Prof. Ludwig Kappos, M.D., Basel, Switzerland, together with Prof. Stephen L. Hauser, M.D., Director of the UCSF Weill Institute for Neurosciences, San Francisco, USA, chaired the Steering Committee of the two studies ASCLEPIOS I and II. These studies evaluated ofatumumab compared with teriflunomide in patients with relapsing-remitting multiple sclerosis (RMS) [1]. In the following interview, he describes the specific properties of this anti-CD20 antibody, explains the most important study results and describes his personal experience with ofatumumab.

Prof. Dr. med. Dr.h.c.mult. Ludwig Kappos, Director Research Center for Clinical Neuroimmunology and Neuroscience Basel (RC2NB)
Prof. Kappos, how does the mechanism of action of ofatumumab differ from that of other antibodies used in MS?
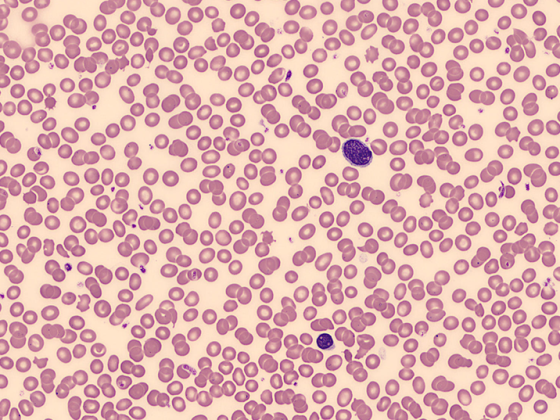
Ofatumumab is a B-cell-depleting antibody. That is, by binding to CD20, it leads to destruction of B cells in the periphery. However, this leaves out the early and late developmental stages of B cells because they do not express the CD20 receptor. This is also used for the other CD20 antibodies as an explanation for the quite good long-term tolerability of this substance group.2-4 However, unlike the other CD20 antibodies, ofatumumab binds to both extracellular components of the CD20 receptor, not just one.5 As a result, for example, the similarity between rituximab and ocrelizumab in terms of binding site is much greater, whereas ofatumumab differs in this respect. However, what implications this has for what we want to see in MS is not so clear yet.
Does it matter that ofatumumab is a fully human antibody?
In terms of mechanism of action, probably not. However, one would assume that this makes the substance better tolerated because the human immune system has fewer starting points to recognize ofatumumab as foreign and react against it.6 In theory, this is certainly an advantage. How big the difference really is in practice compared to the other antibodies, especially the humanized antibodies, we lack data from direct comparisons.
In your view, what are the most important results of the two ASCLEPIOS studies in terms of the efficacy of ofatumumab in RMS?
The efficacy of ofatumumab in RMS is certainly very impressive.1 One advantage in terms of efficacy assessment is that ofatumumab was compared with a drug that has no or very few compound-specific side effects.7-9 This means that the blinding in the study was certainly better than if, for example, an interferon – with the known flu-like and local injection side effects – had been used as a comparator.10, 11 In addition to the relatively low local and systemic side effects of ofatumumab1 itself, this means that one can probably rely on a higher reliability of assessments by patients and also study physicians. Specifically, in the trials, ofatumumab versus teriflunomide in a population with active RMS achieved a 50% to 60% reduction in annual relapse rate, depending on which of the two ASCLEPIOS trials one looks at.1 In addition, there was also an effect on disability progression. The incidence of confirmed disability progression was significantly reduced by approximately one-third compared with teriflunomide-a drug that itself had a demonstrated effect on disability progression compared with placebo in both main registration trials8, 9 .1 MRI showed near to complete suppression of active lesions with ofatumumab.
Gd-positive lesions decreased over 90%. The new or enlarging T2 lesions were also radically reduced.1 Not significantly different from teriflunomide was the change in brain volume affected over time.1 It should be noted that teriflunomide has been shown to have a positive effect on volume reduction compared with placebo in other studies.12 In the ASCLEPIOS trials, it was also planned from the outset to measure serum neurofilament light chains as an important secondary outcome parameter, a now established specific measure of neuroaxonal damage or protection by ofatumumab. Here, there was a clear effect in that there was virtually normalization of this marker under ofatumumab in both ASCLEPIOS studies. Here, the effect already appears after three months and is then practically at the level of a normal population after 12 and 24 months.1 This means that we have clear evidence here that there is also a positive effect of ofatumumab in terms of tissue integrity.
What points are relevant regarding the safety of ofatumumab?
