Inflammatory systemic diseases such as psoriasis are associated with a high risk of comorbidity. In addition to cardiometabolic diseases, mental disorders are particularly common in this patient population. As part of the long-term SDNTT(Swiss Dermatology Network for Targeted Therapies) study, data is being collected on the prevalence and course of comorbid mental disorders, among other things. New analyses showed that effective systemic therapy was associated with a reduction in psychological distress, with the best results being achieved with biologics.
A large European multicenter study showed that adult patients with skin diseases such as psoriasis, atopic dermatitis and hand eczema often suffer from psychological comorbidities [1]. Compared to the general population, adult psoriasis sufferers have a three times higher risk of anxiety disorders and depression. The estimated worldwide prevalence rate is 21–30%, with both disorders being underdiagnosed in psoriasis patients [1–4]. The SDNTT (Swiss Dermatology Network for Targeted Therapies) registry is a Swiss-wide real-world cohort with the overall aim of generating valid data on the efficacy and safety of systemic therapy in patients with psoriasis and psoriatic arthritis (PsA) [7]. Adult psoriasis patients who start a new systemic treatment are included; the follow-up phase lasts 20 years. In addition, data on comorbidities and the patients’ quality of life are collected. In this context, the researchers investigated the following questions [8]:
- What is the prevalence of anxiety disorders and depression (Hospital Anxiety and Depression Scale, HADS) [5] in a real-world setting?
- What are the predictors of anxiety and depression that can be identified using HADS?
- What effects does systemic psoriasis treatment have on psychological impairment (Patient Benefit Index subscale, PBI-Psych) [6]?
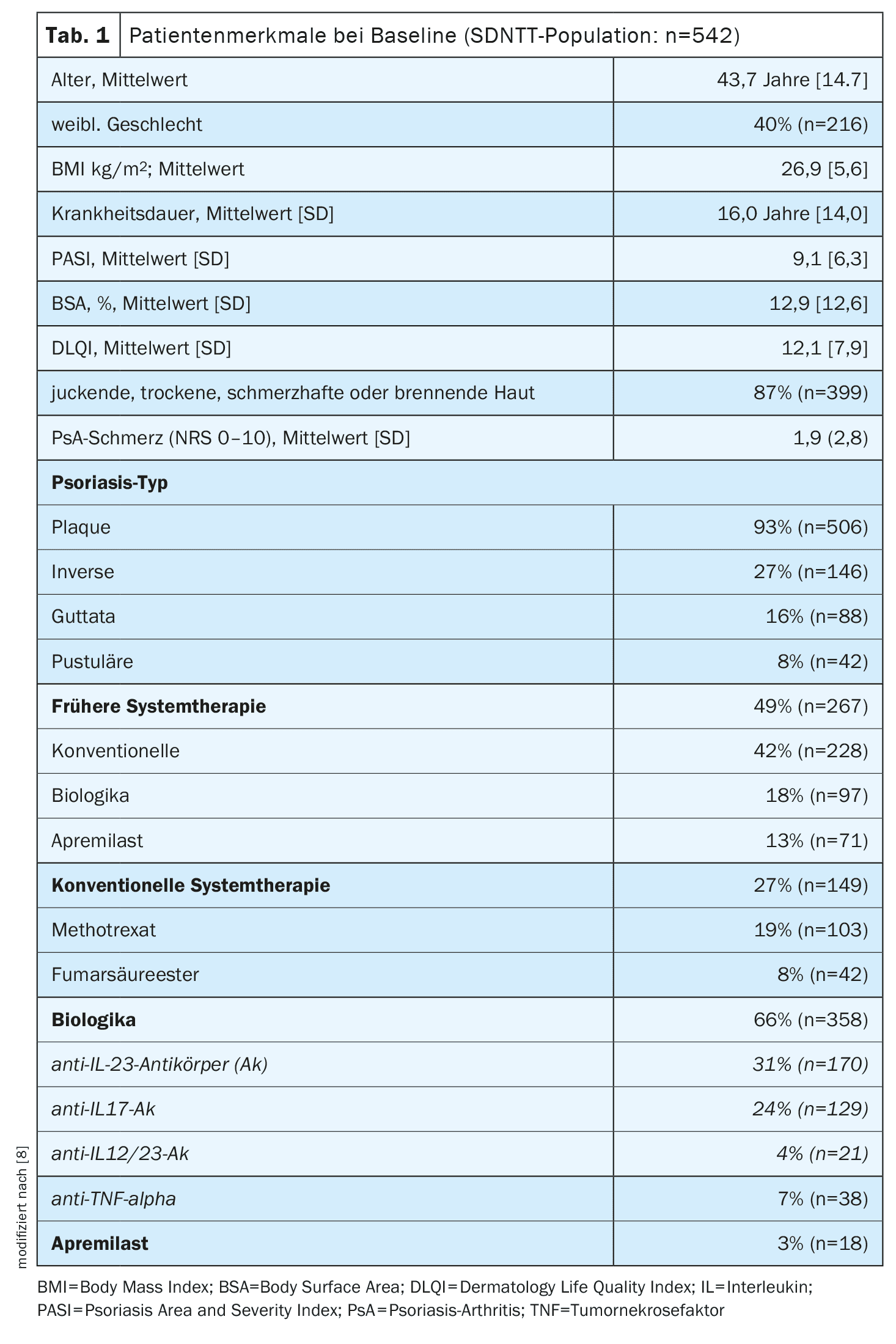
An analysis presented at this year’s SGDV congress included data from 542 psoriasis patients who were recorded between March 2017 and April 2024. 40% were female and the mean age at baseline was 43.7 [SD 14,7] years (Table 1). The mean PASI at baseline was 9.1 and the mean DLQI was 12.1. In 70% of cases, the newly initiated systemic therapy consisted of biologic treatment, 27% received conventional systemic therapeutics and 3% apremilast. A proportion of 49% of all participants had previously received systemic treatment. The