interventions of complementary and integrative medicine based on empirical meta-data [6] (Table 1).
Diet and exercise: Regarding the lifestyle factors diet and exercise as a supportive intervention in breast cancer, a longitudinal study (n=1490, observation period eight years) showed that just the combination of a diet with five servings of vegetables/fruit per day with higher physical activity tended to have a more positive effect on life expectancy in breast cancer [7]. Empirical evidence of efficacy for exercise interventions also exists with respect to fatigue and breast cancer-specific apprehension (weighted mean effect sizes = -0.54 and 0.62; p=0.003, respectively) [8]. Walking, Nordic walking, yoga, and qigong at moderate intensity and frequency (e.g., five times per week for a period of 30 minutes) are particularly well suited [8]. Yoga has been shown to be effective in reducing anxiety and depression and improving quality of life [9].
Mindfulness-based therapies: Concerning mindfulness-based therapies as complementary treatment interventions for various diseases, study results are summarized in a review article [10] and a meta-analysis [11] and there are further studies on this [9,12]. The results of Gotink et al. [10] Are based on 23 reviews with data from 115 RCTs (n=8683). Using MBSR (“Mindfulness-Based Stress Reduction”) and MBCT (“Mindfulness-Based Cognitive Therapy”) showed significant improvement in stress (d=0.51, 95% CI 0.36-0.67), anxiety (d=0.49, 95% CI 0.37-0.61), depression (d=0.37, 95% CI 0.28-0.45), and quality of life (d=0.39, 95% CI 0.08-0.70) compared with the control group and standard treatment. The changes brought about by mindfulness-based therapies are described as follows: Attention regulation, body awareness, emotion regulation, altered self-awareness [13]. Imaging studies have shown effects in corresponding brain areas (anterior cingulate cortex: self-regulation and attention; prefrontal cortex: attention and emotions; insula: awareness, emotional processing; striatum: regulation of attention and emotions; amygdala: emotional processing) [14]. That mindfulness-based therapies may also have positive effects on cellular aging (d=0.46, n=190) was demonstrated in a meta-analysis by Schutte and Malouff [11], with this explained by an increase in telomerase activity.
Acupuncture and acupressure: Other complementary medicine treatments that have better empirical support include acupuncture and acupressure. Acupuncture and acupressure are considered safe treatment options [15], which were recommended by over 60% of Comprehensive Cancer Centers in the United States prior to 2010 [16]. There is empirical evidence of efficacy for concomitant use with analgesics to reduce pain [17] and to reduce chemotherapy-induced postoperative nausea and vomiting [18,19]. In a meta-analysis by Cheong et al. [18] (30 RCTs, n=2534) showed that pericardial PC6 acupuncture significantly reduced (RR 0.36, 95% CI 0.19-0.71, p=0.003) the number of cases of early vomiting (postoperative 0-6 h) as well as contributed to a significant reduction (RR 0.25, 95% CI 0.10-0.61, p=0.002) of nausea (postoperative 0-24 h). Also in the study by Dibble et al. [19] showed a significant reduction in chemotherapy-induced nausea and vomiting in the acupressure condition (“wrist device”) compared with placebo and standard treatment.
“Mind Body Medicine” as a supportive treatment measure
In summary, there is a growing body of evidence supporting the use of integrative therapies. “Mind Body Medicine” is an approach originally developed for the treatment of pain disorders and later adapted for use with cancer, incorporating elements of mindfulness-based therapy [20]. It is a multimodal and integrative treatment concept that has been further developed at the Institute for Complementary and Integrative Medicine of the University Hospital Zurich, among others, and is offered for various diseases. A main goal of this treatment concept is to positively influence the balance of body and psyche during or after a conventional cancer therapy and to contribute to a reduction of symptoms and a strengthening of self-efficacy. The exercise sessions are conducted in a group setting and include the following components: Lifestyle modification (e.g., diet and exercise), stress management, and complementary self-help measures. In addition, there are medical rounds with the opportunity to clarify questions, and psychological topics such as illness perception and illness processing are discussed. The interdisciplinary collaboration of complementary physicians with oncologists and psychologists is something very important, Prof. Witt said.
