Allergies to arthropods in general and insects are a common problem and encompass a wide spectrum of complaints. For example, the general allergic reactions to the hymenoptera bee, wasp and, in the international context, the red fire ant, some of which are quite life-threatening, should certainly be mentioned. Very good diagnostic methods exist for these allergies, and excellent and highly effective immunotherapies also exist for bee and wasp venom allergies. Mosquito bites can often cause very pronounced local hypersensitivity reactions, but are very rarely responsible for general allergic reactions. Besides, various insects resp. whose excrement triggers inhalation allergies, such as cockroaches, ladybugs, red mosquito larvae or silkworms. In regions where insects are enjoyed as food, corresponding allergies up to anaphylaxis have also been described after ingestive ingestion. Finally, other arthropods, such as dust mites or crustaceans, also contain important allergens that can lead to relevant cross-allergies via certain proteins.
Arthropods include insects (three pairs of legs), arachnids (four pairs of legs), centipedes, millipedes, and crustaceans (such as shrimp, crabs, lobsters). The variety is enormous: the class of insects alone comprises about six million species. In addition to insects, other arthropods such as dust mites or crustaceans are responsible for quite common allergic reactions and are therefore also briefly discussed at the end of this article.
Allergies to hymenopterans as triggers of the “classical” insect venom allergy
Allergic reactions to hymenopteran venoms, especially those of bees and wasps, are common and well known. They affect about 1-3% of the population in Switzerland. The spectrum of symptoms ranges from excessive local reactions to severe anaphylactic reactions with asthma, shock or circulatory arrest. On average, three to five deaths due to insect venom allergy occur in Switzerland each year – in most cases, however, additional risk factors are present, such as pre-existing cardiovascular diseases with corresponding comedication, older age, hypertryptasemia/mastocytosis or additional heavy physical exertion.
Nowadays, the use of molecular allergy diagnostics to measure specific IgE and intracutaneous skin threshold determination can very accurately distinguish actual double sensitizations from cross-reactions between the two poisons. While the venom of the common wasp (Vespa germanica) and that of the hornet (Vespa crabro) hardly differ with regard to allergens, that of bees is composed differently in essential parts. Bumblebees, on the other hand, hardly play a role due to their good nature and very low stinging propensity, but their venom is partially comparable to bee venom.
The often expressed statement that each subsequent allergic reaction is worse than the previous one is only true in about one third of the cases; in more than 60%, a renewed stinging reaction is constant, less severe or even absent. In the case of a new sting, this can again change in both directions. Decisive for the consultation of a patient are therefore, in addition to the severity of the allergic reaction, the frequency of the stings as well as the subjectively suffered loss of quality of life due to the “having to watch out” resp. the fear of being stung again. Necessary in case of general allergic reactions in the history and proven sensitization to a hymenopteran venom is the administration of emergency medication (oral steroids of 50-100 mg and one to two tablets of an H1-blocker, in case of more severe symptoms also an adrenaline autoinjector).
