According to the WHO definition, more than 5 drugs per day is considered polypharmacotherapy and is especially common in elderly patients. In the over-70 age group, up to half of all patients meet this criterion. It is important to consider possible interaction effects.
This is a problem, of course, because every doctor can follow the demographic trend for himself in his practice or on the ward: The over-80s are the fastest-growing population group. The typical patient in practice and hospital is already the elderly with more than three diagnoses. Very often, pain is a central symptom in this group of patients. The most common medical measure is the prescription of a pharmaceutical. And there are often problems with adherence and interactions. Non-adherence is estimated to be as high as 50%, depending on the clinical picture. There are many reasons for this:
- Only 7 out of 100 Germans have a very good level of health literacy
- More than 50% have difficulty in dealing with health information
- Over 50% find it difficult to assess advantages and disadvantages of treatment options
- Over 20% find it difficult to follow instructions for taking medicines
- Depending on education level, migration background and age, 30-60% find it difficult to understand the package insert of medications
Prof. Dr. Dr. Gerd Geißlinger, Institute for Clinical Pharmacology, University Hospital Frankfurt, who presented these figures, pointed out that there have been studies in Germany according to which an educational level between Mittlerer Reife and Abitur is required to understand a German package insert. “In Switzerland, people have obviously thought about this,” says the expert, “because there these figures look much better, so the supplements are apparently written in a way that is easier to understand.”
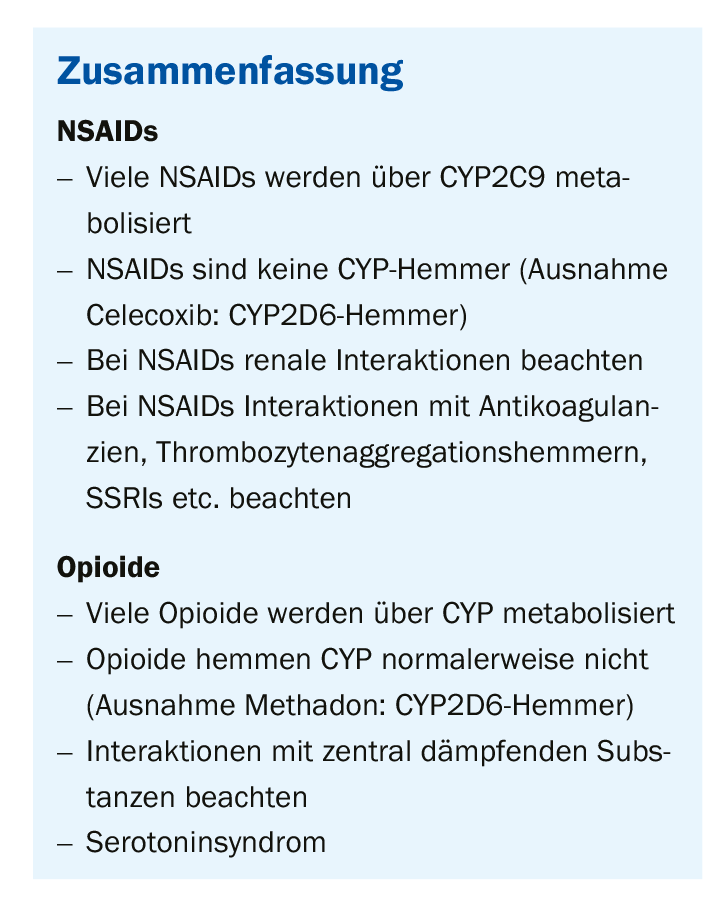
Caution in combinations with NSAID
Polypharmacy interactions are very commonly associated with analgesics, especially non-steroidal anti-inflammatory drugs (NSAID). For example, Prof. Geisslinger strongly cautioned against combining an NSAID with anticoagulants because they are platelet aggregation inhibitors and the risk of bleeding is increased. The same risk exists when combined with a selective serotonin reuptake inhibitor (SSRI). On the pharmacodynamic side, however, there are interactions with opioids and centrally depressant substances; for example, combination with benzodiazepine, barbiturate, or pancuronium results in an increase in effect. “And, of course, you shouldn’t combine a WHO Level 3 opioid with a Level 2,” the pharmacologist explained. He highlighted one interaction in particular because, although rare, it can have dramatic consequences if it occurs: serotonin syndrome.
