Per se, although cardiac risk increases briefly during any exercise, even for the well-trained athlete, and may remain elevated for several hours after exercise, the positive health or prognostic effect of regular exercise reduces the overall cardiovascular risk for the athlete and thus the risk of death from cardiac causes. Although the clear majority of deaths in sports are cardiovascular in origin, approximately 80-90% of these athletes would theoretically be detectable by adequate screening. The potential causes of sudden cardiac death are significantly influenced by the age of the athlete and determine the screening approach. The ECG is the crucial screening tool, at least in younger athletes. The fact that so-called amateur athletes are massively under-screened, even though they engage in competitive sports and are therefore at significant risk for sudden cardiac death, must be urgently addressed.
The health benefits of regular physical training are diverse and impressive: for example, various studies showed strong evidence for prolonged overall survival with continued independence and, at the same time, a reduction in falls in old age [1, 2]. Furthermore, a significant reduction of cardiovascular and cerebrovascular events can be achieved, not least by positively influencing classic cardiovascular risk factors (type 2 diabetes, arterial hypertension, serum lipids, body weight, abdominal circumference) [1–5]. And, of course, this directly counteracts sedentariness, a risk factor that is sometimes neglected even in medical consultation, but which can be absolutely equated with the traditional risk factors [1, 5, 6]. Even the prevention of various malignancies can be positively influenced by regular training. This is especially true for colon, breast, and pancreatic cancer, with somewhat less evidence for bronchus and endometrial carcinoma [4].
Particularly in the spectrum of cardiovascular diseases, regular physical training has definitely established itself in recent years as a fixed and indispensable part of therapy, both in primary and secondary prophylaxis. The “HF-ACTION” study published about four years ago should be mentioned here only as an example, since it particularly emphasized that even patients with advanced heart failure can benefit from adapted physical training, regardless of age and gender [7].
Sports stress – a danger?
As early as 1994, Haskell et al. found that health benefits increase with increasing levels of exercise, with previously sedentary patients in particular achieving excellent health gains [8]. In contrast, Paffenbarger et al. already found in the 1970s that the frequency of sudden fatal myocardial infarctions increased above a certain level of exercise [9]. This ambivalence still leads to uncertainty today, both among athletes and physicians.
In fact – exercise is considered a “trigger” for sudden cardiac death, especially when there is underlying cardiovascular disease [10–16]. But is the “paradox of sport” that many experts invoke in this context actually correct? At least to a certain extent, this concept can certainly be called into question: Per se, the cardiac risk increases briefly during every sporting activity, even for the well-trained athlete, and can remain elevated for several hours after the sporting activity. [17], but the positive health or prognostic effect of regular physical training reduces overall cardiovascular risk for the athlete and thus the risk of dying from cardiac-related death [1, 2, 8]. However, adequate preparation is absolutely crucial, i.e. a slow and targeted training build-up and an adapted extent of the load, according to the cardiac risk (or known pre-existing conditions). However, in non-trained, sedentary individuals undergoing sudden physical exertion, the risk of sudden sports-associated cardiac death may acutely increase more than 100-fold [18]. This situation, which is by no means “paradoxical”, does not occur so rarely in reality: marathons, for example, are nowadays regarded as “lifestyle events”, which are tackled without any major preparation. This is reflected in the steadily increasing average times in public marathon competitions in recent years [19].
Mainly amateur athletes are under-supported
Although the clear majority of deaths in sport are cardiovascular in origin, approximately 80-90% of these athletes would theoretically be detectable by adequate screening [20–22].
Overall, these events are fortunately rare in young athletes (approximately 3 deaths per 100 000 young competitive athletes per year) [15, 16, 20-24]. However, depending on the study method and especially on the studied collective, large discrepancies appear regarding the prevalence of sudden cardiac death in sports: On the one hand, a large American study showed that sudden cardiac death occurs less frequently than expected in marathon runners [25]. On the other hand, surveys of American soldiers also showed a much higher incidence than today’s established figures would have predicted [26]. The truth lies, as so often, somewhere in between and, as mentioned above, the decisive factor is the population under study. For example, the risk of sudden cardiac death in sports is increased in older athletes, in men, and in black athletes of African descent [11–26]. Impressively, Harmon et al. calculated. a 1 in 3000 risk of sudden cardiac death for a black college basketball player at a “Division I” college [24].
