The main symptoms of knee bursitis are stabbing knee pain, pressure pain or extension deficits of the knee joint. After radiographic examination and sonographic confirmation of the diagnosis, magnetic resonance imaging can be used to determine the exact extent and activity of the bursitis by means of contrast-enhanced sequences. Conservative therapy often leads to relief of symptoms, but in the case of chronic bursitis, surgical intervention is usually the only option.
In the preceding articles, various degenerative changes of internal structures of the knee joint have already been discussed, without any detailed discussion of bursitis so far. In principle, there are other peripatellar changes that are not very different clinically and symptomatically. In the following articles, these diseases will be discussed in terms of differential diagnosis.
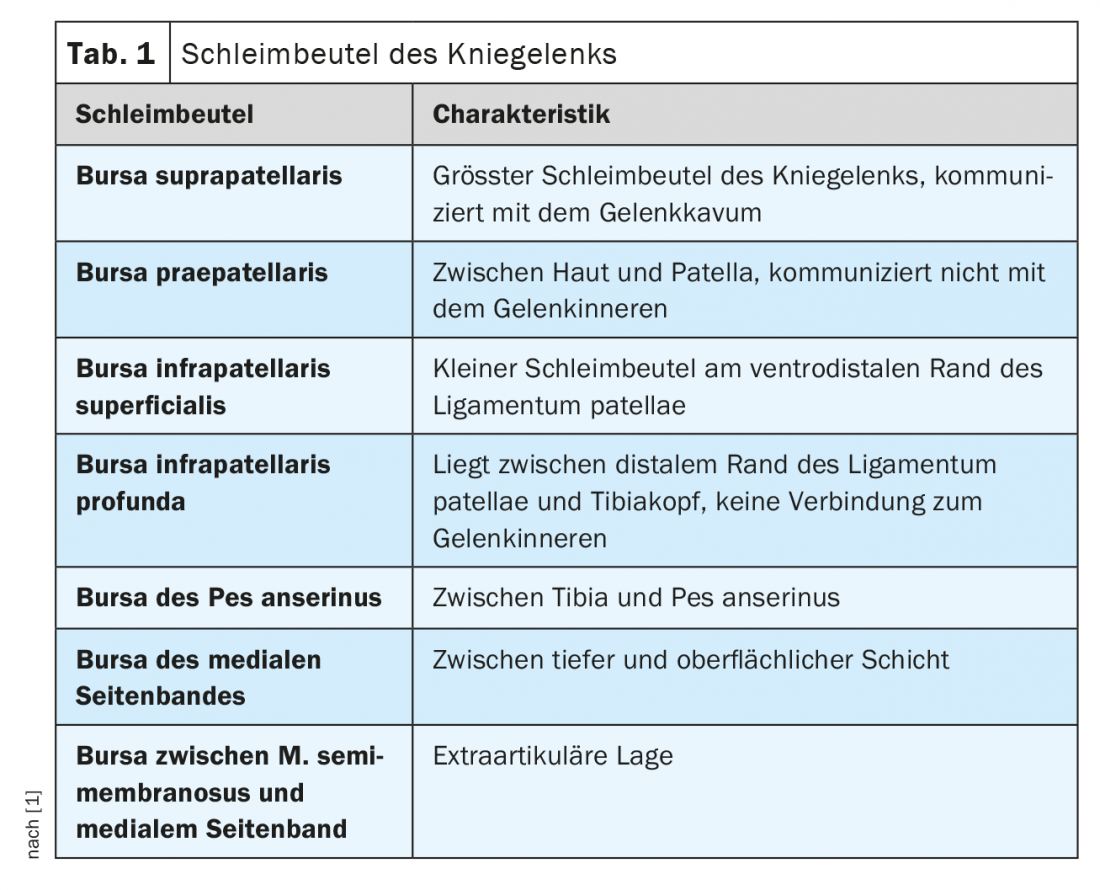
The knee joint is surrounded by several bursae (Tab. 1), which can become symptomatic in the context of inflammatory degenerative or traumatic influences. These include acute or chronic overload situations, traumas that have taken place, or postoperative sequelae. Bursitis may also occur in the context of generalized inflammatory diseases, e.g. rheumatic diseases. Inflammatory alteration of the bursa results locally in the classic signs of inflammation, which may well cause impressive clinical symptoms [4,5]. Various risk factors can be determined by anamnesis (overview 1). Preventive measures are therefore advisable in the case of corresponding occupational or sporting exposure (padded knee pads, bandages).
