Contact allergy is a common cause of eyelid eczema. However, ocular involvement is also a symptom of many chronic inflammatory skin diseases. What are the differential diagnoses to consider? What are the new findings regarding treatment options? This article provides answers to these questions and more.
The fact that skin irritations are frequent in certain areas of the eye area is not only due to the heavy strain on the skin, but also has physiological reasons, explains Prof. Haase. For example, the skin in the eyelid region is considerably thinner than in the eyebrow region and two populations of sebaceous glands are present: Zeis’ sebaceous glands at the ciliary follicles, meibomian glands on the conjunctival side. Meibomian glands are large sebaceous glands that produce a secretion that plays an important role in the tear film [1].
“Air-borne” contact dermatitis and gold as allergen
Almost half of the cases of eyelid eczema are allergic contact eczema, atopic eyelid eczema is the cause in 26% of those affected and irritant eyelid eczema in 17.6%, seborrheic eczema accounts for a smaller proportion [1]. If the eczema is unilateral, it is most likely a contact allergic form; in other cases, the skin irritations usually occur bilaterally. The hit list of positive contact allergens in eyelid eczema is headed by gold, followed by perfumes, perubalsam, nickel, neomycin, quaternium and chloromethylisothiazolone [2,3]. If a specific substance is suspected as a trigger and/or a positive result in the epicutaneous test, avoidance of the possibly irritating factors can provide information. In the case of “air-borne” contact dermatitis caused by daisies, it is possible that only the eyelids are affected and no other skin areas are affected, said the speaker.
Regarding therapeutic options, there is a rather small evidence base, only a few studies specifically investigate therapeutics in the eyelid area. Experience-based treatment recommendations for contact allergic eczema include allergen avoidance and anti-inflammatory topical preparations such as low-potency corticosteroids (e.g., Ultracortenol eye ointment, Advantan®) or calcineurin inhibitors (e.g., Protopic®, Elidel®) [1]. Calcineurin inhibitors can be used, for example, if one wishes to avoid a risk of increased intraocular pressure associated with the use of topical steroids. Depending on the cause, antifungal therapeutics may also be used. With regard to eye care creams, a wide variety is available on the market, although care must be taken to ensure that no irritating ingredients are contained, such as formaldehyde or formaldehyde releasers, emphasizes Prof. Haase.
What are the differential diagnostic challenges?
Ocular involvement is present in more than half of all patients with rosacea, usually in the following manifestations: Blepharitis, conjunctivitis, keratitis, scleritis, iritis, neovascularization of the cornea. Approximately one-third of patients with rosacea have punctate corneal damage [1]. Empirical evidence shows pathogenetic correlations between clinical signs of blepharitis, extent of Demodex colonization of target follicles and bacterial counts of Staphylococcus aureus / Propionibacterium acnes [4,5]. The following other disorders should be considered in the differential diagnosis: Erysipelas, angioedema, perioral dermatitis, psoriasis, herpes simplex/herpes zoster, dermatomyositis. Periorbital erysipelas (preseptal cellulitis) refers to a bacterial infection of the skin as a result of sinusitis, impetigo, trauma, insect bites. Etiologically, infection with streptococci, staphylococci, and hemophilus is usually present. History of infectious disease may be present. Classic clinical symptoms include fever, pain on contact, and fatigue. Standard therapy includes antibiotics such as co-amoxicillin or cephalosporins. The symptoms of periorbital erysipelas and orbital phlegmon are similar in the initial stages. “Orbital phlegmon, or infestation of tissue proximal to the preseptal fascia, is an emergency and requires inpatient treatment,” Prof. Haase said.
Eyelid rim inflammation and “meibomian gland dysfunction”.