The fact that, according to the definition of most guidelines, primarily “competitive” athletes are at risk and thus should primarily be screened has two fatal consequences: The so-called amateur athletes, who, however, also engage in competitive sports, such as a professional athlete, and are subject to a corresponding risk, are massively under-screened. This in turn leads to a significant underestimation of the frequency of fatal events in sports. These are usually the focus of public attention (and statisticians) only when they involve prominent or professional athletes [27, 28]. The results of a survey of more than 1000 competitive Swiss amateur athletes speak for themselves: only 9% of these athletes have ever undergone a sports cardiology examination [29]. A distinction between competitive and non-competitive athletes therefore makes little sense and can theoretically have fatal consequences.
Causes of sudden cardiac arrest are age-dependent
Ultimately, the question of the causes of sudden cardiac arrest or even cardiac death is of critical importance, as this will determine the optimal screening strategy. It is very helpful in this context to distinguish younger from older athletes. Whereas younger athletes have underlying congenital heart disease (e.g., cardiomyopathies, coronary anomalies, an excitation conduction disorder, or connective tissue weakness)(Fig. 1), in older athletes, coronary artery disease (CAD) or myocardial infarction is responsible for sudden cardiac death in sports in more than 80% of cases [11-16, 21, 23-28].

Detection of clinically mostly asymptomatic CHD in the “older” athlete is incomparably more difficult than the search for congenital disease in “younger” athletes. This complex area will deliberately not be discussed further in this framework and I refer to the relevant literature [27, 28].
In this context, the classic age limit (30-35 years) for differentiation has rightly been questioned in recent years. Several tragic deaths of athletes between 25 and 30 years of age could be autopsy-assessed as myocardial infarction in CHD; impressive in this context are the results of a survey in King County (WA, USA), which examined the causes of death in different age segments [30]. In the 25- to 30-year-old group, 43% died of myocardial infarction secondary to relevant CHD [30].
Proper prevention through targeted screening
Although the “age cut-off” today is probably lower than previously thought, basic cardiac screening for young athletes is clearly defined and, when performed correctly, proves to be extremely sensitive and specific in detecting underlying cardiovascular disease [21, 22]. Athletes with hypertrophic cardiomyopathy, the most common underlying disease in young athletes, can be detected by ECG in over 90% [20, 21, 31]. Screening also registers a similar sensitivity for ARVC [32], and in primary conduction disorders, which account for up to 10% of deaths in young athletes, the resting ECG is the diagnostic (basic) tool of choice anyway [22, 33-35].
However, there are also weaknesses of the concept: for example, coronary abnormalities, which play a significant role at least in North American recordings, are virtually never detectable by ECG changes, and warning symptoms also rarely occur [14, 23, 36].
Commotio cordis affects completely healthy hearts and can result in spontaneous ventricular fibrillation due to blunt chest trauma during the vulnerable repolarization phase [14]. The same applies to the diagnosis of potentially fatal myocarditis, which can of course also affect primarily “normal” hearts. Even if hardly any data exist regarding incidence and especially pathophysiological relevance, during and after febrile infections a sufficiently long break from sports should be taken to avoid affections of the myocardium [37–39]. And finally, the resting ECG also has insufficient sensitivity with respect to relevant CHD, which, as mentioned, affects younger and younger athletes [40, 41].
Despite these limitations, basic cardiac screening in young athletes can be considered a great success story: In Italy, where such screening has been required by law for all competitive young athletes for decades, an 89% reduction in the risk of sports-associated sudden cardiac death has been achieved [20, 21].
Implemented by the European Society of Cardiology (ESC), the International Olympic Committee (IOC) and the World Football Association (FIFA), among others, baseline screening for young athletes consists of three factors:
- Accurate collection of medical history (personal, system and family history),
- a focused cardiac status and
- of performing a 12-lead resting ECG(Fig. 2) [22, 42-46].
