Smoking tobacco products is associated with significant health risks. Nearly half of the people in Switzerland who smoke would like to quit smoking. Various therapeutic options are available today for this purpose. They range from minimal intervention to intensive drug-assisted treatment. This can achieve abstinence rates of over 30%.
Smoking, the most common and dangerous form of tobacco consumption, takes the form of cigarettes in about 90% of cases in Switzerland. Cigars, pipes, or smokeless forms of tobacco use play a minor role. A survey on the prevalence of smoking among a representative sample of the population (Tobacco Monitoring Switzerland) revealed the following key results:- The proportion of smokers in Switzerland is 27%.
- The amount consumed by daily smokers averages 14.2 cigarettes/day.
- It smokes 30% of men and 24% of women.
- The highest rate is found between the ages of 20 and 24 (42% of men, 36% of women).
- Nearly half of people who smoke (48%) want to quit [1].
Health risks of smoking
Smoking is associated with significant health risks. Its vasodamaging effect leads to increased heart attacks, strokes and peripheral vascular occlusions. Its carcinogenic effect increases the risk of malignancies of various organs (lung, pharynx, larynx, esophagus, stomach, urinary bladder, uterus). Smokers have delayed wound healing, increased risk of infection after surgical procedures, and altered function of numerous genes. Smokers have a shortened life expectancy by many years compared to non-smokers. Smoking during pregnancy can be associated with fetal tobacco syndrome, deficiency development, and prematurity.
Diagnosis dependence
A specific medical history should be obtained for each smoker. The most important features are summarized in Table 1.
A diagnosis of tobacco dependence (ICD-10: F17.2) requires that three or more of the following criteria have been met simultaneously during the past 12 months:
- A strong desire or some kind of compulsion to use tobacco
- A decreased ability to control the onset, cessation, and amount of tobacco use
- A physical withdrawal syndrome upon cessation or reduction of use.
- Proof of a tolerance
- Progressive neglect of other pleasures or interests in favor of tobacco use
- Continued tobacco use despite evidence of clear harmful consequences [2].
The best known and most commonly used internationally is the Fagerström Test for Nicotine Dependence (FTND), which uses six questions to assess smoking behavior [3]. Depending on the point value (0 to 10) the severity of the dependency can be graduated from low to very high.
Parameters for the objectification of smoking behavior
For research purposes and in therapy, it can sometimes be helpful to objectify smoking behavior by means of biochemical parameters. The most common are the determination of cotinine levels in serum, urine or saliva and the measurement of carbon monoxide levels in the breath.
Cotinine is a degradation product of nicotine resulting from oxidation. Because of its significantly longer half-life (up to 40 h), cotinine opens a larger observation window for abstinence monitoring than the determination of nicotine (HWZ up to 2 h).
Inexpensive measuring devices from various manufacturers allow the determination of carbon monoxide (CO) in exhaled air. The level of the CO reading (measured in ppm) reflects the strength of the smoking behavior. This provides a parameter that allows , among other things, to objectify abstinence success in the context of weaning treatment.
Therapy
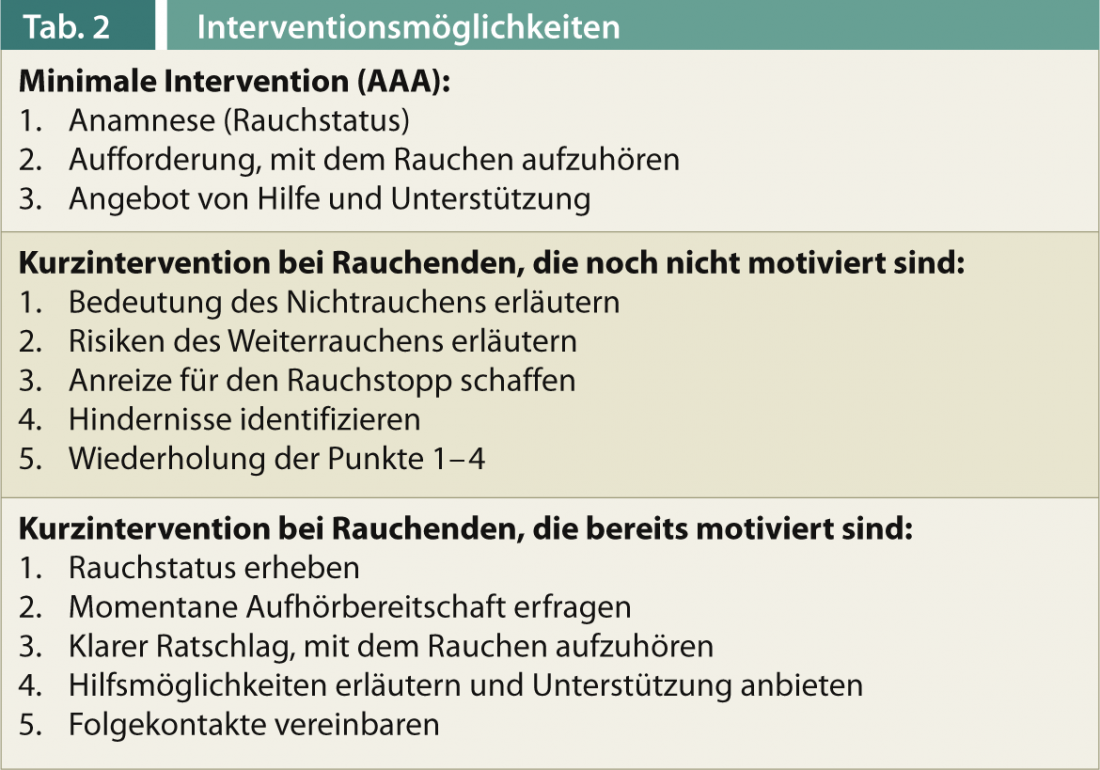
