The second day of the Gastrointestinal Cancer Conference in St. Gallen focused on pancreatic cancer. In terms of its incidence, pancreatic cancer is one of the deadliest cancers. While the prognosis has improved in recent decades, it has unfortunately improved only slightly. Complete surgical removal of the tumor remains the most important prerequisite for affected patients to survive the disease in the longer term.
Pancreatic cancer (PC) accounts for only 3.2% of all new cancer cases in Switzerland, but has a 7% share of all cancer deaths per year. In industrialized nations, PC is the fourth to fifth leading cause of cancer deaths, and the trend is rising. Presumably, lifestyle factors and the aging of society are responsible for this increase in incidence. PC is projected to be the second leading cause of cancer death in the U.S. by 2020.
Smoking causes 20% of all pancreatic cancers
Dr. Patrick Maisonneuve, European Institute of Oncology, Milano (I), spoke about the epidemiology and risk factors of PC. Various factors can increase the risk of PC (Tab. 1) . Rare hereditary and genetic factors provide for a strongly increased risk, but they are responsible for only a very small proportion of PC. Pancreatic cancer in the family history doubles the risk. The most important risk factor in the general population is smoking, which causes about 20% of all PC. Metabolic factors such as obesity, impaired glucose tolerance, and long-term diabetes also increase the risk, whereas an atopic predisposition and the use of metformin reduce the risk.
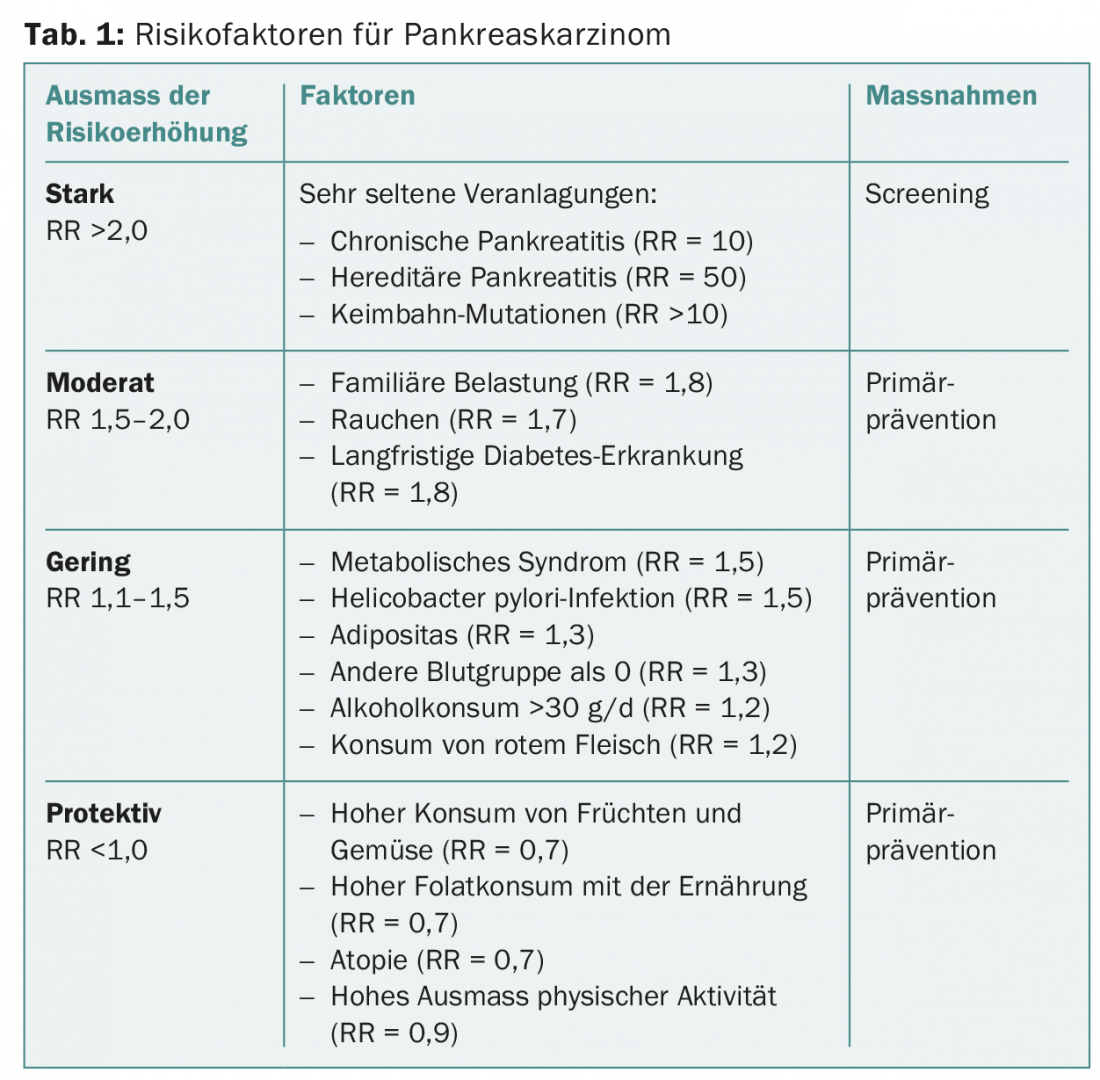
About two-thirds of the risk factors are dependent on lifestyle, which means that consistent preventive measures (not smoking, reducing alcohol consumption, balanced diet with lots of fruits and vegetables and little red meat, sufficient exercise) could reduce the incidence of PC by 30%.