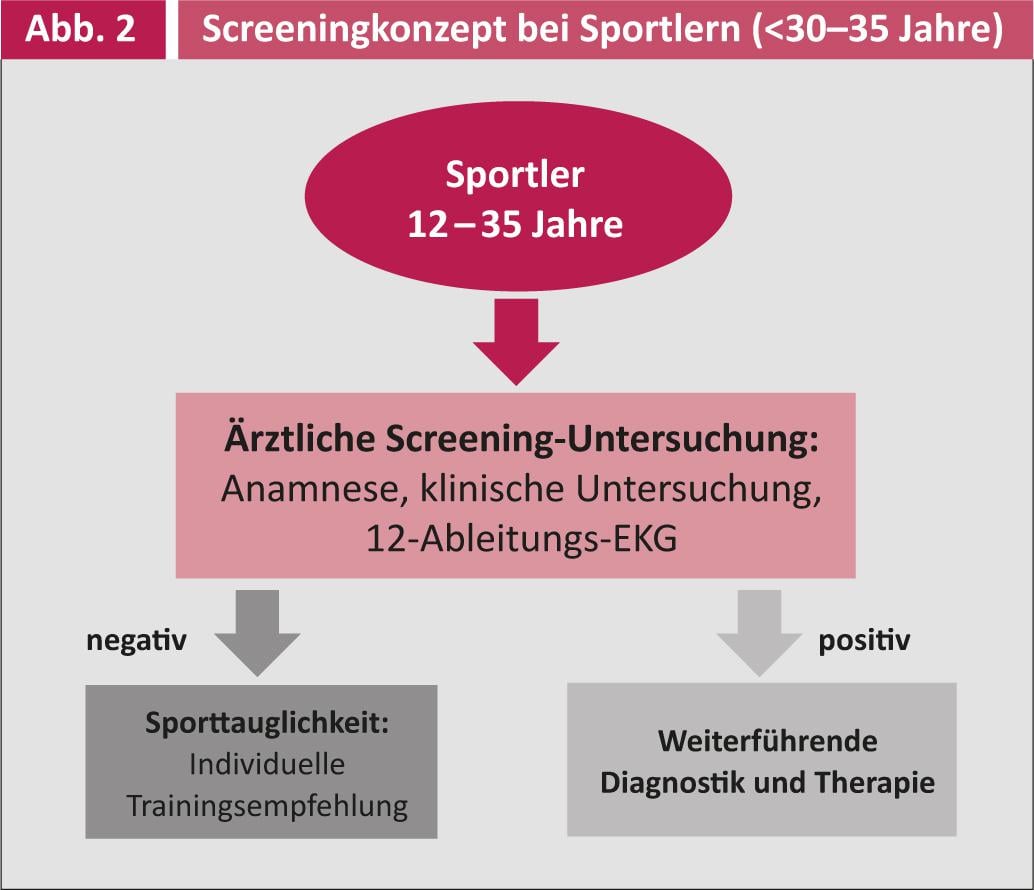
Regarding anamnesis questionnaires, the so-called “Lausanne Recommendations” of the IOC offer a nice overview and serve excellently as orientation guidelines [46]. Cardiac status usually focuses on cardiopulmonary auscultation, blood pressure measurements on both upper arms, and a review of any stigmata for connective tissue disease (e.g., using the Gent criteria [47]).
The adequate interpretation of the 12-lead ECG is the real “crux” in the screening of young athletes: A reduction in the specificity of the examination, which is mainly criticized because of many training-associated but benign ECG changes, has led many expert committees, especially in North America, to refrain from using an ECG in the basic screening of young athletes [48, 49]. These arguments have been clearly put into perspective by several very good papers in this field in recent years, and thus the so-called “Seattle Recommendations” are not only the most up-to-date and probably most accurate ECG interpretation guidelines, but also an expression of the insight of many American experts who participated in the development of the consensus statement [35, 50-53].
