If a malignant skin tumor is clinically and dermatoscopically suspected, it should be completely excised, if possible, and classified according to the TNM system (tumor, lymph nodes, metastases). Depending on histopathology, stage of the disease and detection of mutations, for example in malignant melanoma, the indication for one of the new system therapies may be given or irradiation may be given. Discussion takes place in the multidisciplinary tumor board and with the patient.
Prof. Ketty Peris, MD, from Rome, offered an overview of new findings on the genetic susceptibility to developing malignant melanoma at a continuing education event in Munich. Individuals with red or blond hair, fair skin and eye color, low tanning ability, and atypical, numerous nevi are phenotypically most at risk for malignant melanoma. Underlying rare high-penetrance genes such as CDKN2A and CDK4; they play the key role in familial melanomas, which account for about 5-12% of cases. Of low penetrance are numerous genes for pigmentation, nevib formation, DNA repair, and cell cycle control. They play the decisive role in the majority of sporadic melanoma cases.
Thanks to new technologies such as whole exome sequencing, next generation sequencing (NGS) and whole genome sequencing, new candidate genes have been discovered. MITF (“microphthalmia-associated transcription factor”), BAP1 (“BRCA1-associated protein-1”) and TERT (“telomerase reverse transcriptase”) are, for example, significantly involved in the control of differentiation, proliferation and survival of melanocytes.
Amplifications in only one base or mutations in the SOX10 regulator of MITF are found in familial and sporadic malignant melanomas and may be partly responsible for the metastatic tendency. Candidate gene studies have found associations between malignant melanoma, pancreatic cancer, and renal cell carcinoma. BAP1 mutations predispose to malignant melanoma of the skin and uvea, but they have also been found in numerous other tumor entities. The linkage of telomeres, nevi, and melanoma risk via TERT was demonstrated in familial and sporadic melanomas.
“Nested Melanoma of the elderly.”
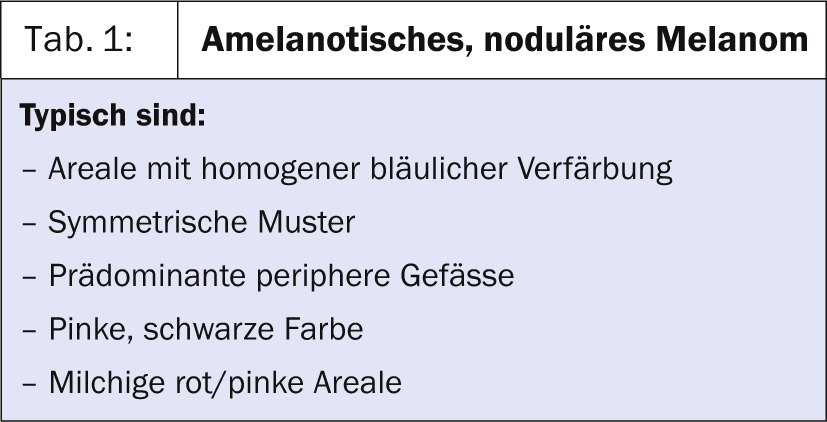
New fascinating insights into the world of dermoscopy of nodular and desmoplastic melanoma [1] were offered by Prof. Peris in the second part of her presentation. The differential diagnosis of amelanotic nodular melanoma (basal cell carcinoma, spinocellular carcinoma) is dermoscopically based on the
pigmentation degree, the vessel volumes and the special features in the coloration are often possible (Tab. 1).
Desmoplastic melanoma always shows at least one melanoma-specific feature: atypical vessels, atypical globules, crystalline structure, blue-white veil. Biopsy is still indicated in most cases, Prof. Peris concluded.
A new entity that has been described is “Nested Melanoma of the Elderly” (histopathologically: variant of “Superficial spriting Melanoma”) with large intraepidermal nests that appear like cannonballs. Dermoscopically, a reticular pattern and pigmented globules of irregular size, color, and distribution on a dark brown structureless background are noticeable [2].
“Non-Melanoma Skin Cancer.
Basal cell carcinoma and spinocellular carcinoma are the most common malignant tumors in humans, with up to 1.2 million new cases occurring each year in the United States. More than half of those affected develop other non-melanotic tumors of the skin (“non-melanoma skin cancer”) within five years. The importance of UV radiation can be seen in the lateralization: occupational
motorists have significantly more melanomas, Merkel cell tumors, non-melanotic tumors and actinic keratoses on the side of the vehicle window.
The most important new therapy option presented by Prof. Dr. med. Philipp Babilas from Regensburg was Ingenol mebutat (Picato®), which is suitable for the indication of non-hypertrophic and non-hyperkeratotic
actinic keratoses is approved. The treatment field is limited to 25 cm2, and the inflammatory response with neutrophil infiltration and necrosis due to cell membrane rupture is delayed after three to five days. Compliance is good. Complete clinical remission has been achieved in 42% of patients in Lebwohl’s study. Photodynamic therapy can further increase the remission rate.
In metastatic head and neck spinocellular carcinoma, the EGFR antibody cetuximab (Erbitux®) and the EGFR tyrosine kinase inhibitors erlotinib (Tarceva®) and gefitinib (Iressa®) are new therapeutic options with good response rates [3]. Acne-like rush occurred in 78% of patients. “However, polychemotherapy with cisplatin and 5-FU remains the standard therapy for metastatic spinocellular carcinoma,” Prof. Babilas concluded.
For unresectable and advanced metastatic basal cell carcinoma and Gorlin-Goltz syndrome, a highly potent selective inhibitor of the Hedgehog pathway, vismodegib (Erivedge®), has been introduced. Taken orally once daily, amazing results can be achieved, but only 20% of patients tolerated it for longer than 18 months [4, 5]. Imiquimod (Aldara®), photodynamic therapy, and 5-FU continue to be excellent treatment options for this group of patients, he said.
The BRAF inhibitor vemurafenib (Zelboraf®) induces the appearance of kerathoacanthomas or spinocellular carcinomas in 25% of patients. This is caused by activation of the RAS signal transduction pathway in cells with mutations in RAS. Vemurafenib increases the growth of existing lesions. Viros et al. investigated whether 5% 5-flourouracil topical could be an option in these cases. Fresh lesions responded well, older hyperkeratotic ones less well.
Source: 3rd Munich International Summer Academy of Practical Dermatology (ISA), July 21-26, 2013, Munich.
Literature:
- Menzies SW, et al: Dermoscopic evaluation of nodular melanoma. JAMA Dermatol 2013; 149(6): 699-709.
- Longo C, et al: Dermoscopy and confocal microscopy of nested melanoma of the elderly: recognizing a newly defined entity. JAMA Dermatol 2013; 149(8): 941-945.
- de Andrade DA, Machiels JP: Treatment options for patients with recurrent or metastatic squamous cell carcinoma of the head and neck, who progress after platinum-based chemotherapy. Curr Opin Oncol 2012; 24(3): 211-217.
- Viros A, et al: Topical 5-fluorouracil elicits regressions of BRAF inhibitor-induced cutaneous squamous cell carcinoma. J Invest Dermatol 2013; 133(1): 274-276.
- Tang JY: Inhibiting the hedgehog pathway in patients with the basal-cell nevus syndrome. N Engl J Med 2012; 366(23): 2180-2188.
HAUSARZT PRAXIS 2013; 8 (10): 35-37.











