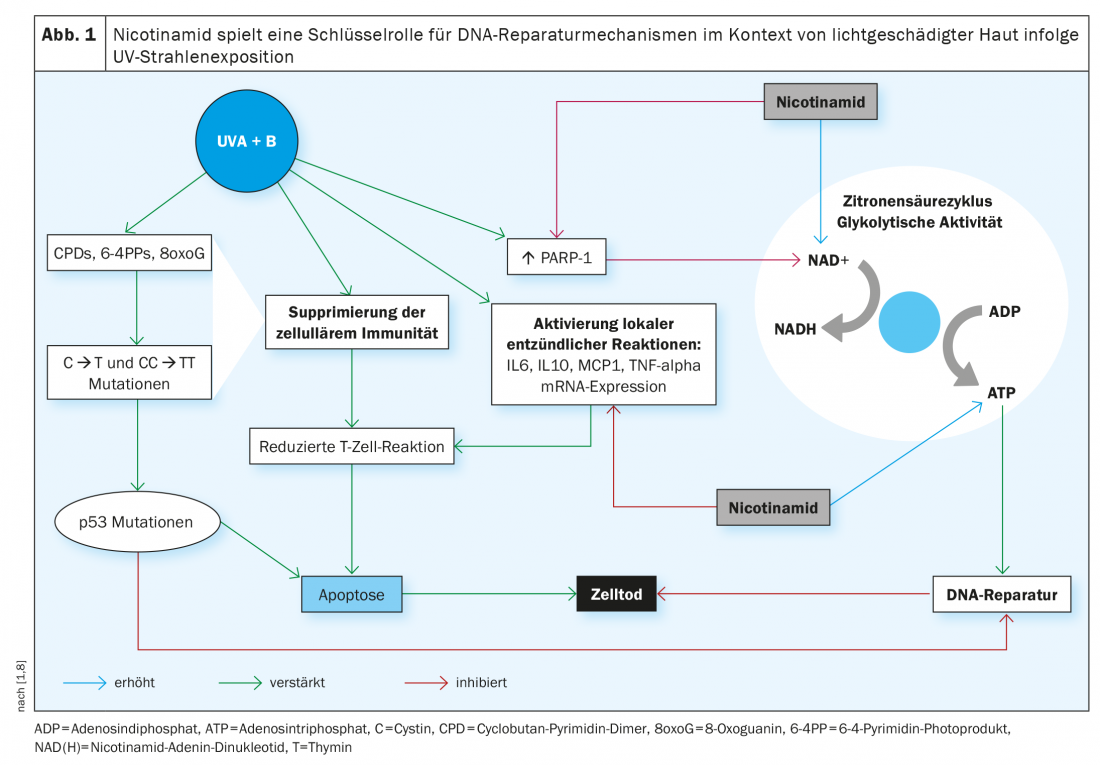
It is well known that UV radiation exposure is considered a major cause of non-melanocytic skin cancer by damaging DNA and inhibiting antitumor immunity. A reduction in intracellular ATP concentration, the main cellular energy source, plays an important role in this process. Nicotinamide is a cofactor for the provision of cellular ATP and promotes DNA repair mechanisms. The hypothesis of preventive effects of nicotinamide have been confirmed especially for secondary prevention of non-melanocytic skin cancer.
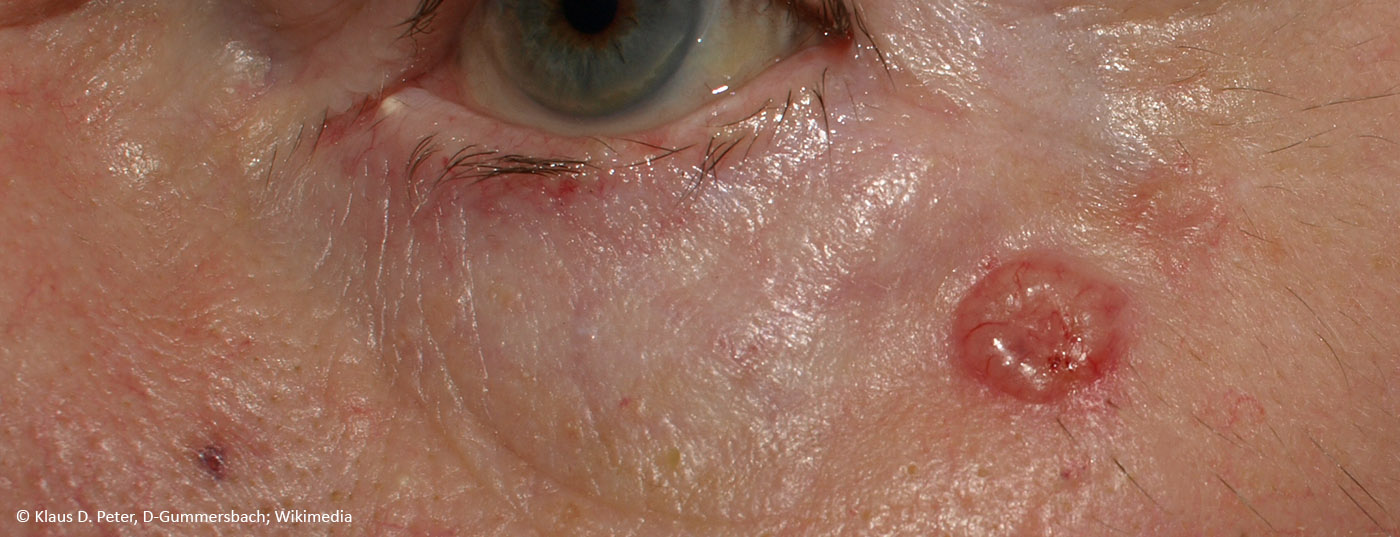
The incidence of non-melanocytic tumors (NMSCs) has risen sharply in recent years. Protection from UV radiation represents the most important part of skin cancer prevention; in addition, other skin cancer prevention strategies are being explored. Recently, there have been increasing reports of a potential benefit of phytochemical cell-protective compounds for the prevention of NMSC. At the virtual EADV Annual Meeting in October 2020, Prof. Yolanda Gilaberte Calzada, MD, from Miguel Servet University Hospital Zaragoza (Spain), spoke on oral prevention of skin cancer [1].
Nicotinamide promotes DNA repair
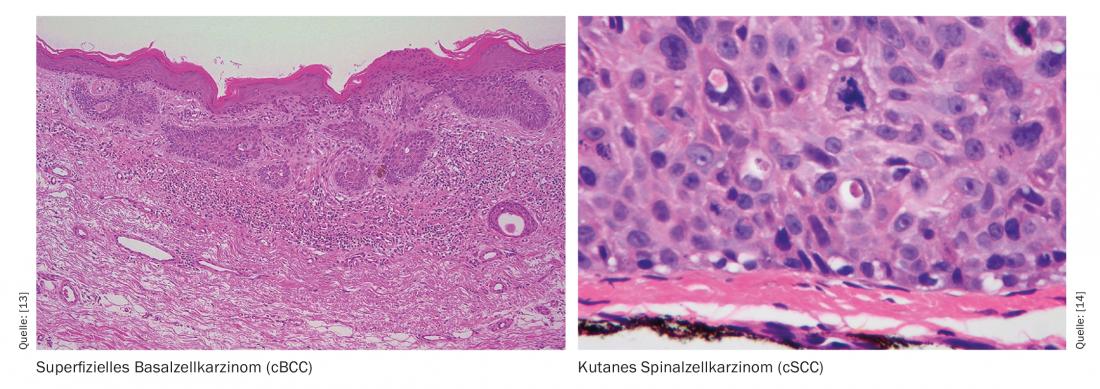
The current S2k guideline basal cell carcinoma of the skin (cBCC) recommends the oral use of nicotinamide at a dosage of 500 mg twice daily for secondary prevention, and studies have shown that over a 12-month treatment period, the incidence rate of squamous cell carcinoma (cSCC) was reduced by 30% [2,15]. What is the basis of the postulated preventive effect of this phytochemical substance? UV radiation exposure is known to be a major cause of NMSC by causing DNA damage and reducing antitumor immunity. This is accompanied by a depletion of intracellular adenosine triphosphate (ATP) concentration, the cell’s main source of energy. Nicotinamide counteracts this by blocking the inhibitory effect of UV radiation on ATP production and minimizing UV-induced immunosuppression (Fig. 1) [3,4]. Chemically, nicotinamide is the amide form of vitamin B3 – an important vitamin for many metabolic processes in the organism, which is only produced by the body in small quantities and must therefore be taken in with food. And it is a precursor of nicotinamide adenine dinucleotide (NAD) and of nicotinamide adenine dinucleotide phosphate (NADP), both co-enzymes involved in various metabolic processes. Among other things, NADP is an essential factor for intracellular ATP production and thus plays an important role in DNA repair mechanisms. NADPH is the reduced form of NADP and a derivative of NADH (Fig. 1).