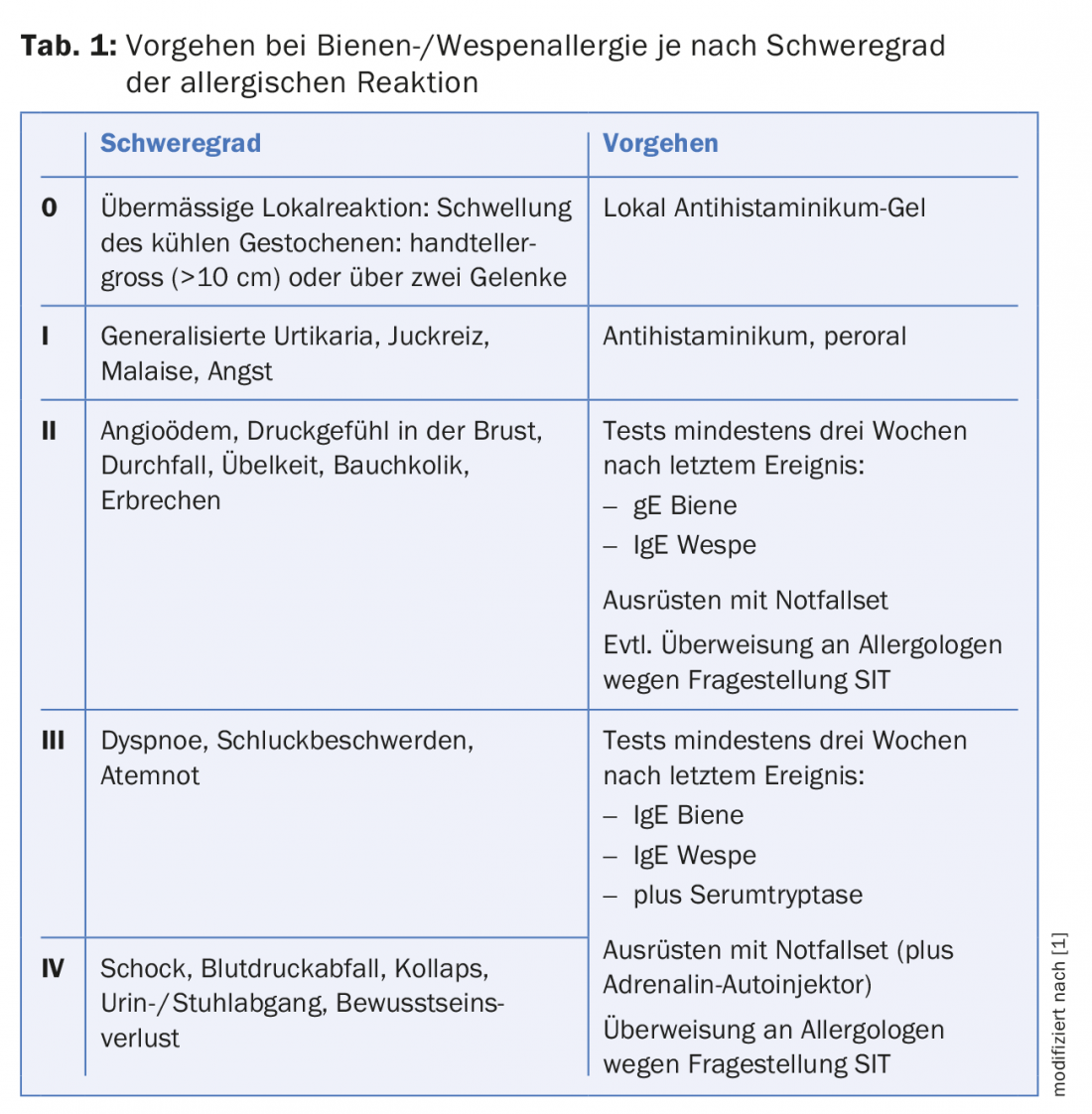
In addition, immunotherapy is a costly but safe and highly effective treatment method for severe bee and wasp venom allergies. Protection can be achieved in 90-95% of patients with wasp venom immunotherapy, which usually lasts five years; with bee venom allergies, the success rate is only slightly lower. Table 1 summarizes the most important diagnostic steps for the workup of bee and wasp venom allergies depending on the severity of the allergic reaction.
Hymenoptera also include ants, especially the red fire ant (Solenopsis invicta). Their venom is related to that of wasps, but in addition to stings, it can also be applied by bites of ants. In addition to severe local reactions, general allergic reactions are also possible here – accordingly, the red fire ant is quite feared in its distribution area, which includes the southern states of the USA, Central and South America and the east coast of Australia. Local ants are very rarely responsible for allergies except in isolated reported cases.
