Ovarian cancer is often not detected until an advanced stage due to initial nonspecific or absent symptoms [1]. Consequently, the prognosis is rather poor, also due to the high relapse rate [2]. However, the approval of PARP inhibitors has significantly improved the situation for patients, as maintenance therapy after platinum-based chemotherapy can prolong disease- and progression-free survival without significantly affecting health-related quality of life [2, 3].
Every year, approximately 600 women in Switzerland are diagnosed with ovarian cancer [1]. Approximately 75% of patients relapse within the first 18-28 months after completion of initial therapy and the 5-year survival rate is only 30-50% [2]. Treatment options for recurrent ovarian cancer have been significantly expanded with the introduction of PARP inhibitors. Niraparib provides a maintenance therapy for patients with platinum-sensitive relapsed ovarian cancer that leads to a significant prolongation of progression-free survival independent of BRCA mutation status [4]. In this context, the individual starting dosage approved in Switzerland allows for improved tolerability while maintaining efficacy [2, 4, 5].
Niraparib works regardless of BRCA mutation status
Niraparib was the first PARPi to demonstrate significant improvement in progression-free survival (PFS) in patients with relapsed platinum-sensitive ovarian cancer regardless of BRCA mutation status in a randomized, placebo-controlled phase III trial (ENGOT-OV16/NOVA) [6]. For example, PFS in patients with BRCA germline mutation (gBRCA) was prolonged by 15.5 months (niraparib: 21.0 months; placebo: 5.5 months; HR 0.27; P<0.001) and in patients without BRCA germline mutation (non-gBRCA) by 5.4 months (niraparib: 9.3 months; placebo: 3.9 months; HR 0.45; P<0.001) [6].
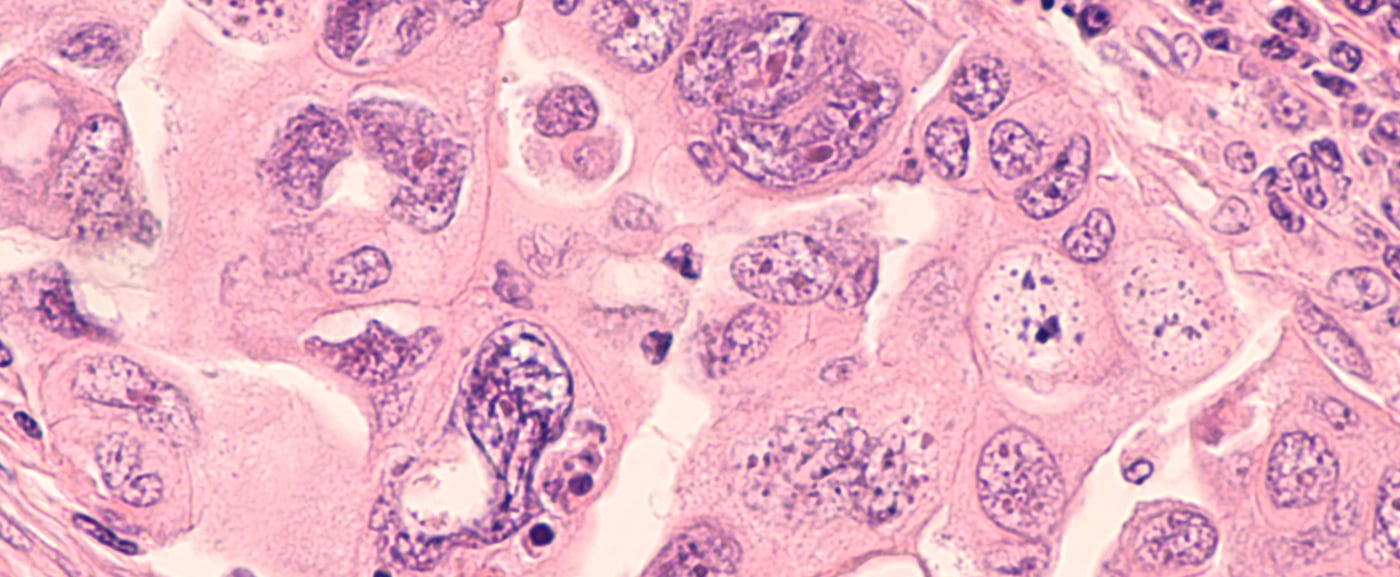
Based on these study results, niraparib has been approved in Switzerland since October 2018 as maintenance therapy in patients with platinum-sensitive, recurrent, primary epithelial serous high-grade ovarian, tubal, or peritoneal carcinoma after complete or partial response to platinum-based chemotherapy [4].
The other PARPi approved in Switzerland, olaparib, also showed positive results in terms of PFS in the randomized, placebo-controlled phase III SOLO2/ENGOT-Ov21 trial, but only in patients with gBRCA [7]. For non-gBRCA, data are available from the phase II study 19 and the single-arm phase IIIb OPINION study [8, 9].