predictors at baseline recorded using the HADS were assessed using multivariable linear regression and longitudinal correlations with the “reduction in psychological impairment” subscale of the Patient Benefit Index (PBI-psych), using a multivariate linear mixed-effects model (baseline vs. aggregated follow-up data). Of the 436 patients who completed the HADS questionnaire at baseline, 6% had a clinically diagnosed anxiety disorder or depression, while 63% (95% confidence interval [KI], 58-68%) were assessed by the HADS results as possibly having one of the two disorders and 44% (39-49%) as very likely to have one. In 92% of the patients who possibly had an anxiety disorder or depression based on the HADS, there was no clinical diagnosis.
Higher patient benefit with biologics than with conventional systemic therapy
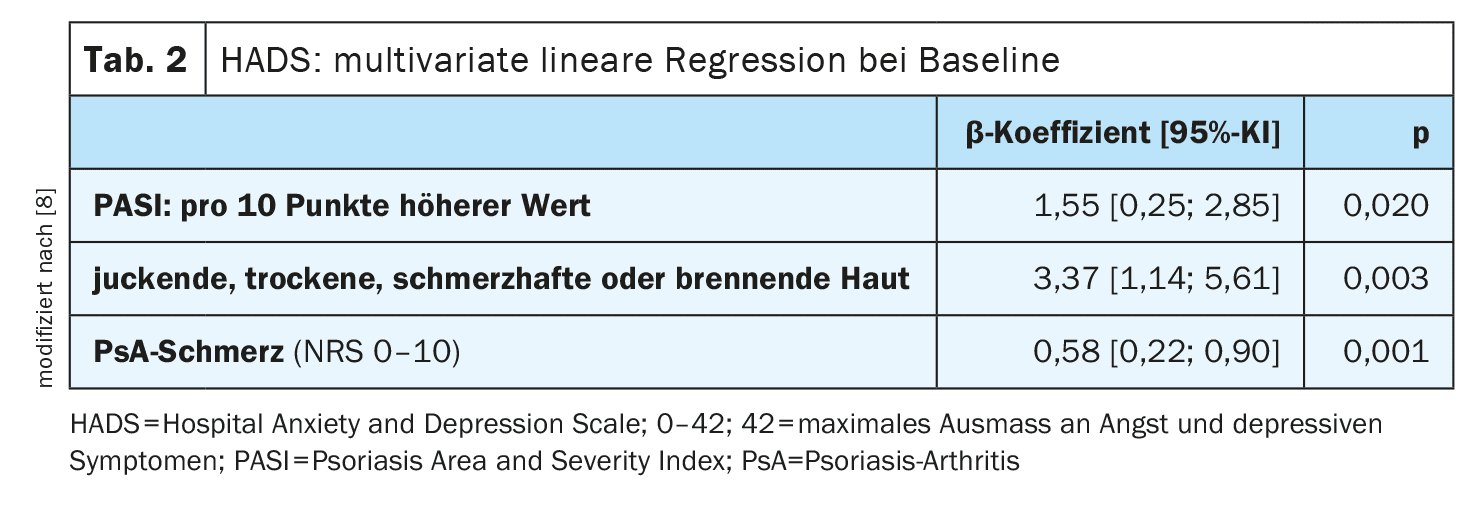
A multiple linear regression was performed to assess the strength and direction of the relationship between the parameters recorded using the PASI and HADS. This showed that anxiety disorders and depression were associated with higher PASI (Psoriasis Area and Severity Index) scores, PsA pain, as well as itchy, dry, painful and burning skin. Furthermore, higher DLQI scores predicted higher levels of anxiety disorders and depression. The Patient Benefit Index (PBI) was used to assess the patient benefit of dermatological therapy. The PBI consists of two self-explanatory questionnaires, one to be completed by the patient before and one after therapy [9]. Using the first of the two questionnaires, the Patient Needs Questionnaire (PNQ), patients rate how important the listed therapy goals are to them. Using the second questionnaire, the Patient Benefit Questionnaire (PBQ), patients can evaluate the achievement of the therapy goals during or after therapy. The results of the PNQ and PBQ are used to calculate an overall benefit score, which can range from 0 (no benefit) to 4 (maximum possible benefit). If the PBI is ≥1, this is considered a relevant patient benefit [10]. The PBI standard version (PBI-S) contains 25 items and can be used for all skin diseases, including psoriasis. The subscale “Reduction of psychological impairment” consists of the following items [11]:
- …to be less depressed,
- …to gain a zest for life,
- …to be able to lead a normal everyday life,
- …to be more efficient in everyday life,
- …to be able to pursue normal leisure activities.