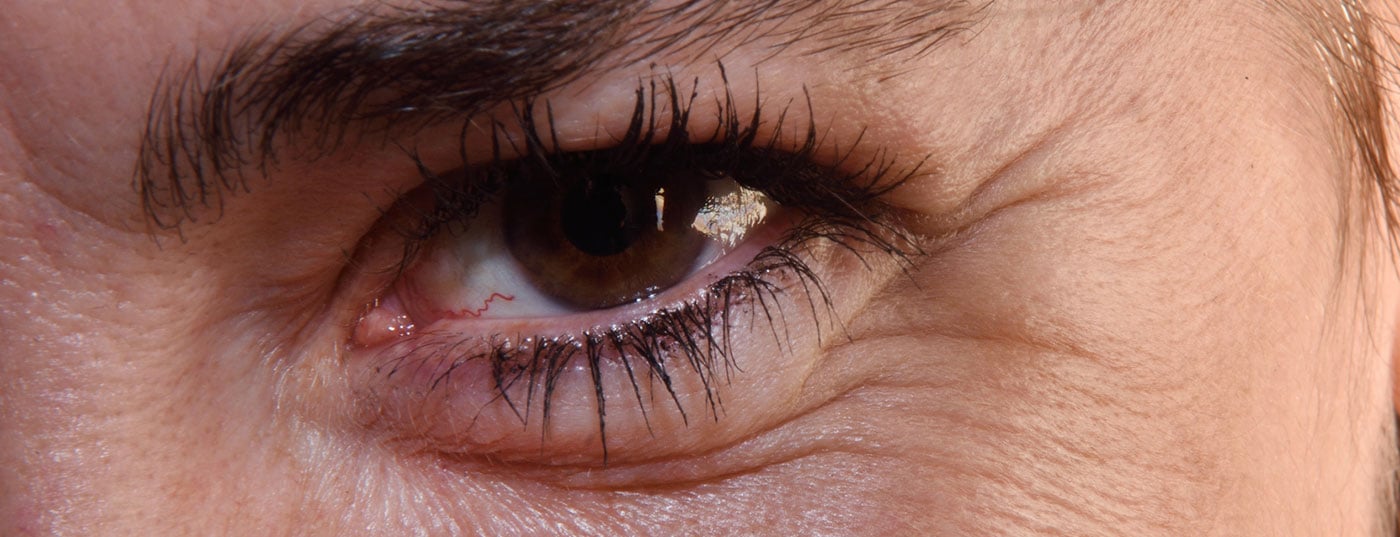
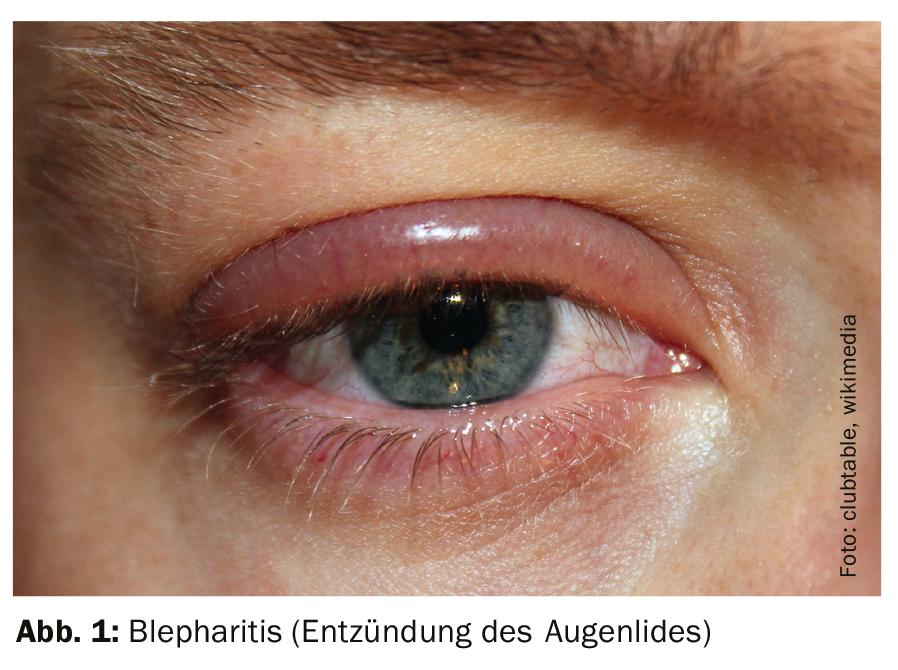
Anterior and posterior blepharitis are inflammations of the eyelid margins that are usually bacterial in origin. Blepharitis anterior is characterized by inflammation of the Zeiss glands and eyelash follicles and external hordeolum. If the cause is infectious, possible causative agents are bacteria. The most common sources of infection are Staphylococcus aureus, and less frequently Staphylococcus epidermis, Corynebacterium, Propionibacterium or Heliobacter. Sprout fungi (e.g. Pityrosporum ovale) or parasites (e.g. Demodex brevis, Demodex folliculorum) are also possible causative agents. Non-infectious causes are rarer, for example, blepharitis in the context of rosacea is possible, although there are still some gaps in knowledge about this at the present time [1,6]. Blepharitis anterior can also be localized, in which case only one or two follicles are affected, which is also called external hordeolum. Prof. Haase mentions that if bacterial