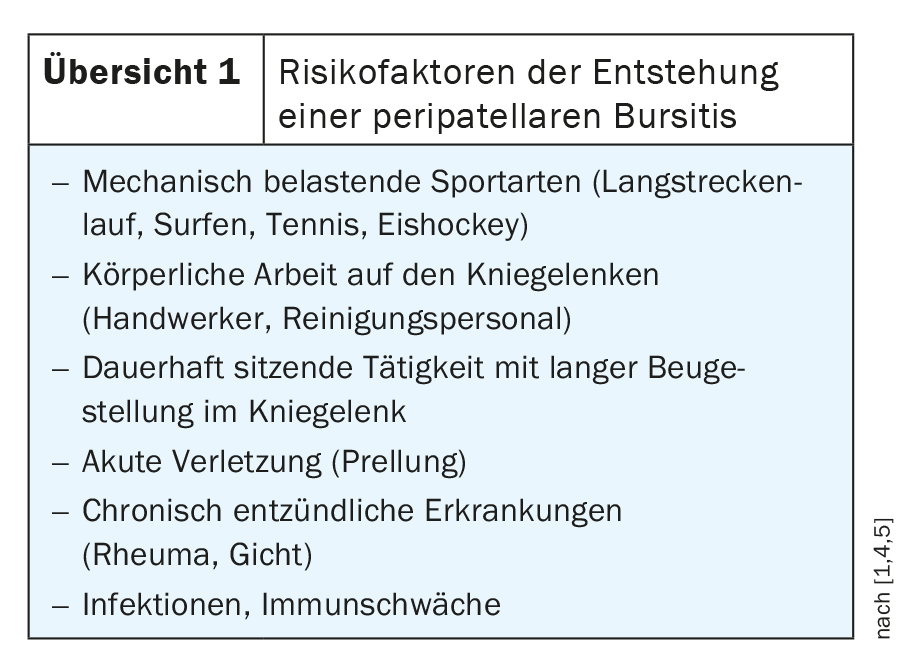
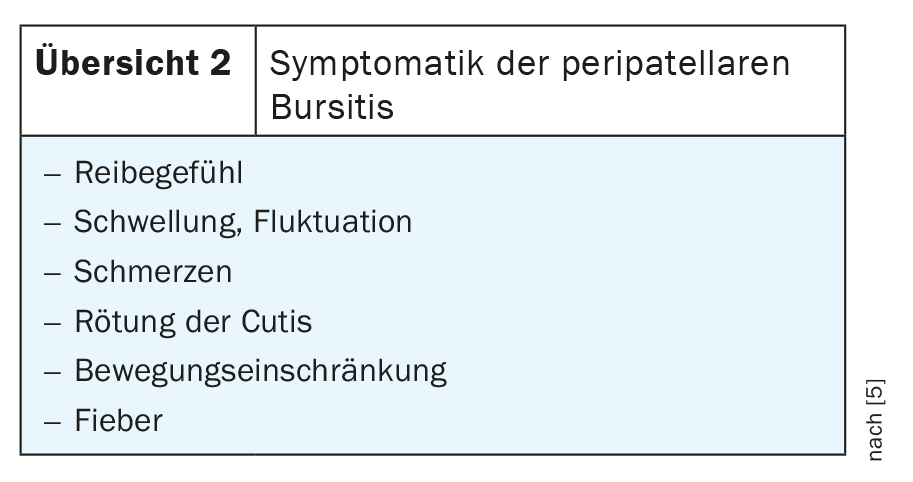
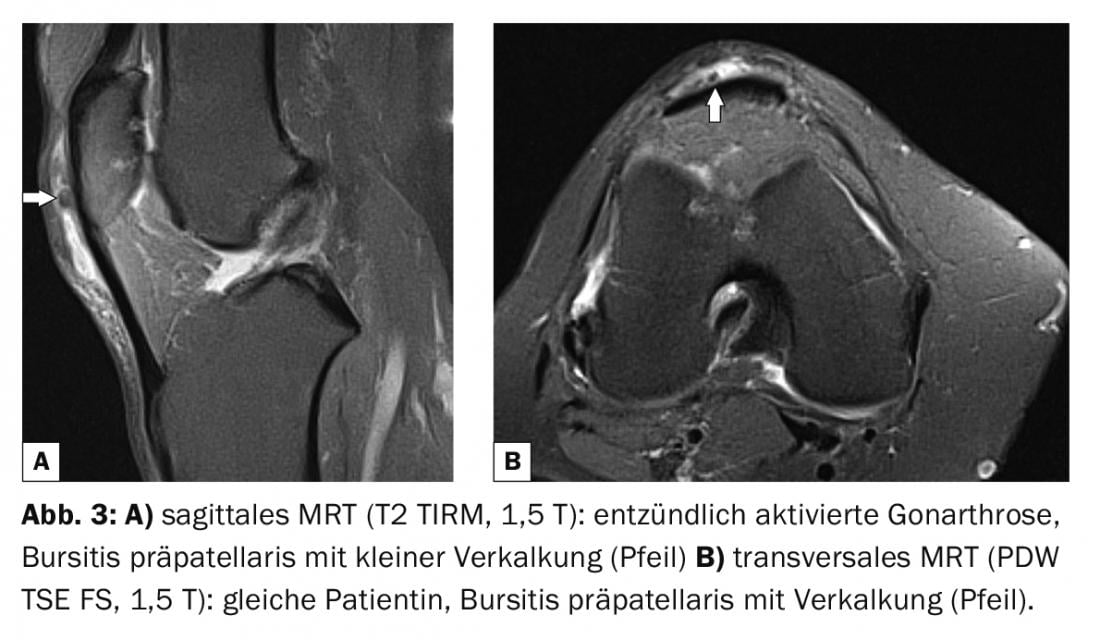
The symptoms of bursitis can be varied (overview 2) . Chronic bursitis is characterized by a course lasting several weeks with constant or chronic recurrent symptoms, which may then also lead to surgical treatment. Chronic progression may result in local tissue calcification or ossification in soft tissue [2,3]. If no lasting improvement can be achieved by conservative therapeutic measures, surgery is the treatment of choice. In this regard, minimally invasive procedures are more likely to result in normal postoperative exercise capacity [4].
Radiographs in lateral projection may show local soft tissue swelling and compaction in the otherwise locally poorly developed subcutaneous fat tissue in cases of pronounced prepatellar bursitis, leading to a tentative diagnosis. Sonographically, the bursa can be shown to be enlarged and fluid-filled in the inflammatory stage, and often with thickening of the wall in the chronic course [5].
Computed tomographic examinations provide more accurate information about the extent of bursitis than radiography and can also better differentiate fluid portions, but they lag behind MRI in information content in soft tissue contrast. However, the calcifications and ossifications are better delineated on CT.