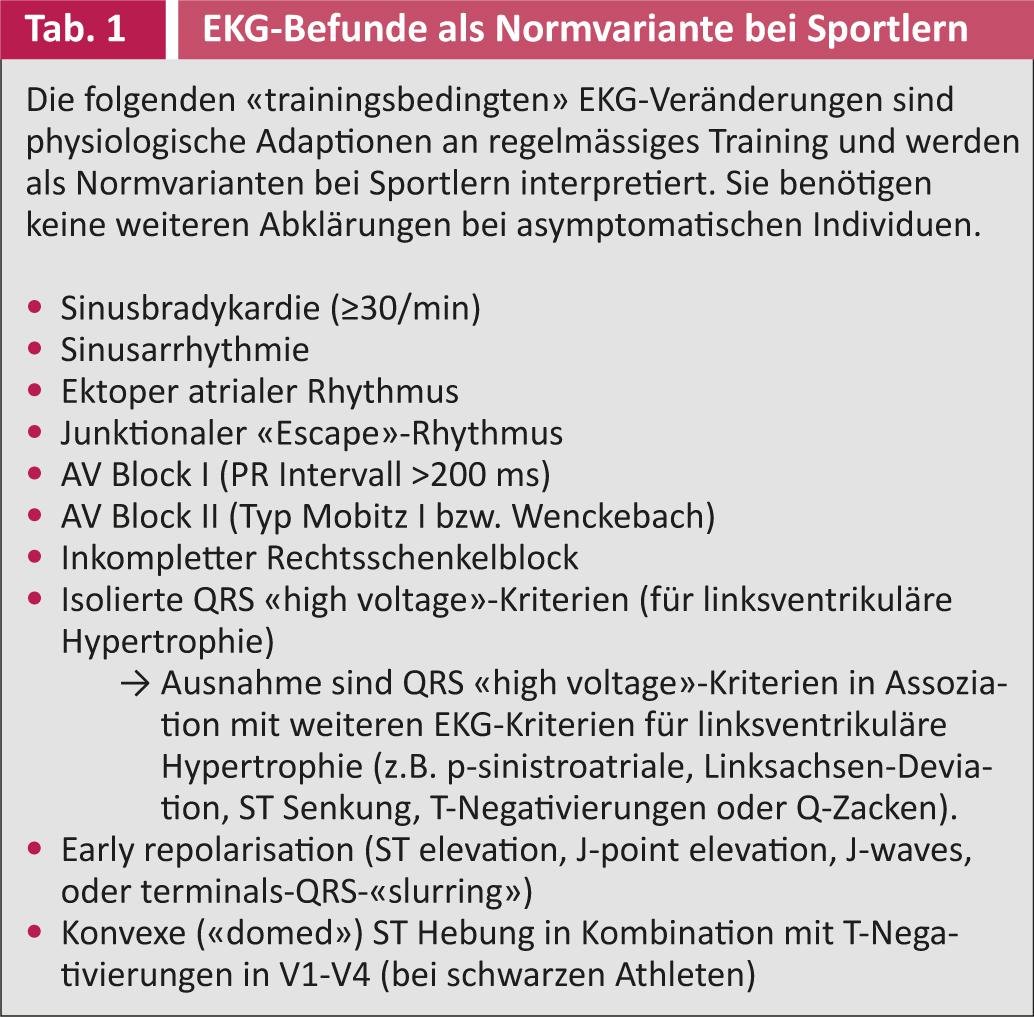
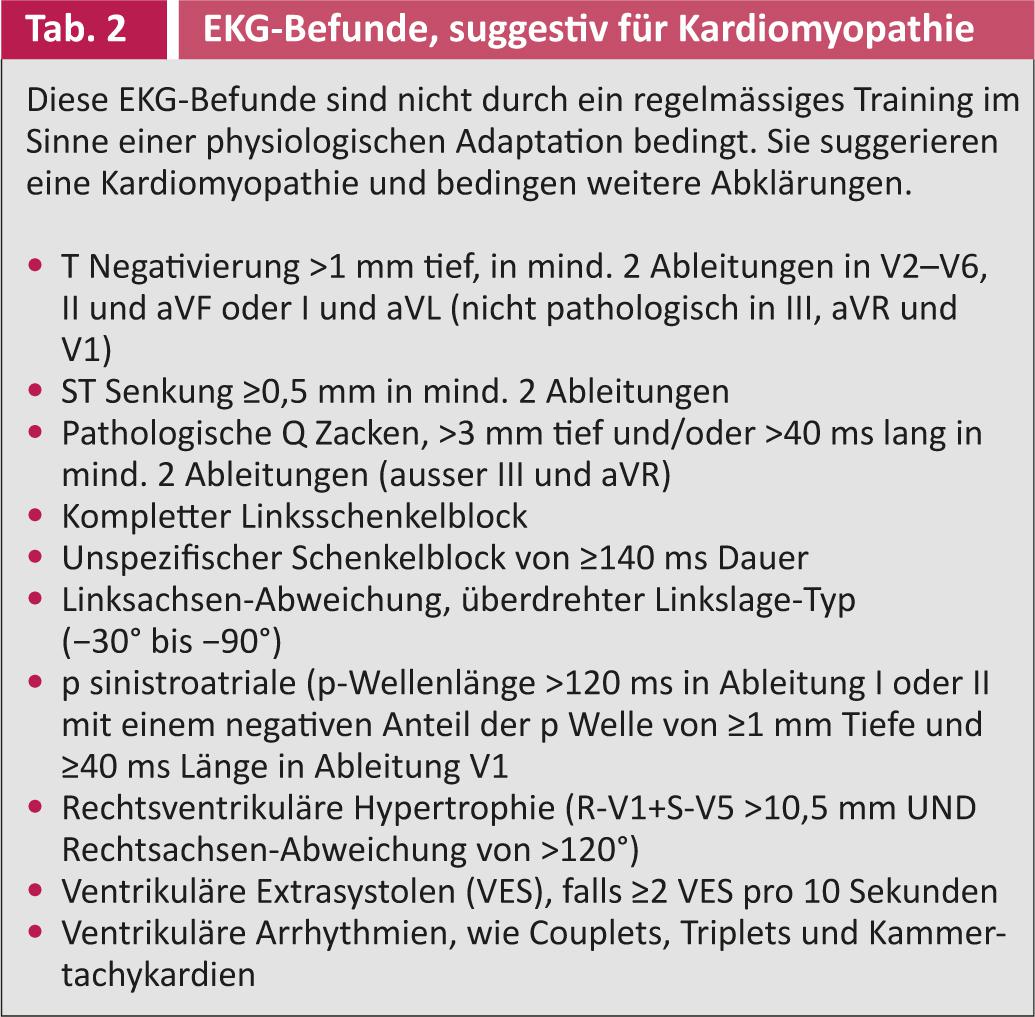
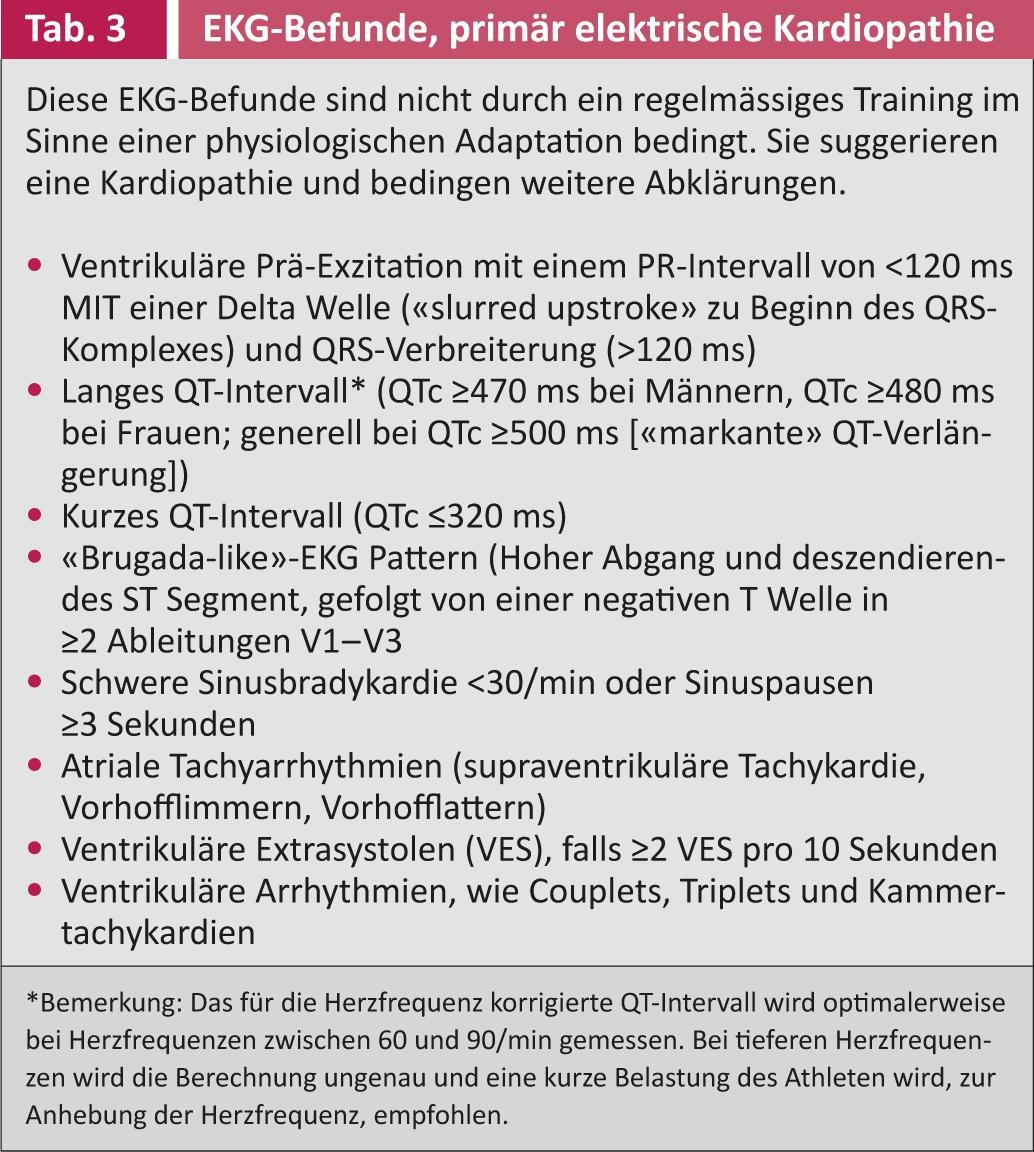
Crucial in the accurate assessment of the resting ECG of young athletes is the differentiation between physiological ECG findings due to regular training (e.g., increased vagotone at rest or physiological structural adaptations in the context of a “sports heart”) (Tab. 1) and pathological, either due to a structural (Tab. 2) or primary electrical (Tab. 3) cardiopathy indicative changes [35, 51, 52]. The ECG interpretation then leads to targeted further clarifications.
Ensure availability of an automatic defibrillator
Of course, as previously mentioned, despite optimal baseline screening, fatal cardiac events can still occur in sports [13, 14, 23, 24]. In these cases, adequate “first responder” measures must function on site. Although adequate cardiac massage is of course