I think it’s important for patients to know that when they initiate therapy with ofatumumab, they don’t need any concomitant medications to dampen any allergic reactions.2 This is in contrast to infused antibodies, for which prophylactic measures must be used consistently from the outset and in some cases even during the further course of treatment.3 Patients can also usually continue subcutaneous injections of ofatumumab at home without problems after the first injection. In the observation period that we survey for ofatumumab so far, there were no differences compared to the side effect profile known from the controlled studies regarding a susceptibility to infections. Also, an effect on the incidence of malignancies, initially feared on the basis of observations with other anti-CD20 antibodies, was not confirmed.13
How well does the patient population in the two studies reflect the patients treated by Swiss neurologists?
I think both studies captured a fairly typical population of patients with active relapsing-remitting MS. Most had been suffering from the disease for several years, and in about one third of the patients the diagnosis was less than three years ago.1, 14 The similarity to the MS population seen by a neurologist here in Switzerland is thus quite high.
Which patients are particularly suitable for treatment with ofatumumab?
I think the B-cell-depleting drugs are the first to allow the threshold to be kept low for the use of a highly effective treatment. This means that there is an increasing trend towards early treatment with these highly effective drugs.15 Ultimately, it is the first truly highly effective active principle that is also well tolerated and can be administered with a clear conscience to people who are still little affected by the disease.3, 14, 15, 18 This with the aim of protecting them from harm in the future. That is certainly an essential point. Thanks to the possibility of subcutaneous injection, and thus the lack of expense for an infusion every six months, ofatumumab may also be somewhat more accessible.2, 3 However, patients must decide individually with their neurologist which therapy suits them best.
What should be considered before starting treatment with ofatumumab?
If the start of therapy is not extremely urgent, in today’s world, for example, patients would be administered the Corona vaccine first and then therapy would not begin until two weeks after completion of the vaccination. This is the general recommendation.2 Generally, chronic infections are screened for, vaccination history is obtained, and vaccination gaps are closed as much as possible before treatment is initiated. A differential blood count, and in some centers a FACS analysis is also ordered, is also used to roughly analyze whether there is any evidence of immunodeficiency before therapy is started.2
Does it matter what prior therapy patients received prior to ofatumumab use? Is there a distance that needs to be maintained?
There are no data on this so far, but in the ASCLEPIOS studies certain distances were observed.1 Normally, it is only necessary to maintain a distance to other depleting therapies, for example to alemtuzumab, which is not very frequently used, or to cytostatic drugs. If someone is switched from ocrelizumab to ofatumumab, they would not start the new therapy before the end of six months from the last dose of ocrelizumab. One would not normally keep a greater distance from oral medications. In the case of teriflunomide, flushing out the substance is recommended. Once elimination is complete, ofatumumab can be started immediately. There are no such clear recommendations for S1P receptor modulators. We ourselves say that lymphocytes should be close to normal before starting.2
In your opinion, at what point within the therapeutic algorithm of MS should ofatumumab ideally be used?
Ofatumumab is one of those drugs that you should consider using early on. Within the scope of the official indication of the drug, we do not see any restrictions in this regard.2 The assumption, which is also suggested by the subgroup analyses, is that early treatment is probably even more efficient than late treatment.14,15 From there, ofatumumab is certainly a first-line drug that I offer myself.
What does it mean for both patients and neurologists to have ofatumumab available as another treatment option?
I think that overall, with the B-cell-depleting drugs, it has become easier to use a very effective therapy from the beginning. Ofatumumab’s ease of subcutaneous administration and good tolerability make this even easier.2
What is your own experience with ofatumumab so far?
Overall, ofatumumab is proving to be very well tolerated. For patients who want to maintain their normal lifestyle, the treatment does not involve any special requirements or burdens.2 Ofatumumab, for example, cannot be compared in terms of tolerability with drugs such as interferons, which need to be injected more frequently and can lead to local reactions and flu-like side effects.10,11
There are more than twelve disease-modifying treatment options in Switzerland that are classified as moderately or highly effective. Is there a need for ofatumumab at all?