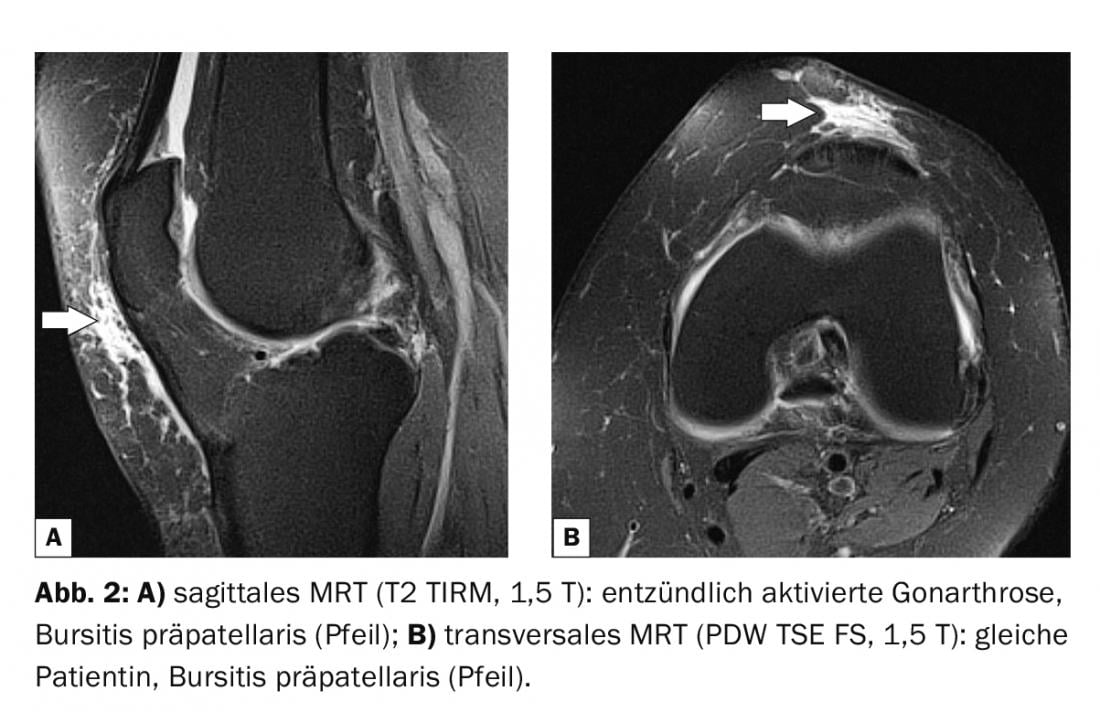
Magnetic resonance imaging reliably identifies prepatellar bursitis, and contrast sequences also show the activity and extent of the inflammatory reaction. Purulent enamels are differentiable. Of course, the method also provides comprehensive information about the internal structures of the joint.
Case studies
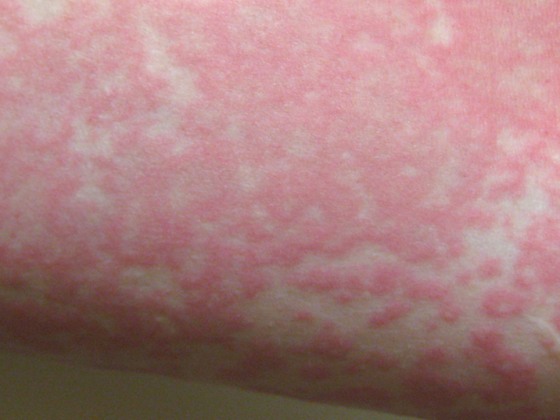
In case report 1 , the lateral radiograph of the right knee (Fig. 1) shows significant soft tissue compaction and swelling in a 64-year-old patient with the clinical picture of activated gonarthrosis and prepatellar soft tissue swelling with localized hyperthermia, consistent with florid prepatellar bursitis. Anamnestically, no adequate trauma was present.

Case report 2 demonstrates bursitis prepatellaris on MRI (Fig. 2A and B) with liqour-equivalent signal in a 58-year-old female patient with inflammatory activated gonarthrosis.
Extensive prepatellar bursitis with an apparently chronic course is documented in case report 3 in a 55-year-old cleaning woman. Hypointense structures within the bursa were delineable, compatible with small calcifications (Fig. 3A and B).