Incidence reduction in high-risk groups
The hypothesis that oral nicotinamide treatment is associated with a reduction in the incidence of NMSC was confirmed empirically. In the Australian phase III ONTRAC (“Oral Nicotinamide to Reduce Actinic Cancer”) study, regular intake of nicotinamide reduced the risk of developing non-melanocytic skin cancer in at-risk individuals [5]. In this double-blind randomized trial, high-risk patients (n=386) received either 2× 500 mg nicotinamide or placebo daily for 12 months. “High-risk” was defined as having at least two NMSC tumors within the past 5 years. The average age of the study participants was 66 years. After 12 months, 23% fewer new NMSC cases had occurred in the nicotinamide group compared to placebo (p=0.02). The number of new actinic keratoses was 11% lower after 3 months and 13% lower after 12 months. Six months after discontinuation of nicotinamide, however, no significant differences were measurable between the two groups, so the protective effect appears to be limited to the treatment period. According to the authors, in order to be able to make clearer statements about preventive effects, a study over a longer period of time with higher doses could be informative; the tolerability of nicotinamide treatment proved to be good in this study.
Based on the results of the ONTRAC study, Chen et al. is conducting a Phase II study to evaluate the effects of nicotinamide on NMSC incidence in organ transplant recipients, a patient population in which skin cancer and actinic keratosis are more common compared to immunocompetent individuals [6,8]. After a period of 6 months, there was a 35% reduction in the nicotinamide group with respect to NMSC incidence compared with placebo. The fact that the significance level was not reached is attributed to the small sample size in a review published in 2019. The authors cite as further evidence of efficacy in organ transplant patients a study by Drago et al 2017 (n=38), in which a reduction in the size of actinic keratoses was observed in 88% of patients treated with nicotinamide, with complete remission in 42%, and the incidence rate was zero [7].
Evidence of efficacy of nicotinamide in the dermatological field is not limited to skin cancer prevention. For example, a review published in 2017 found symptom relief in pruritus, attributed to anti-inflammatory effects and improvement in epidermal barrier function [9]. Furthermore, there are indications of positive effects in bullous pemphigoid [10] as well as in other dermatological diseases. However, the best evidence base currently exists in the area of skin cancer prevention.
What about other phytochemicals for skin cancer prevention?
The current American Academy of Dermatology (AAD) guideline recommends acitretin for the prevention of NMSC and for the treatment and prophylaxis of actinic keratosis in organ transplant patients [11]. The suggested dose is 10 mg/d with an increase of 10 mg at 2-4-week intervals. The target dose is 20-25 mg/d [1]. According to clinical studies, the duration of treatment can be up to 1 year, whereby the measurable preventive effects are also limited to the treatment period according to current knowledge [1]. Regarding isotretinoin and nonsteroidal anti-inflammatory drugs (NSAID) such as aspirin or ibuprofen, the evidence on possible preventive effects for primary or secondary prevention of NMSC is inconsistent and dependent on patient characteristics [1,12]. In summary, with regard to chemoprevention by oral substitution, the findings on nicotinamide are currently the most promising, although its use must be weighed up individually in each case.
Source: EADV Annual Meeting 2020
Literature:
- Gilaberte Y: Oral Prevention of Skin Cancer. Prof Dr Yolanda Gilaberte, EADV Annual Meeting, 31.10.2020.
- AWMF: s2k guideline basal cell carcinoma of the skin, 2018, www.awmf.org/uploads/tx_szleitlinien/032-021l_S2k_Basalzellkarzinom-der-Haut_2018-09_01.pdf
- AWMF: S3 Guideline. Actinic keratosis and squamous cell carcinoma of the skin, 2020, www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/Downloads/Leitlinien/Aktinische_Keratosen_und_PEK/LL_Aktinische_Keratosen_PEK_Langversion_1.1.pdf
- Bayerl C: Skin aging: What anti-aging can do, Pharmazeutische Zeitung (Online), 08.08.2017.
- Chen AC, et al: N Engl J Med 2015; 373(17): 1618-1626.
- Chen AC, et al: Br J Dermatol 2016, 175(5), 1073-1075. doi: 10.1111/bjd.14662
- Drago F, et al : Eur J Dermatol 2017; 27: 382.
- Snaidr VA, Damian DL, Halliday GM: Experimental Dermatology 2019, https://onlinelibrary.wiley.com/doi/full/10.1111/exd.13819
- Forbat E, et al: Clin Exp. Dermatol 2017; 42(2): 137.
- Chen AC, et al: Australas. J Dermatol 2014; 55(3): 169.
- Kim JYS, et al: Guidelines of care for the management of cutaneous squamous cell carcinoma. JAAD 2018; 78(3): 560-578.
- Herold M, et al: Dermatol Surg 2019; 1442-1449.
- Wikimedia, https://doi.org/10.1155/2011/496910
- Wikimedia, DOI:10.1155/2011/210813
- Stratigos AJ, et al: European Journal of Cancer 2020; 128, https://doi.org/10.1016/j.ejca.2020.01.007
DERMATOLOGIE PRAXIS 2021; 31(1): 44-45 (published 2/23/21, ahead of print).