This article will now additionally present allergies to some other insects – be it to their bites, stings, excrements or remains. For example, mosquitoes or silkworms can cause actual allergic, even anaphylactic reactions in addition to pronounced local reactions.
Allergic reactions to mosquito bites
Mosquitoes are found worldwide and their bites can cause reactions of varying degrees of severity, ranging from very common, mainly annoying local reactions to overall distinctly rare general allergic reactions. Even deaths due to mosquito bite allergy are described rarely, but credibly. Typical and frequent reactions, however, are mostly unpleasant, because strongly itching, to sometimes painful local reactions at the sting site. Systemic allergic reactions are extremely much rarer than those resulting from a sting of the hymenopteran bees and wasps. Allergic general reactions with urticaria, asthma or even anaphylactic shock have so far been published in the entire literature with only just over 30 cases.
In addition to wheals, local reactions may include vesicles or blisters, ecchymosis, and even arthralgia, which often occur two to six hours after the mosquito bite but may persist for days or weeks. Both the attractiveness of certain “victims” in the eyes of mosquitoes and the local and immunological response to a bite are highly host-specific. So in a group of several people, some may well be more affected than others. In addition, people bitten with strong local reactions naturally perceive mosquito bites more clearly than those with hardly any reactions, which are therefore almost inapparent. Particularly noteworthy is the so-called “Skeeter” syndrome with skin manifestations similar to folliculitis and with fever appearing within a few hours. The syndrome can be deceptively similar to an infection. The rapid progression within hours and the presence of IgE against mosquitoes may contribute to the differentiation. Significantly more common are bacterial superinfections following scratching of a sting site. The transmission of pathogens such as plasmodia (malaria), flaviviruses (yellow fever) or, more recently, the zika virus through mosquito bites is also a relevant problem worldwide.
If a systemic general reaction is suspected, spec. IgE against mosquito venom should be determined in serum, and measurement of serum tryptase is also recommended, since patients with elevated values or even actual mastocytosis tend to have more severe reactions. With increasing knowledge of the molecular structure of mosquito venom allergens, increasingly differentiated diagnostics will probably be possible in the near future. Skin tests with mosquito venom are only practical with reservations due to the low level of standardization. Similarly, hardly any useful extracts are available for immunotherapy; these still consist of whole-body extracts, which for understandable reasons contain only few salivary proteins relevant to the allergy.