Inpatient therapy may be necessary to treat associated sequelae. However, actual smoking cessation remains the domain of outpatient therapy. Family practice is particularly well suited for this purpose [4]. Intervention options of varying intensity are available today. Minimal and brief interventions are summarized in Table 2. In addition, intensive treatment is also possible. It can be done as individual or group therapy in multiple sessions. A modular program that includes the following therapy modules, among others, has proven successful:
- Clarification and consolidation of the exit motivation
- Set the date to stop smoking
- Problem solving training
- Recognizing the risk of relapse
- Recidivism Management.
In combination with drug treatment, abstinence rates of over 30% can be achieved.
Drug treatment
Two strategies can be distinguished: nicotine substitution to facilitate withdrawal and medication administration to reduce the risk of relapse. Nicotine replacement therapy by means of patches, chewing gum or nasal spray is much more health-friendly than inhaling tobacco smoke with its thousands of harmful ingredients. In particular, the patch allows the maintenance of a consistent nicotine level, thereby alleviating withdrawal symptoms and reducing strong, relapse-inducing nicotine cravings (“craving”). Nicotine substitution is a first-line therapy, and is recommended for all cases of moderate to severe tobacco dependence. A treatment period of eight to twelve weeks with gradual dose reduction is recommended.
Two medications are approved for drug relapse prevention, bupropion and varenicline. Both are available by prescription. Bupropion acts via reuptake inhibition of dopaminergic and noradrenergic neurotransmission, and is also marketed as a drive-enhancing antidepressant. Varenicline reduces smoking cravings via its action at the nicotinic acetylcholine receptor. There is convincing evidence-based efficacy for both drugs.
Treatments without proof of efficacy
Many ex-smokers propagate the abrupt voluntative smoking cessation without support or treatment, the so-called “quit method”. Hypnotherapy, acupuncture or various homeopathic medicines are also popular. All these procedures lack convincing proof of efficacy. They can therefore not be recommended from a medical point of view.
The oral tobacco “snus” popular in Scandinavian countries has been discussed as a smokeless alternative for tobacco cessation. Because of its high nicotine content, snus may prevent withdrawal symptoms in the short term, but it seems more likely to maintain dependence in the long term [5].
Electric cigarettes have become increasingly popular in recent years. They are promoted as a smoke- and tobacco-free and thus less harmful alternative to conventional cigarettes. How helpful or harmful e-cigarettes actually are, however, cannot be reliably answered at present. The U.S. Food and Drug Administration (FDS) already warned against their use [6].
Prof. Dr. med. Gerhard Wiesbeck
Literature:
- Keller R, et al: The tobacco consumption of the Swiss resident population from 2001 to 2010. Tobacco monitoring – Swiss survey on tobacco consumption. Zurich: Psychological Institute of the University of Zurich, Social and Health Psychology 2011.
- From Dilling H, et al: ICD-10 Chapter V (F). International classification of mental disorders. Clinical diagnostic guidelines (8th rev. ed.). Verlag Huber, Bern 2011.
- Heatherton TF, et al: Brit J Addict 1991; 86: 1119-1127.
- Wiesbeck G: InFo Neurology&Psychiatry 2004; 2(1): 20-23.
- Lund KE, et al: Nicotine Tob Res 2010; 12: 817-822.
- FDA: FDA and Public Health Experts Warn About Electronic Cigarettes 2009. Available from: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm173222.htm
- Drug Commission of the German Medical Association (2010): Recommendation on the therapy of tobacco dependence. Prescribing in Practice 2010; 37 (Special Issue 2).