In the present analysis, after 12 months of systemic psoriasis treatment, 80% of patients achieved a PBI-psych ≥1. This was associated with improvements in PASI (beta= -1.3 per 10 points; p<0.001) and DLQI (beta= -0.8 per 10 points; p<0.001). The reduction in psychological impairment was higher among patients receiving biologic therapy compared to conventional systemic treatment (beta=0.60; p=0.004). Of the patients treated with biologics, 31% received anti-interleukin (IL)-23 antibodies (Ak), 24% anti-IL-17-Ak and 4% anti-IL-12/23-Ak.
Nowadays, psychological impairment in psoriasis patients is no longer regarded exclusively as a consequence of the stigmatizing skin lesions, but systemic inflammatory processes are understood as a central component in a bidirectional interaction structure. However, not only patients with a high degree of psoriasis severity, but also those with milder forms can suffer from relevant psychological comorbidities, as several studies have shown [12–14].
In summary, it can be stated that a reduction in systemic inflammatory processes is not only an important therapeutic target for improving skin symptoms, but also for reducing psychological comorbidities, which was confirmed in the SDNTT cohort studied [8,12].
Literature:
- Dalgard FJ, et al: The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol 2015; 135(4): 984-991.
- Liu L, et al: Epidemiology of mental health comorbidity in patients with psoriasis: An analysis of trends from 1986 to 2019. Psychiatry Res 2023 Mar; 321:115078
- Jia YJ, et al: Prevalence of anxiety, depression, sleeping problems, cognitive impairment, and suicidal ideation in people with autoimmune skin diseases. J Psychiatr Res 2024; 176: 311-324.
- Dalgard FJ, et al: Dermatologists across Europe underestimate depression and anxiety: results from 3635 dermatological consultations. Br J Dermatol 2018; 179(2): 464-470.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67(6): 361-370.
- Blome C, et al: Dimensions of patient needs in dermatology: subscales of the patient benefit index. Arch Dermatol Res 2011; 303(1): 11-17.
- SDNTT (Swiss Dermatology Network for Targeted Therapies), www.sdntt.ch/de,(last accessed 15.11.2024).
- Schön V, et al.:Comorbid mental disorders in psoriasis patients and the effect of systemic therapy for psoriasis: a real-world nationwide cohort study of the Swiss psoriasis registry (SDNTT). Poster, SGDV Annual Congress, Basel, 18-20.09.2024.
- Augustin M, et al: Patient benefit index (PBI) – a novel approach in patient-defined outcomes measurement for skin diseases. Archives of Dermatological Research 2009, 301(8): 561-571.
- Schäfer I, et al: Quantitative benefit assessment from the patient’s perspective – the Patient Benefit Index (PBI). Congress Medicine and Society 2007, Doc07gmds676.
- Blome C, et al: Dimensions of Patient Needs in Dermatology: Subscales of the Patient Benefit Index. Arch Dermatol Res 2011: 303(1): 11-17.
- Hölsken S, Krefting F, Schedlowski M, Sondermann W: Common Fundamentals of Psoriasis and Depression. Acta Derm Venereol 2021 Nov 30; 101(11):adv00609. doi: 10.2340/actadv.v101.565.
- Kleyn CE, et al: Psoriasis and mental health workshop report: exploring the links between psychosocial factors, psoriasis, neuroinflammation and cardiovascular disease risk. Acta Derm Venereol 2020; 100: adv00020.
- Patel N, et al: Psoriasis, depression, and inflammatory overlap: a review. Am J Clin Dermatol 2017; 18: 613-620.
HAUSARZT PRAXIS 2024; 19(12): 56-57 (published on 12.12.24, ahead of print)
DERMATOLOGIE PRAXIS 2024: 34(6): 32-33