The most effective prevention is therefore the use of repellents and – in the case of Anopheles mosquitoes, which bite mainly at dusk – mosquito nets. Vitamin B-based products are also said to have a certain mosquito-deterrent effect. For stings that have already occurred, topical steroids, mixed with a disinfectant if necessary, and/or systemic H1 blockers can be used.
Insects as triggers of inhalation allergies
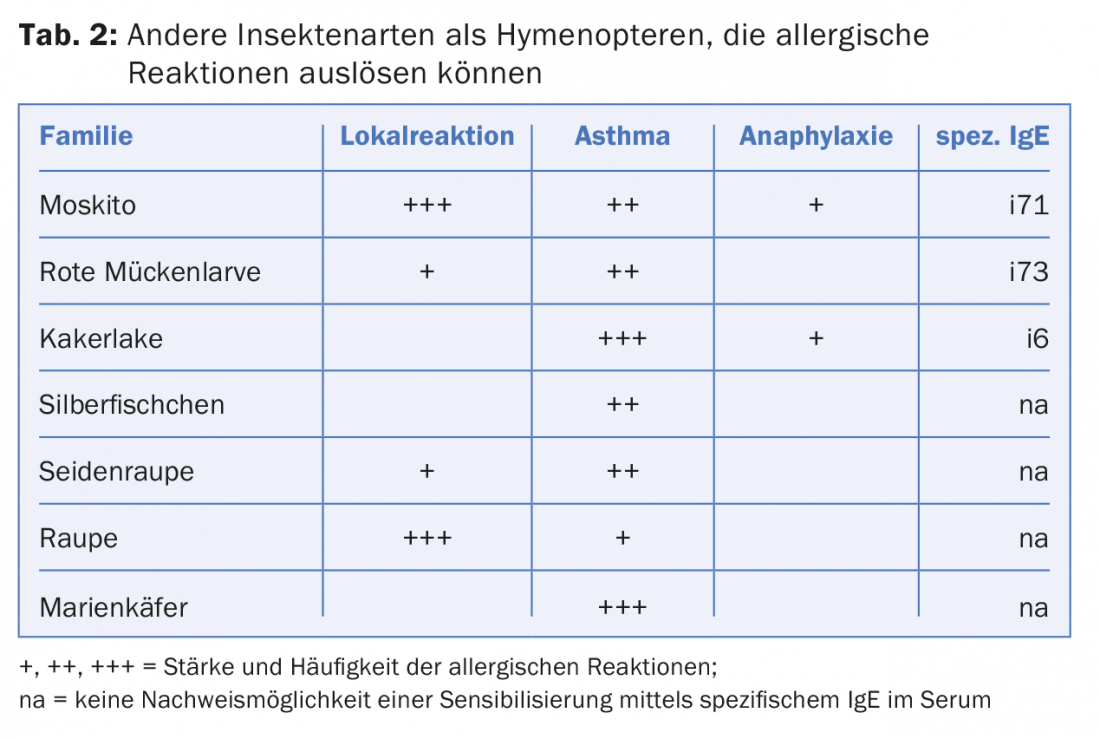
According to the huge number of insects, IgE-mediated sensitization to various other insects can be observed. Inhalation allergies with rhinoconjunctivitis or bronchial asthma are common. Worldwide, cockroaches are even the most common triggers of allergic asthma. Particularly in the highly populated countries of the subtropics, such as Brazil, India or Indonesia, cockroaches almost the size of a thumb are sometimes found. their excrement important allergenic components of house dust. In addition, inhalation allergies are also caused by ladybugs and other insects. their dust possible after death, for example, in a screed. Red mosquito larvae are often added to fish food as a source of protein and can therefore cause dyspnea if sensitized when feeding aquarium fish. Finally, silkworms can cause symptoms either as an occupational allergen during silk processing or, much less frequently, by inhalation or contact with silk-containing bedding or garments made of unprocessed wild silk (tab. 2).
Allergies caused by other arthropods – from respiratory to food allergies.
Other arthropods can act as inhalation allergens, through direct venom contact (touch, stings, bites), on the one hand, and as food allergens, on the other. In addition to the actual spiders, arachnids also include scorpions, ticks and mites. House dust mites are well known as triggers of inhalative allergies and are even the most important trigger of year-round allergic bronchial asthma in this country. In addition, certain ticks, such as the pigeon tick (Argas reflexus), can also trigger actual allergic reactions with their bite. Typical here are nocturnal allergic reactions in persons living near a pigeon nest, where the pigeon ticks bite humans at night as a false host.
Centipedes and millipedes can cause toxic, but in rare cases allergic reactions due to secreted toxins. However, the representatives occurring in Switzerland are harmless in this respect except for triggering at most slight skin irritations.
Crustaceans such as shrimp, crab or lobster, especially when eaten as food, cause allergic reactions that can be very severe, potentially even life-threatening. In about 50% of cases, tropomyosin, which can act as an allergen in insects and worms as well as snails, is responsible. It can trigger allergic symptoms by inhalation (house dust mites) or when these creatures are eaten (Fig. 1).
