The line between low disease activity and remission in systemic lupus erythematosus is often imprecise. The question remains to what extent this can play a role for outcomes such as flare or mortality. Scientists have now addressed this and found that patients can be well positioned even without remission.
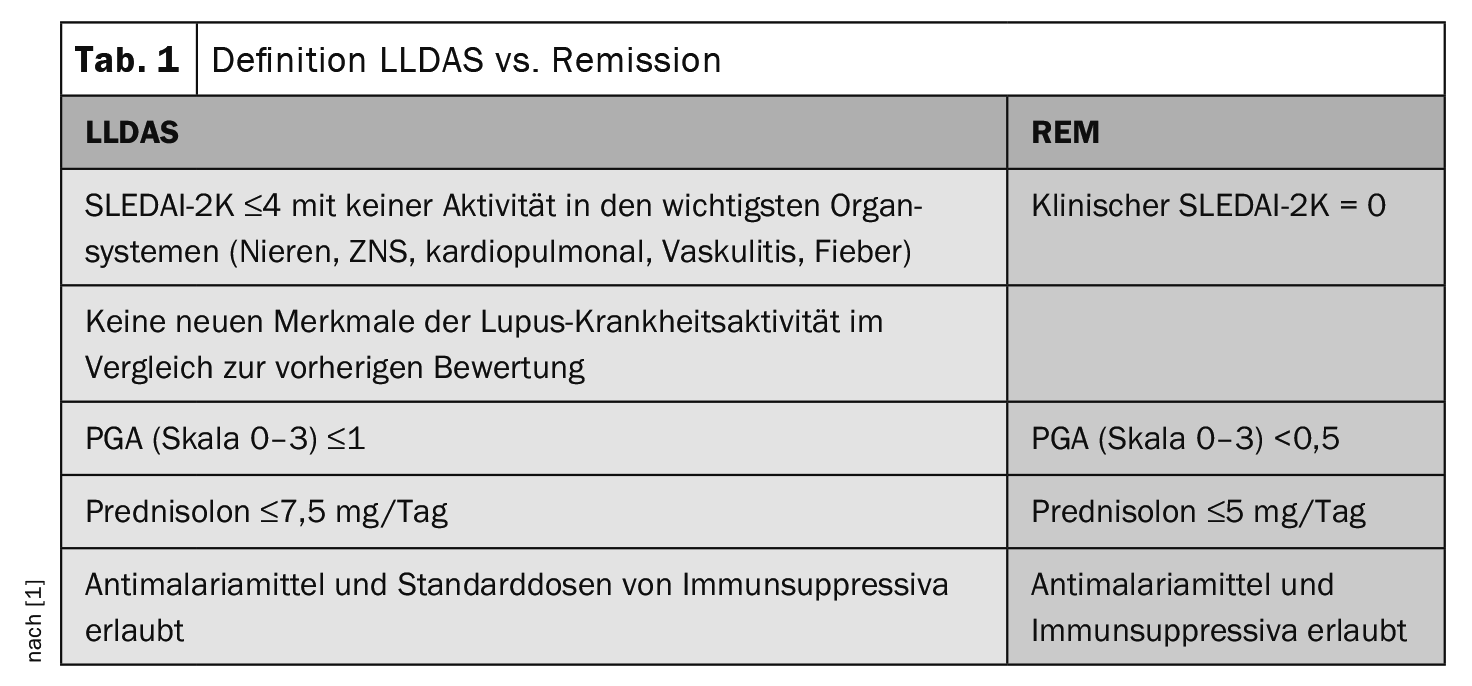
The Lupus Low Disease Activity State (LLDAS ) sets a limit for the acceptable disease and treatment burden in systemic lupus erythematosus (SLE) by establishing a maximum acceptable SLEDAI-2K of 4 and a maximum acceptable prednisolone dose of 7.5 mg/d. The definition of remission in SLE (DORIS) is stricter, but as there is overlap with LLDAS, many patients in LLDAS also fulfill the DORIS remission definition (Table 1). In most studies, LLDAS and remission (REM) are insufficiently differentiated from each other, but many patients with low disease activity are not in remission.
An international study group from Southeast Asia and Australia wanted to clarify whether low disease activity (LLDAS) but no remission (LLDAS+REM-) offers protection against adverse outcomes in SLE. The scientists analyzed data from the Asia Pacific Lupus Collaboration (APLC) Cohort and examined patients who met the LLDAS+REM criterion for the outcomes SLE relapses, increase in damage and mortality, explained Prof. Dr. Eric F. Morand, Centre for Inflammatory Diseases, Monash University, Melbourne [1].
