Complex perianal fistulas in Crohn’s disease are associated with significant distress for those affected. Until now, there has been a lack of long-term effective therapies, especially for those who do not respond to anti-TNF-α drugs.
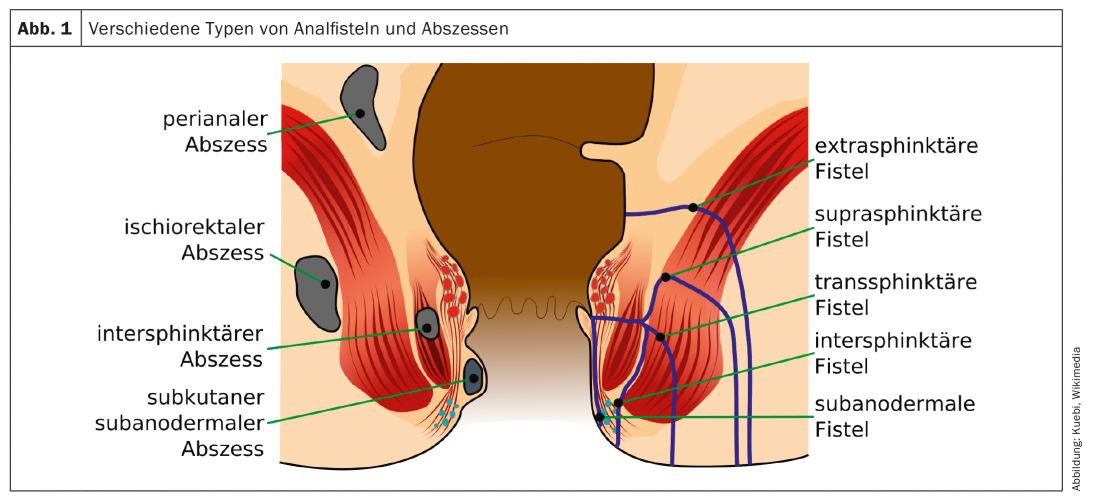
(red) Crohn’s disease patients are frequently affected by perianal fistulas. Perianal fistulas are abnormal passages between the lower parts of the bowel and the skin near the anus. Fistulas can be differentiated into simple or complex fistulas. Approximately 80% of perianal fistulas in MC are considered complex; the fistulas involve the upper portion of the sphincter complex, have multiple external openings, are associated with pain or fluctuation suggestive of a perianal abscess, and/or are associated with a rectovaginal fistula or anorectal stricture (Fig. 1). Complex perianal fistulas result in a high burden of disease and significantly affect health-related quality of life. The fistulas may cause pain during bowel movements, sitting or walking. In addition, uncontrolled fluid such as blood, pus or stool can leak through the fistula tracts. They are often difficult to treat and respond poorly to drug therapies.
Treatment approaches include combinations of drug and surgical options with the goal of achieving remission, treating and preventing further septic complications, releasing fistula drainage, and improving patient quality of life. In adults with nonactive or mild Crohn’s disease, perianal fistulas are treated with medications, including antibiotics, immunosuppressants, and biologic therapy. Currently, TNF-α agents are recommended as first-line therapy for complex perianal fistulas in patients with MC. Relapses often occur after medical treatment is discontinued, and it is generally believed that only one-third of patients achieve remission, which is often defined as closure of external orifices and lack of drainage. If the fistula and associated abscesses do not heal, surgery is required. Under general anesthesia, the abscesses are then drained and a suture is passed through the fistula. This keeps the fistula open so that it can drain. These setons are usually not curative and remission rates are low. In the worst case, the MC patient cannot avoid proctectomy (permanent removal of a portion of the bowel to bypass the perianal fistula). There is now hope for a certain patient population.
New treatment option
Since the beginning of this year, Alofisel® (darvadstrocel), an allogeneic stem cell therapy for patients with Crohn’s disease, has been approved in Switzerland. It is indicated in adults with non-active or low-activity Crohn’s disease with complex perianal fistulas, provided the fistulas have responded inadequately to at least one conventional or biologic therapy. The treatment is based on mesenchymal stem cells, which can alleviate inflammatory processes. The cells do not have to survive long in the patient’s body to do this; they emit anti-inflammatory messenger substances for a limited time.
For more information on stem cell therapy, email alofisel_CH@takeda.com.
Further reading:
- Panés J, Rimola J: Nat Rev Gastroenterol Hepatol 2017; 14(11): 652-664.
- Baumgart DC, Sandborn WJ: Lancet 2012; 380(9853): 1590-1605.
- https://stemcells.nih.gov/info/basics/4.htm.
- Panés J, et al: Lancet 2016; 388(10051): 1281-1290.
HAUSARZT PRAXIS 2019; 14(3): 30