blepharitis anterior is suspected, an examination using a reflected light microscope may be informative. If the cilia are surrounded by a scaly crust, this is an indication of bacterial causes; if this is demodex colonization, a tubular-cylindrical type of scaling at the lid margin is typical.
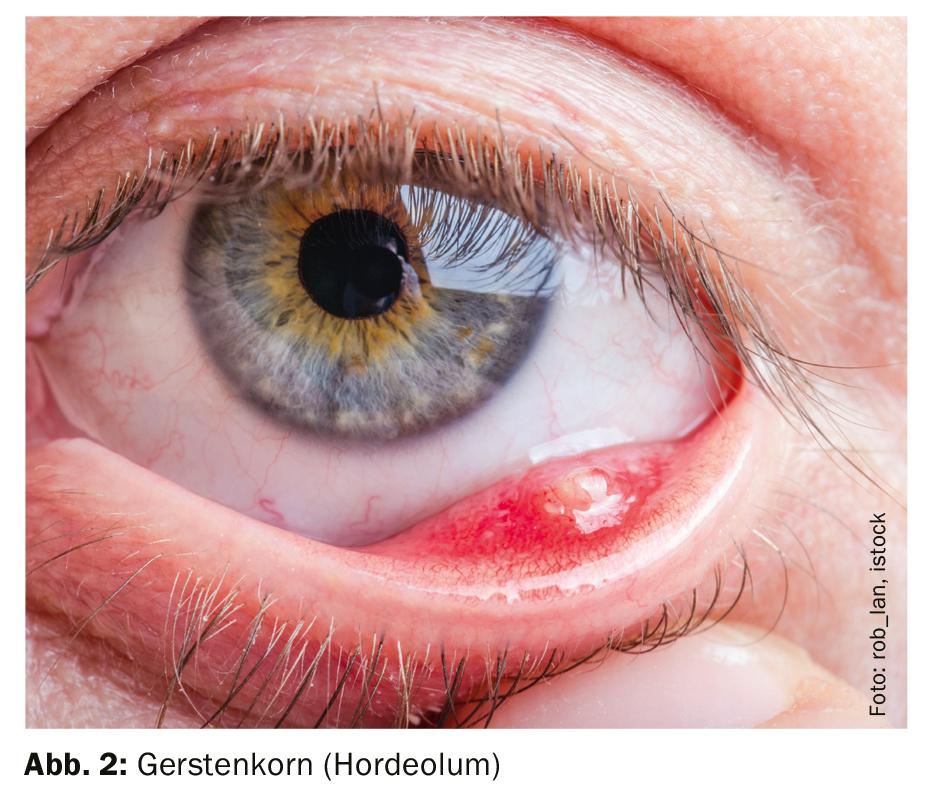
In posterior blepharitis, inflammation of the meibomian glands is present. Clinically, this manifests as either an internal hordeolum or a chalazion. An internal hordeolum is an acute, purulent infection caused by bacteria, shoot fungi, or mites. If this inflammation becomes chronic, chalazion, a chronic lipogranulomatous inflammation, forms. Differential diagnosis of a possible eyelid tumor should be distinguished [1]. For both internal hordeolum and chalazion, the viscosity of the sebum produced by the meibomian glands plays an important role. If the meibomian glands are clogged, they can no longer release their tear secretions, resulting in dry eye, also known as “meibomian gland dysfunction.”