One would almost like to ask the opposite. How many of the previous drugs are still needed now that ofatumumab is available? The antibody’s mode of action and experience to date have the potential to make ofatumumab a game-changer. With one reservation, however, as we do not yet have any long-term data. MS lasts 30 or more years and if we treat it well probably 50 or more years. From this point of view, vigilance is certainly still needed on the part of all those involved. But so far, we have no evidence that we are taking on a mortgage with ofatumumab and other B-cell-depleting therapies that we will end up not being able to pay.13
This article was realized by Novartis Pharma Schweiz AG, Suurstoffi 14, 6343 Rotkreuz, Switzerland
References: 1 Hauser SL et al. Ofatumumab versus Teriflunomide in Multiple Sclerosis. N Engl J Med. 2020;383(6):546-557. 2 Expert information KESIMPTA® (ofatumumab), www.swiss- medicinfo.ch; as of January 2021. 3 Professional information Ocrevus® (ocrelizumab). www.swissmedicinfo.ch; as of April 2021. 4 Hauser SL et al. Safety of Ocrelizumab in Multiple Sclerosis: Updated Analysis in Patients with Relapsing and Primary Progressive Multiple Sclerosis. Presented at the 8th Joint ACTRIMS-ECTRIMS Meeting, MSVirtual2020, September 11-13, 2020, ePoster P0389. 5 Klein C et al. Epitope interactions of monoclonal antibodies targeting CD20 and their relationship to functional properties. MAbs. 2013;5(1):22-33. 6 Ruuls SR et al. Novel human antibody therapeutics: the age of the Umabs. Biotechnol J. 2008;3(9-10):1157-1171. 7 Specialty Information Aubagio® (teriflunomide). www.swissmedicinfo.ch; as of February 2021. 8 O’Connor P et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med. 2011;365(14):1293-303. 9 Confavreux C et al. Oral teri- flunomide for patients with relapsing multiple sclerosis (TOWER): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13(3):247-256. 10 Technical information Rebif® (interferon beta-1a). www.swissmedicinfo.ch; as of February 2020. 11 Technical information Avonex® (interferon beta-1a). www.swissmedicinfo.ch; as of July 2020. 12 Vermersch P et al. Teriflunomide versus subcutaneous interferon beta-1a in patients with relapsing multiple sclerosis: a randomised, controlled phase 3 trial. Mult Scler. 2014;20(6):705-16. 13 Cross A et al. Safety experience with extended exposure to ofatumumab in patients with relapsing multiple sclerosis from phase 2 and 3 clinical trials. Presented at the 8th Joint ACTRIMS-ECTRIMS Meeting, MSVirtual2020, September 11-13, 2020, ePoster P0234. 14 Gärtner J et al. Benefit-risk of Ofatumumab in Treatment-naïve Early Relapsing Multiple Sclerosis Patients. Presented at the 8th Joint ACTRIMS-ECTRIMS Meeting, MSVirtual2020, September 11-13, 2020, ePoster P0192. 15 Stankiewicz J et al. An argument for broad use of high efficacy treatments in early multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2020;7(1):636. 16 Schmierer K et al. Highly effective disease-modifying treatment as initial MS therapy. Curr Opin Neurol. 2021;34(3):286-294. 17 Samjoo IA et al. Comparison of ofatumumab and other disease-modifying therapies for relapsing multiple sclerosis: a network meta-analysis. J Comp Eff Res. 2020;9(18):1255-1274. 18 Hauser SL and Cree BAC. Treatment of Multiple Sclerosis: A Review. Am J Med. 2020;133(12):1380-1390.e2
KESIMPTA® Solution for injection in a Ready-to-use pen ▼ This medicinal product is subject to additional monitoring. For more information, see the Kesimpta SmPC/patient information leaflet on www.swissmedicinfo.ch. Z: 1pre-filled pen contains 20 mg ofatumumab in 0.4 ml solution for subcutaneous injection (50 mg/ml). I: Kesimpta is indicated for the treatment of adult patients with active relapsing forms of multiple sclerosis (MS). D: 20 mg as a subcutaneous injection: initial administration at weeks 0, 1, and 2, followed by subsequent monthly administrations beginning at week 4. KI: Hypersensitivity to the active ingredient or any of the excipients listed in the composition section, severely immunocompromised patients, presence of active infection, known active malignancies, initiation of therapy during pregnancy. VM: Warnings and precautions regarding injection-related reactions, infections, progressive multifocal leukoencephalopathy, hepatitis B virus reactivation, treatment of highly immunocompromised patients, treatment with immunosuppressants before, during, or after treatment with ofatumumab, vaccinations, malignancies. IA: Immune response to vaccination may be reduced due to B-cell depletion. Possible additive immunosuppressive effects when switching from other immunosuppressive or immunomodulatory therapies to Kesimpta should be considered. UW: Very common: upper respiratory tract infection, urinary tract infection, headache, injection site reactions (local), injection-related reactions (systemic). Common: oral herpes, decreased serum immunoglobulin M (IgM) levels. P: 10.4 ml pre-filled pen. Levy category: [B]. You can find more information at www.swissmedicinfo.ch. Status ofinformation: January 2021 V01. Novartis Pharma Schweiz AG, Risch; address: Suurstoffi 14, 6343 Rotkreuz, Tel. 041 763 71 11