The APLC cohort included adult SLE patients from 13 countries (ACR/SLICC criteria met) who were prospectively evaluated between 2013 and 2020. Demographic data (gender, age, ethnicity, year of onset) and diagnostic criteria (ACR and SLICC) were collected during recruitment (baseline). At all visits (3-6 monthly), disease activity (SLEDAI-2K, SFI, PGA), medication (PNL, AM, IS) and pathology (Cr, eGFR, Alb, Hg, Plt, WCC, etc.). At the start of the study and once a year, organ damage was also assessed using the ACR/SLICC Damage Index (SDI) and quality of life using the HRQoL(SF36v2) questionnaire.
Achievement of treat-to-target (T2T) per patient and visit
Of 3806 patients, 728 (19.13%) never achieved LLDAS or REM during the observation period. Low disease activity without remission was found in 687 (18.05%) of patients and low disease activity with remission (LLDAS+REM+) in 2391 (62.82%). These patients reached this stage one or more times. Prof. Morand considers the evaluation based on visits to be more informative: 38,663 patient visits were analyzed for this purpose. 50.1% of visits (n=19 370) did not meet the definition of either low disease activity or remission (LLDAS-REM-), 15.9% (n=6149) of visits were in low disease activity but not remission (LLDAS+REM-) and 34.0% (n=13 144) were in low disease activity and remission (LLDAS+REM+)
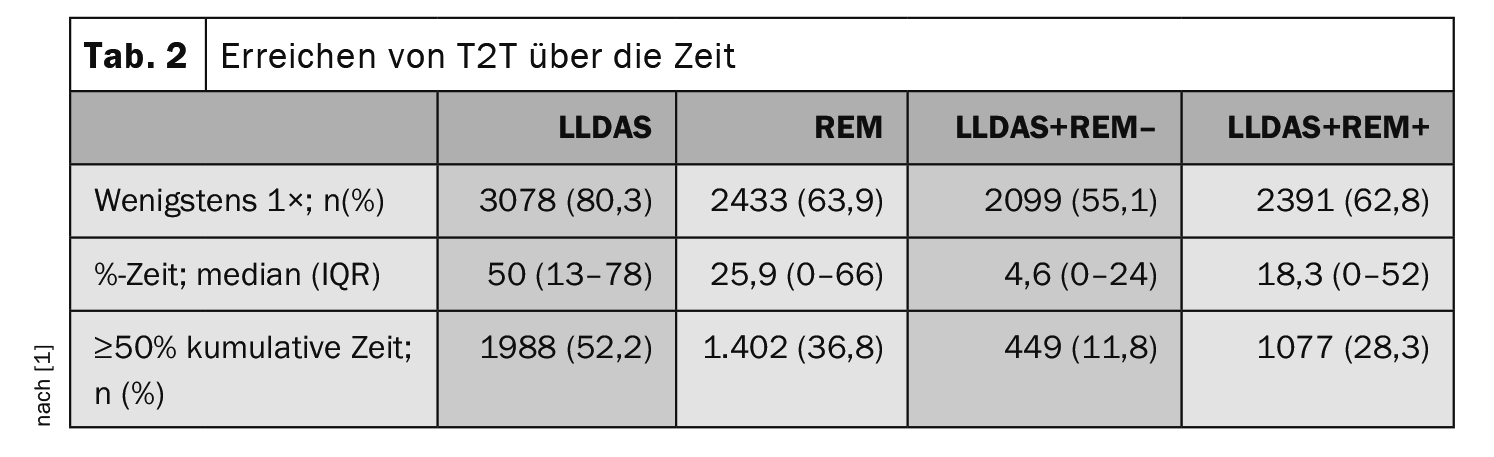
Over time, a period of low disease activity (LLDAS) was observed at least once in 80.3% of patients and remission was observed in 63.9% of patients. An episode of low disease activity without remission (LLDAS+REM-) was observed in 55.1% of patients and low disease activity with remission (LLDAS+REM+) in 62.8% of patients. 52.2% of patients were in LLDAS at least 50% of the time, 36.8% were in REM 50% or more of the time. 11.8% of patients were in LLDAS+ REM- for ≥50% of the time and 28.3% were in LLDAS+REM+ for ≥50% of the time (Table 2).