of the utmost importance in cardiopulmonary resuscitation, the availability and rapid use of an automatic defibrillator (AED) has proved to be absolutely crucial, as has been impressively demonstrated in the case of sudden cardiac arrest in athletes: While the survival rate in American university athletes in the event of sudden cardiac arrest, despite adequate cardiac massage, was only about 10%, it could be increased to a survival rate of 64% by using an AED. [53–56].
Despite this great importance, the availability of an AED is often insufficient [54, 57, 58]. In a survey conducted by FIFA, the world football governing body, only 68% of the federations surveyed reported having an AED available on pitch at official matches [57]. In official trainings, the situation is even more striking: only 35% of the federations have an appropriate device in place [57]. This alarming situation led to the further expansion of FIFA’s already extensive scientific and clinical-practice efforts to prevent sudden cardiac death in footballers [35, 42-45, 50-52, 59, 60] – each of the 209 member associations was provided with a “FIFA Medical Emergency Bag” containing an “extensive” assortment of rescue paraphernalia and medications, as well as an AED. The “11 steps to prevent sudden cardiac death in football” also includes the latest recommendations in this area [61].
Of course, pre-existing cardiovascular disease is by no means a general contraindication to exercise. However, an adequate sports recommendation is important for optimal and, above all, safe secondary prophylaxis. For this purpose, well-established European (European Society of Cardiology [39]) and American (36th Bethesda Conference, [38]) guidelines can be used.
Literature list at the publisher
Christian Marc Schmied, MD