Possibilities for early detection in high-risk groups
Prof. Dr. Marco Bruno, University Medical Center Rotterdam (NL), presented options for early detection of PC. Early detection measures may be important in individuals who have a significantly increased risk of disease due to a hereditary predisposition. A distinction is made between two main target groups. The larger includes individuals with at least three first-degree relatives with PC but no known genetic defect (familial pancreatic cancer, FPC) – their risk of developing PC is increased 17- to 32-fold compared with the normal population. The second group is individuals with a well-defined genetic syndrome that increases the risk for various cancers (Table 2).
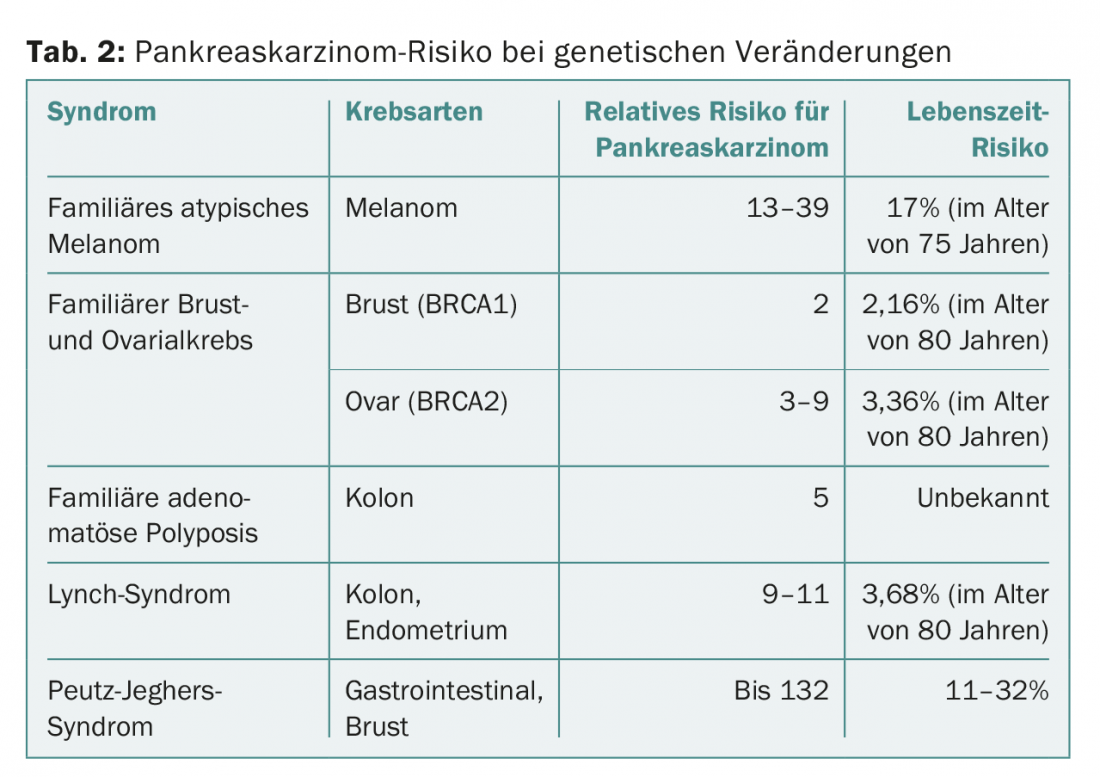
Surveillance of individuals at high risk of PC aims to prevent (too) early deaths – either by detecting the cancer at an early stage that is still curatively treatable, or by diagnosing precancerous lesions before invasive cancer develops. The (still) benign precursors of PC include intraepithelial neoplasms of the pancreas (PanIN), intrapancreatic mucinous neoplasms (IPMN), and mucinous cystadenomas. The precursors take about twelve years to develop into invasive carcinoma. This time window can be used for early detection measures, but technical procedures must also be able to detect the precursors.