Practical recommendations for everyday clinical practice
One problem with the feasibility of implementing complementary therapy measures in everyday clinical practice is that there is often insufficient space for the discussion of corresponding treatment options [9]. Reasons include time pressure, patient role, and insufficient access to relevant expertise [21–23]. To change this in the future, recommendations and training programs for physicians have been developed [5,9]. To clarify patient requests and questions about specific complementary medicine treatments, Prof. Witt recommends the following databases that provide information based on peer-reviewed summaries: Onkopedia and CAM Cancer (Complementary and Alternative Medicine for Cancer). The About Herbs MSKCC (Memorial Sloan Kettering Cancer Center) website and app is also recommended. One advantage of non-drug supportive therapies (diet, exercise, acupuncture/acupressure, etc.) is that the risk of interactions with orthodox cancer medications is avoided.
Source: Swiss Symposium on Psychooncology, May 31, 2018, Bern.
Literature:
- Sackett DL, et al: Evidence based Medicine: what it is and what it isn’t. It’s about integrating individual clinical expertise and the best external evidence. BMJ 1996; 312: 71-72.
- Horneber M, et al: How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther 2012; 11(3): 187-203.
- Federal Constitution of the Swiss Confederation : constitutional article 118a.
- Witt CM, et al: A Comprehensive Definition for Integrative Oncology. J Natl Cancer Inst Monogr 2017; 2017(52).
- Witt CM, et al: Competence Network Complementary Medicine in Oncology (KOKON) – A scientific contribution to improving care. Forum 2017; 32: 416-432.
- Greenlee H, et al: Clinical Practice Guidelines on the Evidence-Based Use of Integrative Therapies During and After Breast Cancer. CA Cancer J Clin 2017; 67(3): 194-232.
- Pierce JP, et al: Greater survival after breast cancer in physically active women with high vegetable-fruit intake regardless of obesity. J Clin Oncol 2007; 25(17): 2345-2351.
- Speck RM, et al: An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv 2010; 4: 87-100.
- Witt CM, Cardoso MJ: Complementary and integrative medicine for breast cancer patients – evidence based practical recommendations. Breast 2016; 28: 37-44.
- Gotink RA, et al: Standardised mindfulness-based interventions in healthcare: an overview of systematic reviews and meta-analyses of RCTs. PLoS One 2015; 10(4): e0124344.
- Schutte NS, Malouff JM: A meta-analytic review of the effects of mindfulness meditation on telomerase activity. Psychoneuroendocrinology 2014; 42: 45-48.
- Lengacher CA, et al: Examination of Broad Symptom Improvement Resulting From Mindfulness-Based Stress Reduction in Breast Cancer Survivors: A Randomized Controlled Trial. Journal of Clinical Oncology 2016; 34(24): 2827-2834.
- Hölzel B, et al: Perspectives on Psychological Science 2011; 6(6): 537-559.
- Tang YY, Holzel BK, Posner MI: The neuroscience of mindfulness meditation. Nat Rev Neurosci 2015; 16: 213-225.
- Witt CM, et al: Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed 2009; 16(2): 91-97.
- Brauer JA, et al: Complementary and alternative medicine and supportive care at leading cancer centers: a systematic analysis of websites. J Altern Complement Med 2010; 16(2): 183-186.
- Hu C, et al: Acupuncture for Pain Management in Cancer: A Systematic Review and Meta-Analysis. Evidence-Based Complementary and Alternative Medicine 2016: 1-13.
- Cheong KB, et al: The Effectiveness of Acupuncture in Prevention and Treatment of Postoperative Nausea and Vomiting – A Systematic Review and Meta-Analysis. PLoS One. 2013 Dec 13; 8(12): e82474.
- Dibble SL, et al: Acupressure for chemotherapy-induced nausea and vomiting: a randomized clinical trial. Oncol Nurs Forum 2007; 34(4): 813-820.
- Kabat-Zinn J, et al: Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1992; 149(7): 936-943.
- Schofield PE, Juraskova I, Butow PN: How oncologists discuss complementary therapy use with their patients: an audio-tape audit. Support Care Cancer 2003; 11(6): 348-355.
- Corbin Winslow L, Shapiro H: Physicians want education about complementary and alternative medicine to enhance communication with their patients. Arch Intern Med 2002; 162(10): 1176-1181.
- Münstedt K, et al: Wishes and Beliefs of Cancer Patients Regarding Counseling on Integrative Medicine. Breast Care 2014; 9: 416-420.
InFo ONCOLOGY & HEMATOLOGY 2018; 6(3): published 6/13/18 (ahead of print).