This syndrome is triggered by a rise in serotonin in the CNS, often caused by drug interaction. This can occur if substances that can increase serotonin concentrations in the synaptic cleft (such as tramadol) and SSRIs are taken at the same time. Symptoms include tachycardia, sweating, RR increase, diarrhea, and CNS agitation, as well as agitation, hallucinations, hypomania, dyskinesia, and suicidality. Neuromuscularly, tremor, reflex increase, and myoclonia may occur.
Tramadol as a trigger
Tramadol is a racemate, there is a plus and a minus enantiomer. The (-)-tramadol preferentially inhibits the uptake of norepinephrine, while the (+)-tramadol inhibits the uptake of serotonin. The consequence of this is that when combined with an SSRI, there are increased serotonin concentrations and possibly said serotonin syndrome.
You can’t always tell from the name that you have to pay attention as a doctor: It may still be relatively visible with SSRIs, but substances such as lithium can also cause the syndrome, because lithium can increase serotonin receptor sensitivity. So do antidepressants, triptans, ergot alkaloids or St. John’s wort extract, and also some drugs.
For almost 75% of all substances, metabolization occurs via the liver and the so-called cytochrome (CYP)-P450 isoenzyme system. Within this system, various substances are metabolized by different P450 isozymes. For example, theophylline functions via CYP1A2, whereas phenprocoumon and tamoxifen function via CYP3A4 (Table 1).
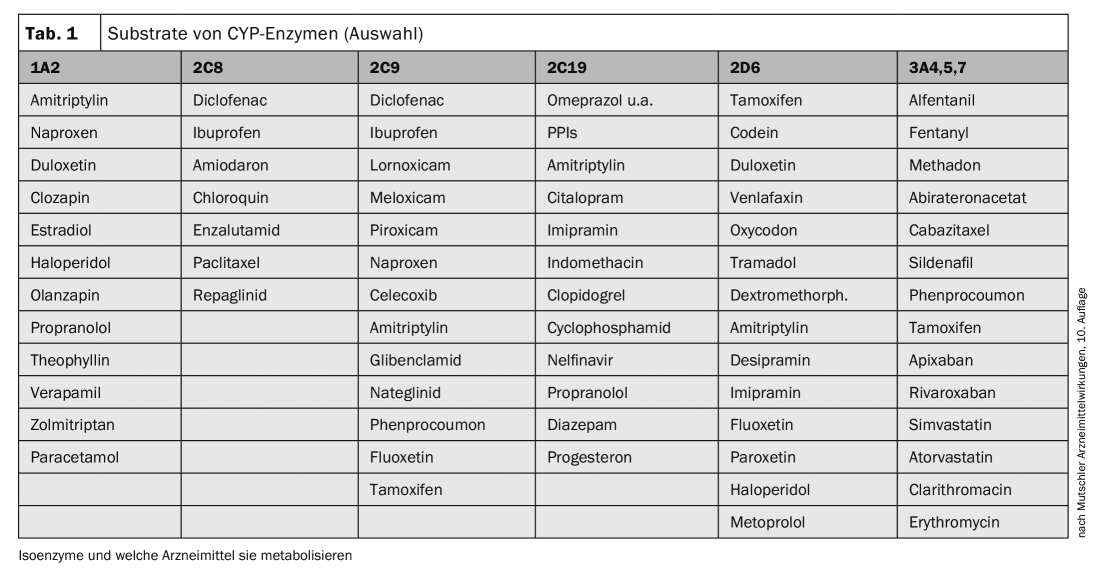
Where there are substrates, there are also inhibitors: ciprofloxacin, for example, is a strong CYP1A2 inhibitor. This means that if ciprofloxacin were combined with theophylline, there would be major problems, especially since the therapeutic range of theophylline is relatively small. CYP3A4, on the other hand, can be inhibited by a great many substances, for example grapefruit juice – hence the common recommendation to patients to take their medication with water and never with grapefruit juice.
Prof. Geißlinger recommended familiarizing oneself with the enzyme tables and taking a look at them from time to time, as in this way many drug interactions can be anticipated and thus avoided.
Source: Industry Symposium “Modern Management of Chronic Pain Patients” at the 125th Annual Meeting. Congress of the German Society for Internal Medicine (DGIM), Organizer: Grünenthal
FAMILY PRACTICE 2019, 14(6): 26-27