Sub-syndromal and generalized anxiety disorders are common disorders. If left untreated, anxiety disorders can be associated with significant psychosocial consequences. Therefore, effective and well-tolerated therapeutic options are needed. A new meta-analysis confirms the evidence-based treatment effects of a lavender oil-based phytotherapeutic preparation also on somatic components of anxiety.
According to epidemiological data, the prevalence of generalized anxiety disorder (GAS) in primary care patients is 4.1-6.%–6,0% in men and 3%–7,1% 7-7%–7,1% in women [1]. If the diagnostic criteria of a GAS are not fully met, the disorder is referred to as subsyndromal anxiety disorder. Its prevalence is 2.3% in the general population [2]. In addition to the leading symptom of excessive anxiety and worry for at least 6 months, secondary criteria for GAS include muscle tension, fatigability, sleep disturbances, and other vegetative symptoms [3,4]. If left untreated, anxiety disorders can be associated with significant impairments in coping with everyday life as well as a reduced quality of life. Moreover, the economic consequences associated with incapacity for work are considerable [5,6].
Silexan® as a proven treatment option for anxiety reduction
Lavender oil extract Silexan®, derived from the medicinal lavender Lavandula angustifolia, has shown anxiolytic effects in GAS and other anxiety disorders, and beneficial effects on sleep and fatigue have also been demonstrated in subsyndromal anxiety disorder [7–11]. The mechanism of action of Silexan® involves presynaptic inhibition of voltage-dependent calcium influx (VOCC) in the central nervous system as well as modulation of serotonergic neurotransmitter circuits (Overview 1).

New meta-analysis confirms: Silexan® also reduces somatic symptoms
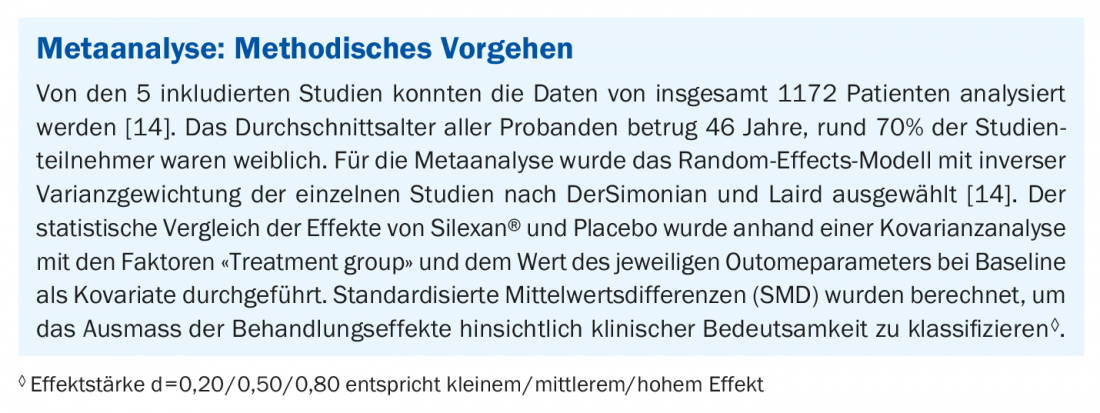
To evaluate specific therapeutic effects of Silexan® on somatic symptoms in GAS and subsyndromal anxiety disorder, a meta-analysis was conducted [14]. Included five randomized, placebo-controlled trials in patients with GAS (2 trials) and in patients with subsyndromal anxiety disorder (3 trials) [7–10,13] (box ). Silexan® (80 mg /day) proved superior to placebo at week 10 after baseline in terms of mean change in the HAMA ‘Somatic Anxiety’ subscore (HAMA items 7-13). The Standardized Mean Difference (SMD) was -0.31 [95% Kl: -0.52 to -0.10, p=0.004] [14,15,18]. The treatment effects of Silexan® on somatic components of anxiety were independent of gender and age. Statistically significant differences were also shown for the individual HAMA items somatic, muscular, cardiovascular, respiratory, and urogenital symptoms. Also with regard to the SF-36 subscore ‘Physical health’, which is evaluated as an indicator for health-related quality of life and was used in all included studies except Kasper et al. 2015 [9], clinically significant effects of Silexan® were measurable.
Literature:
- Munk-Jorgensen P, et al: Psychiatric Services (Washington, D. C.) 2006; 57(12): 1738-1744.
- Gilmour H: Health Reports 2016; 27(11): 13- 21.
- Burstein M, et al: Psychological Medicine 2014; 44(11): 2351-2362.
- APA: Diagnostic And Statistical Manual Of Mental Disorders 2013, Fifth Edition. Washington D.C: American Psychiatric Publishing.
- Greenberg, PE, et al: Journal of Clinical Psychiatry 1999; 60(7): 427-435.
- Hoffman DL, et al: Depressed Anxiety 2008; 25(1): 72-90.
- Kasper S, et al: International Clinical Psychopharmacology 2010; 25(5): 277- 287.
- Kasper S,et al: European Neuropsychopharmacology 2016; 26(2): 331-340.
- Kasper S, Anghelescu I, Dienel A: European Neuropsychopharmacology 2015; 25(11): 1960-1967.
- Möller H-J, et al: European Archives of Psychiatry and Clinical Neuroscience 2019; 269(2): 183-193.
- Kasper S, et al: International Clinical Psychopharmacology 2010; 25(5): 277-287.
- Müller WE, et al: Psychopharmacotherapy 2015; 22: 3-14.
- Kasper S, et al: International Clinical Psychopharmacology 2017; 32(4): 195-204R, et al: Brain and Behaviour 2021 ; 11(4): e01997.
- von Känel R, et al: Therapeutic effects of Silexan on somatic symptoms and physical health in patients with anxiety disorders: A meta-analysis. Brain and Behaviour 2021 ; 11(4) : e01997.
- Hamilton M: British Journal of Medical Psychology 1959; 32(1): 50-55.
- Baldinger P, et al: Int J Neuropsychopharmacol 2014; 18(4). doi: 10.1093/ijnp/pyu063.
- Seifritz E, et al: International Journal of Neuropsychopharmacology 2020, DOI: 10.1093.
- Cohen J: Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates: 1988,2nd ed., pp. 82
HAUSARZT PRAXIS 2021; 16(5): 29
InFo NEUROLOGY & PSYCHIATRY 2021; 19(3): 42.