Currently, (annual) endosonography and MRI examinations are the main tools used for early detection, but intensive research is being conducted on potential biomarkers that can be detected in pancreatic juice, blood, saliva or stool. Regular PC screening is recommended for individuals whose risk of PC is increased by at least a factor of 10. Yet, to date, there is no evidence that monitoring individuals at high risk for PC improves survival.
Improving surgery improves prognosis
Jens Werner, MD, University Hospital Munich (D), provided information on which factors can improve the prognosis of PC. Over the past 40 years, the prognosis has improved, but unfortunately only slightly. One reason for this is probably that many patients with “localized” PC already have micrometastases present at diagnosis. The 5-year survival rate is currently between 15 and 25%. However, it is strongly dependent on risk factors
from – these allow an accurate assessment of the forecast.
The most important factor for a possible cure is curative R0 resection of the carcinoma, including standard lymphadenectomy. Complete removal of the carcinoma is sometimes only achievable with total pancreatectomy; if the vessels are not yet infiltrated, 5-year survival is 25%. The quality of life of affected patients is good, and diabetes is usually well controlled.
However, although surgery is so important, according to a 2007 study, not all patients for whom surgery would be possible and appropriate are offered surgery [2]. Chemotherapies and targeted therapies also help improve prognosis.
In summary, the following measures are needed to improve prognosis in as many patients as possible:
- Surgery as soon as possible after diagnosis
- Radical tumor resection (R0)
- Extended resection, if necessary
- Resection of precancerous carcinoma; no “watch and wait”.
- Multimodal therapy incl. Chemotherapy and targeted therapies
How effective is neoadjuvant radiochemotherapy?
When diagnosing PC, patients can be divided into different groups:
- 15-20% have localized disease and are directly operable;
- 30-40% have locally advanced disease (some operable, some inoperable);
- 40% have metastatic disease treated with chemotherapy.
For those patients with localized disease, the question is whether neoadjuvant chemotherapy or even radiochemotherapy can improve the chance of cure. Prof. Dr. Karin Haustermans, UZ Leuven (Belgium), spoke at the congress about the option of radiochemotherapy.
The organs surrounding the pancreas (small intestine, kidneys, spinal cord, liver) are very sensitive to radiation, for this reason radiotherapy is particularly challenging. For adjuvant radiotherapy, there are some studies with negative results, but for neoadjuvant radiotherapy, two studies have shown an improvement in median survival [3,4].
Neoadjuvant therapy offers several advantages:
- Patients with rapidly progressing disease may be spared useless surgery by re-staging after radiochemotherapy.
- Micrometastases are treated early.
- The chances of subsequent R0 resection may increase.
- The vascularization of the tumor is still intact, which means that chemotherapy can penetrate better and radiation works better (oxigenation of tumor cells)
- The target volume for irradiation is smaller.
- The total treatment time is shorter.
- After surgery, the histology of the treated tissue can be assessed; the histologic response is a prognostic marker.
- No treatment delay due to poorly healing wounds.
Prof. Haustermans emphasized that it is important to continue to improve radiation techniques. One way to do this is stereotactic radiation therapy (SBRT), which requires patients to hold their breath briefly to prevent organ movement and thus “co-radiation” of healthy tissue. SBRT has the advantage that it also destroys endothelia, cell membranes and vessels, resulting in a better antitumor effect. However, as a general rule for neoadjuvant chemoradiotherapy, “The therapy must not be worse than the disease.”
Source:3rd St. Gallen-International Gastrointestinal Cancer Conference, March 10-12, 2016, St. Gallen.
Literature:
- Maisonneuve P, Lowenfels AB: Risk factors for pancreatic cancer: a summary review of meta-analytical studies. Int J Epidemiol 2015; 44(1): 186-198.
- Riall TS, Lillemoe KD: Underutilization of surgical resection in patients with localized pancreatic cancer. Ann Surg 2007; 246(2): 181-182.
- Breslin TM, et al: Neoadjuvant chemoradiotherapy for adenocarcinoma of the pancreas: treatment variables and survival duration. Ann Surg Oncol 2001; 8(2): 123-132.
- White R, et al: Significance of histological response to preoparative chemoradiotherapy for pancreatic cancer. Ann Surg Oncol 2005; 12: 214-221.
InFo ONCOLOGY & HEMATOLOGY 2016; 4(3): 25-27.