Reduced starting dose enables same efficacy with fewer side effects
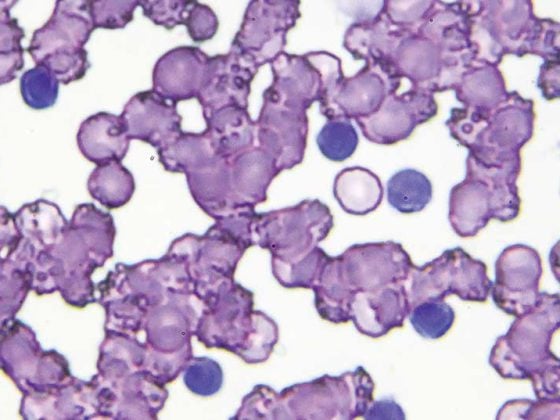
Good tolerability and preservation of health-related quality of life, in addition to efficacy, are central concerns of maintenance therapies [10]. In general, the side effects of niraparib therapy were well managed [6]. The most common serious adverse events (grade 3/4) with niraparib included thrombocytopenia (33.8%), anemia (25.3%), and neutropenia (19.6%) and occurred mostly in the first three cycles of treatment [6]. In contrast, after individual dose adjustments, thrombocytopenia, neutropenia, and fatigue (grade 3/4) were less frequent in later cycles [6]. Thrombocytopenias were mostly transient and platelet counts stabilized from the third cycle of treatment [6].
A retrospective analysis of ENGOT-OV16/NOVA data examined the associations between niraparib dose and the occurrence of treatment-associated adverse events (TEAEs) [5]. This showed that dose reductions were made in 68.9% of patients due to TEAEs, mostly within the first three months of treatment. The most common of these was a reduction in the dose of niraparib from 300 mg to 200 mg, which increased the rate of 3rd/4th TEAEs. degree decreased significantly. A lower rate of anemia (grade 3/4) was observed only at a niraparib dose of 100 mg [5]. In addition, a low platelet count (<150000/µl) and a body weight <77 kg were identified as risk factors for the development of grade 3/4 thrombocytopenia within the first 30 days on niraparib [5]. No difference in efficacy was observed in patients receiving a reduced dose of niraparib (200 mg or 100 mg) compared with the higher dose of 300 mg. To exclude a bias against the 300 mg dose, PFS data were only considered from the fourth month of treatment onwards, as most patients had reached a stable dose by then [5].
Based on these results, niraparib was approved in Switzerland with a recommended starting dose of 200 mg [4]. Only in patients with a body weight
≥ 77 kg and a normal platelet count (≥150,000/µl), niraparib therapy continues to be initiated at a dose of 300 mg [4]. Niraparib only needs to be taken once daily, which simplifies therapy and thus supports adherence [4].
Good compatibility in real-world settings
Treatment with 200 mg niraparib is also associated with improved tolerability under real-world conditions [2]. This is according to a real-world study that evaluated anonymized dossiers from 153 patients who received niraparib at a starting dose of 200 mg [2]. Patients were median 59 years old and weighed median 70 kg. The median time between completion of platinum-based chemotherapy and initiation of maintenance therapy with 200 mg niraparib was 33 days [2]. In clinical trials, nausea, thrombocytopenia, and fatigue were the most common adverse events with niraparib. In the real-world setting, these adverse events occurred in 37% of patients within the first three months, but showed a significantly reduced incidence with 200 mg niraparib compared with the starting dose of 300 mg niraparib in the ENGOT-OV16/NOVA trial (Figure 1). A reduction in niraparib dose from 200 mg to 100 mg occurred in 11% of patients. Interruption of therapy due to side effects was necessary in 4% of patients and in only 2% did treatment have to be discontinued within the first three months [2].

Figure 1: Incidence of the three most common grade 3/4 adverse events in patients in the real-world clinical setting (niraparib starting dose 200 mg) compared with patients in the ENGOT-OV16/NOVA trial (niraparib starting dose 300 mg), modified from [2].
Conclusion
Switzerland is the first country to approve niraparib with a reduced starting dose of 200 mg [4]. This dose reduction can significantly reduce the rate of side effects compared with 300 mg dosing without compromising the efficacy of maintenance therapy [5, 6]. As shown in a real-world study, the reduced dose is also associated with improved tolerability in clinical practice [2]. Individual dose adjustments allow optimal management of side effects, thus helping to preserve patients’ quality of life during maintenance therapy [2].
Swiss Oncology in Motion
Swiss Oncology in Motion is an accredited continuous online education for medical oncologists, hematologists and oncology specialists, available free of charge at medizinonline.ch. In one-hour video modules, relevant oncology topics are conveyed through three 15-minute lectures by specialists each, followed by a question-and-answer session. The modules are moderated by Prof. em. Richard Herrmann, MD. In the first part of the module on ovarian cancer, Dr. med. Anita Wolfer (former senior physician at CHUV) will guide you through relevant figures and scientific facts about the disease. In the second part, Prof. Dr. Andreas Günthert (Head of gyn-zentrum Luzern) will talk about the care situation and treatment in Switzerland. A new update is now also available in which PD Marcus Vetter, MD (Chief Physician, Medical Oncology, University Hospital Basel), presents and discusses the current options in maintenance therapy. This link will take you directly to the video. |
The content of this article is the responsibility of and financed by GlaxoSmithKline AG, Talstrasse 3 – 5, 3053 Münchenbuchsee. Trademarks are property of their respective owners. ©2020 GSK group of companies or its licensor.
Zejula is indicated for the maintenance treatment of adult patients with platinum-sensitive, recurrent, primary epithelial, serous high-grade (highly dedifferentiated) ovarian, tubal, or peritoneal carcinoma. The patient must have had a complete or partial response to platinum-based chemotherapy [4].
Zejula short subject information
Dr. sc. nat. Jenny Thom
PM-CH-NRP-ADVR-210008-01/2021
Literature