Physical and drug therapy components
As therapeutic measures for blepharitis (Fig. 1), including hordeolum (Fig. 2), physical interventions (heat, cleaning of the eyelid margins, massage) have a high priority in addition to drug treatment. One goal is to get the secretion of Meibomian glands back into the tear film. Why in this case heat applications are recommended despite the presence of an inflammation has to do with the peculiarity of the secretion of the meibomian glands, explains the speaker. The secretion is present in gel-like form and must be liquefied to enter the tear film (“phase-transition”), which is temperature-dependent. With regard to cleaning wipes, the speaker explained that the wide range of wipes on the market also includes wipes containing tea tree extract, which is a substance that is toxic to demodex mites.
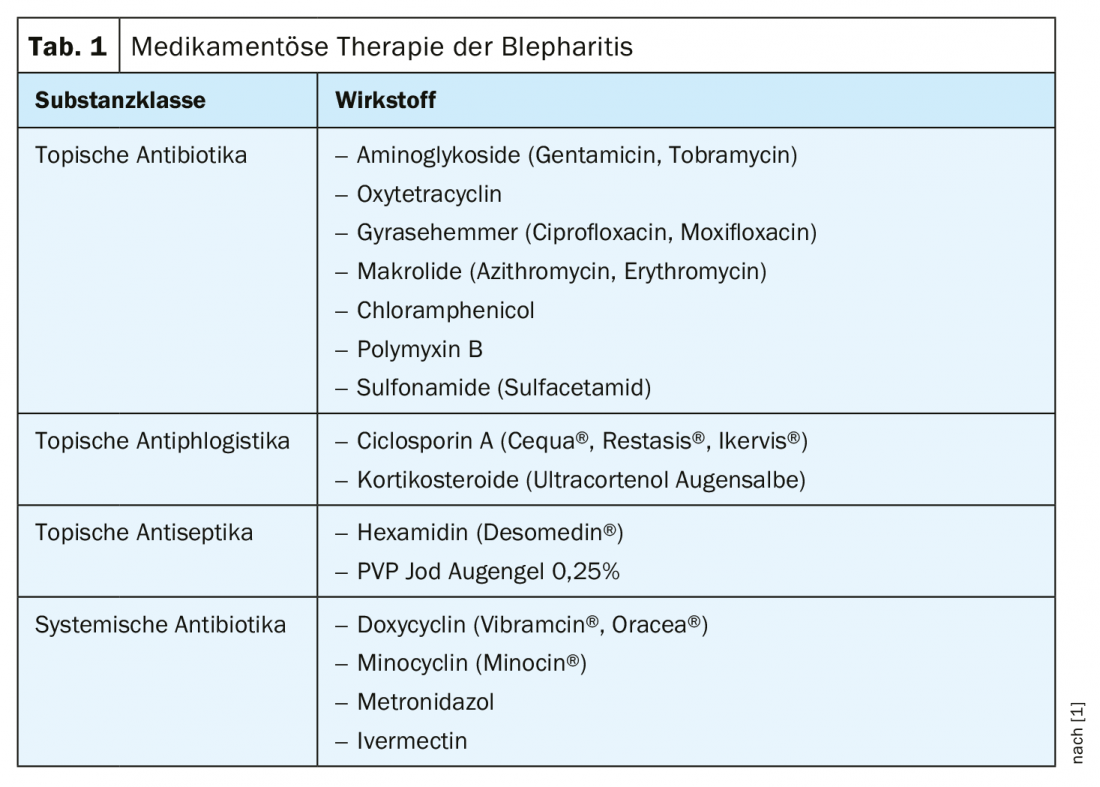
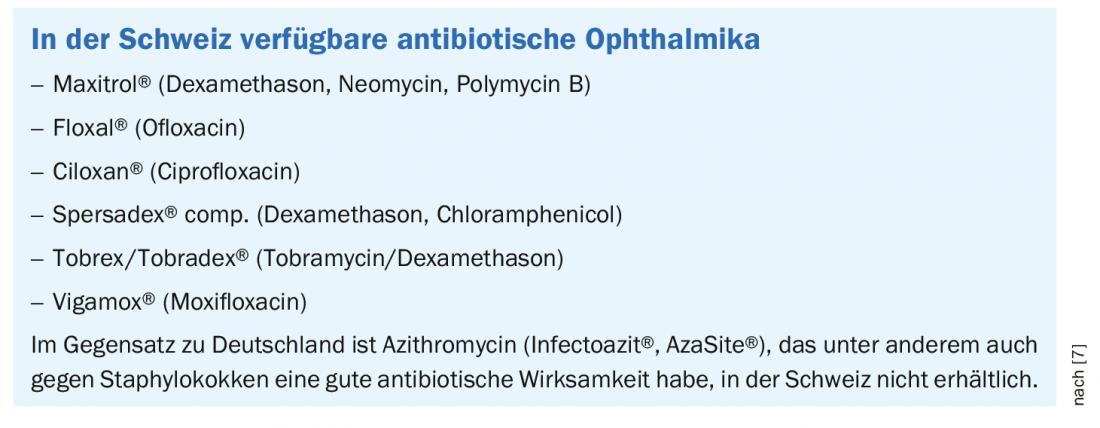
Pharmacotherapeutic measures may include topically applied preparations (antibiotics, possibly steroids) or systemic therapeutics (doxycycline, metronidazole, ivermectin) [1] (Table 1, box).
Literature:
- Haase I: Slide presentation: Update Course 3 – Inflammatory Dermatoses. Problem zones: inflammatory crisis areas of the skin, Prof. Dr. med. Ingo Haase, 9th Zurich Dermatological Training Days 2019, Zurich, June 27, 2019.
- Wolf R, Orion E, Tüzün Y: Periorbital (eyelid) dermatides. Clinics in Dermatology 2014; 32(1): 131-140.
- McDaniel LM, Couch SM: Allergic eyelid dermatitis as the sole manifestation of gold hypersensitivity. Ophthalmic Plastic & Reconstructive Surgery 2017; 33(4): e80-e82.
- Vieira AC, Mannis MJ: Ocular rosacea: common and commonly missed. J Am Acad Dermatol. 2013 Dec;69(6 Suppl 1):S36-41. doi: 10.1016/j.jaad.2013.04.042.
- Zhu M, et al: Quantitative Analysis of the Bacteria in Blepharitis With Demodex Infestation. Front Microbiol 2018; 9: 1719. doi: 10.3389/fmicb.2018.01719. eCollection 2018.
- Bradley JC: Anterior Blepharitis: Treatment Strategies. Ocular Surface Disease: Cornea, Conjunctiva and Tear Film, Expert Consult – Online and Print, 2013, 61-66.
- Foulks GN, Borchman D, Yappert, Kakar S: Topical azithromycin and oral doxycycline therapy of meibomian gland dysfunction: a comparative clinical and spectroscopic pilot study. Cornea 2013; 32(1): 44-53. doi: 10.1097/ICO.0b013e318254205f.
DERMATOLOGIE PRAXIS 2019; 29(4): 42-44 (published 8/28/19, ahead of print).