Significant for flare and organ damage
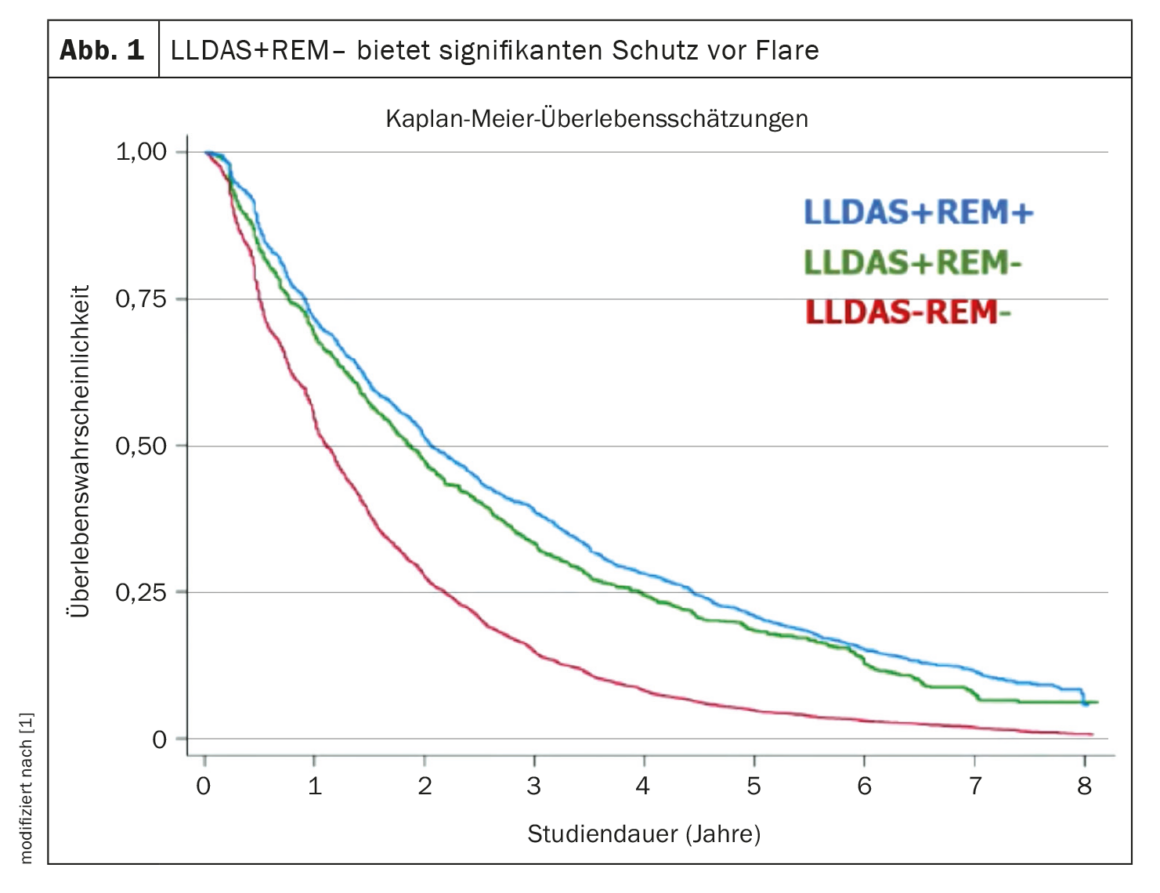
“The question of whether low disease activity without remission offers significant protection against relapses can be answered with a clear yes,” said Prof. Morand, summarizing the results of the study. As expected, the Kaplan-Meier curves for the occurrence of flare-ups in patients in remission were somewhat lower, but LLDAS+REM- still offered significant protection compared to patients without LLDAS (Fig. 1).
Patients who spent 50% or more of the time in LLDAS+REM- had a hazard ratio (HR) of 0.71 and a very small p-value (p<0.0001). Protection from flare in patients who were in LLDAS+REM+ was still slightly better with an HR of 0.62 (p<0.0001), “but the key finding is that low disease activity without remission still protects against disease flare.” With regard to increasing damage, the evaluation also showed that those who spent 50% or more of the time in LLDAS+REM- had a significant reduction in the increase in damage (HR 0.72; p=0.010). With LLDAS+REM+ there was slightly better protection against increasing damage (HR 0.64; p<0.001). But here too, the result was that low disease activity without remission still offers protection. With regard to protection against mortality, there was no statistical significance, as the number of deaths in the cohort between the three different conditions LLDAS-REM-, LLDAS+REM- and LLDAS+REM+ was insufficient.
Achieving low disease activity (LLDAS) offers significant protection against the occurrence of disease relapses and organ damage, even if patients who also meet the definition of remission are excluded, the speaker concluded. His research group therefore came to the conclusion that an LLDAS is an independent predictor of better treatment outcomes in SLE.
Source:
- Morand EF: Presentation “Attainment of lupus low disease activity state exclusive of remission is protective against adverse outcomes in systemic lupus erythematosus”; EULAR 2023, Milan, 2.6.2023 (online).
InFo RHEUMATOLOGIE 2023; 5(2): 21-22 (published on 12.12.23, ahead of print)