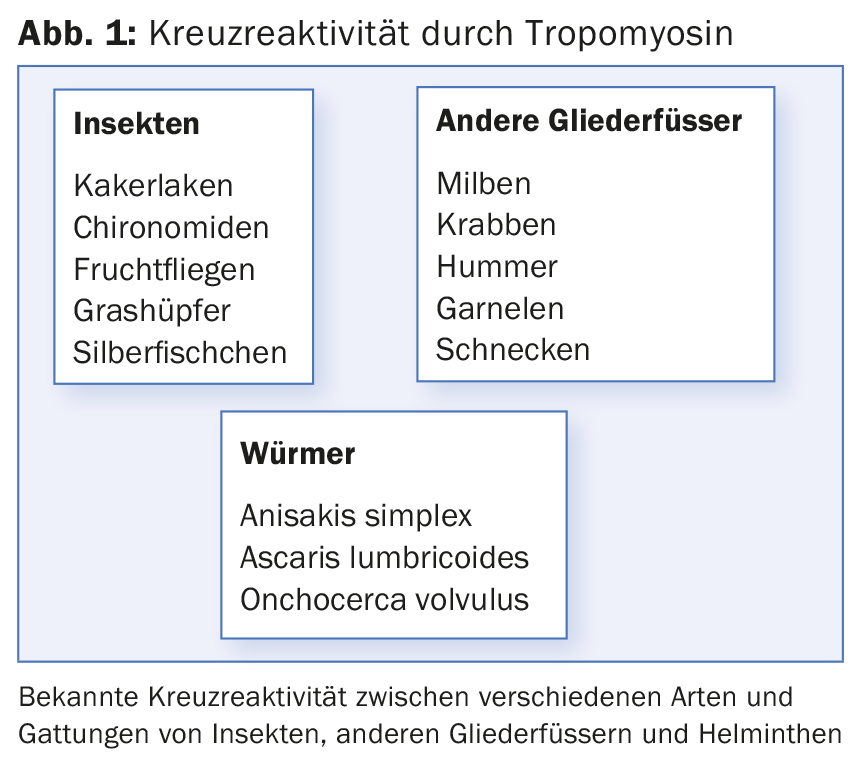
In and of itself, tropomyosin is also found in more highly developed vertebrates, but does not seem to be recognized as an allergen there due to its strong homology with human tropomyosin (Pen m 1). In the other 50% of patients who are allergic to crevettes, for example, other proteins (such as arginine kinase pen m 2, myosin light chain pen m 3, or troponin pen m 6) are responsible for such reactions. The cultural and ethnic background plays an important role in the sensitization spectrum – as does the fact whether the whole shrimp (highly allergenic) or only its abdomen is eaten. In case of unclear or severe anaphylactic reactions after seafood consumption, further allergological investigation with skin testing with native material and corresponding serological, molecularly based clarification is advisable in any case.
Literature:
- CK-Care: Hymenoptera venom allergies – tips for practice. V01/2013. www.ck-care.ch/merkblatter.
Further reading:
- Peng Z, Simons FE: Advances in mosquito allergy. Curr Opin Allergy Immunol 2007; 7: 350-354.
- Dhami S, et al: Allergen immunotherapy for insect venom allergy: protocol for a systematic review. Clin Transl Allergy 2016 Feb 16; 6: 6.
- Potiwat R, Sitcharungsi R: Ant allergens and hypersensitivity reactions in response to ant stings. Asian Pac J Allergy
- Immunol 2015 Dec; 33(4): 267-275.
- Nakazawa T, et al: Asian ladybugs: a new seasonal indoor allergen. J Allergy Clin Immunol 2007; 119: 421-427.
- Perzanowski MS, Platts-Mills TA: Further confirmation of the relevance of cockroach and dust mite sensitization to inner-city asthma morbidity. Clin Exp Allergy 2009; 39: 1291-1293.
- Peng Z, et al: Mosquito salivary allergen Aed a 3: cloning, comprehensive molecular analysis, and clinical evaluation. Allergy 2016 May; 71(5): 621-628.
- Seebach J, et al: Forest ant venom: a rare cause of anaphylactic reactions in Switzerland. Schweiz Med Wochenschr 2000; 130: 1805-1813.