Take-Home Messages
- The suspected diagnosis of acute prepatellar bursitis can be made after taking a medical history (occupational, athletic disposition) and clinical examination.
- Bursitis can be diagnosed sonographically, and if it is extensive enough, it can at least be suspected radiographically.
- Magnetic resonance imaging, supplemented by contrast-enhanced sequences, can determine the exact extent and activity of bursitis and provide additional information about the internal structures of the knee joint.
- If conservative treatment is frustrating, surgical therapy is an option.
Literature:
- Breitenseher M: The MR-Trainer Lower Extremity. Georg Thieme Verlag: Stuttgart, New York 2002: 210.
- Erler M: Ossifying bursitis praepatellaris of the knee joint. Z Orthop Accident. 2009; 147(6): 743-746.
- Hansen TB, Pless S: Calcifying pre-patellar bursitis. Presentation of a case involving both knees. Ugeskr Laeger 1994; 156(25): 3780.
- Steinacker T, Verdonck AJ: Endoscopic therapy of pre-patellar bursitis. Sports Injuries Sports Injury 1998; 12(4): 162-164.
- endoprostheticsguide: Bursitis of the knee: www.endoprosthetics-guide.com/knie/schleimbeutelentzuendung-knie (last accessed 11/18/2021)
HAUSARZT PRAXIS 2021; 16(12): 38-39