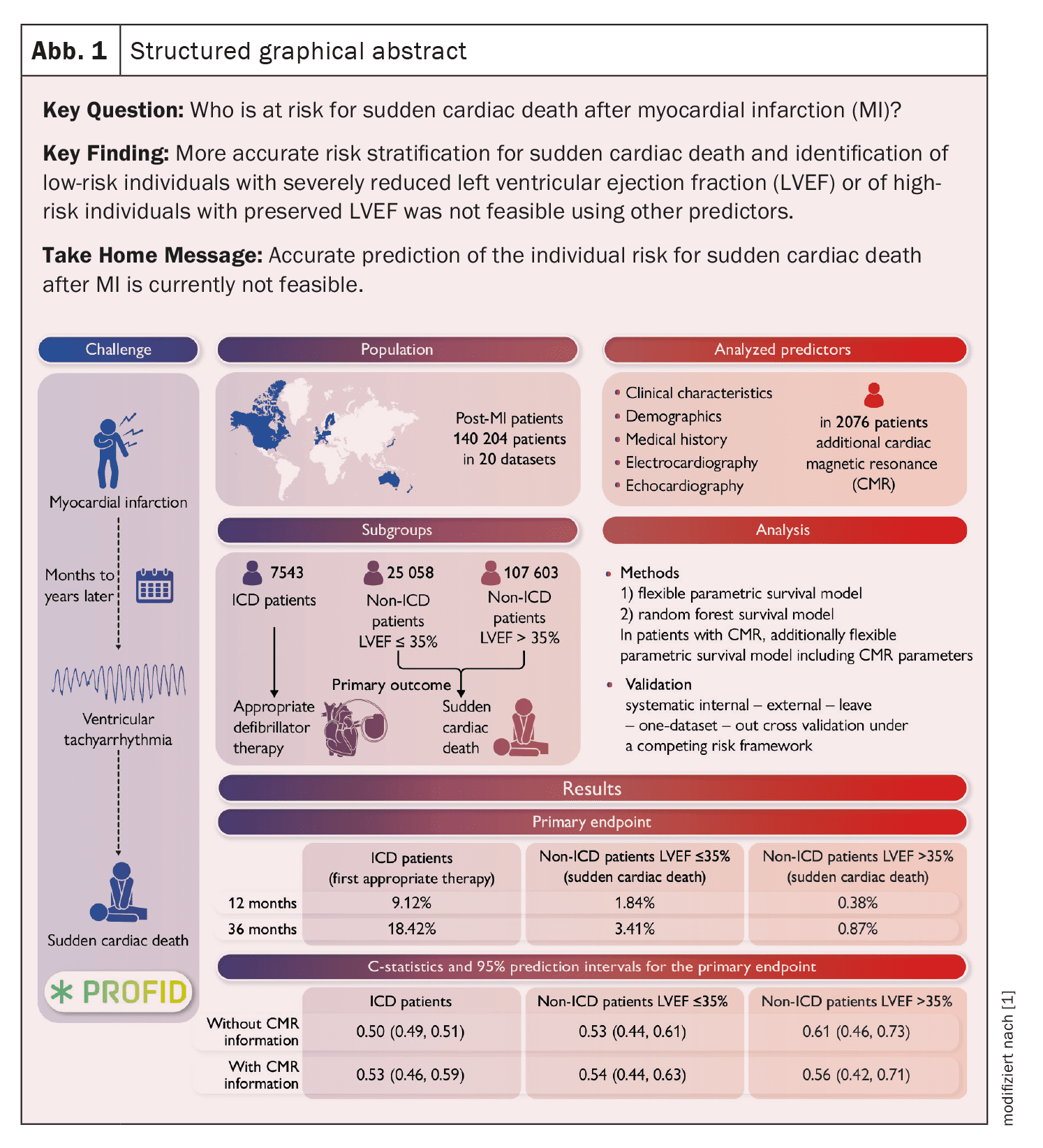
Sudden cardiac death (SCD) is one of the leading causes of death worldwide and is particularly common in patients who have survived a myocardial infarction (MI). Despite significant advances in medical care, the prediction and prevention of PHT remains one of the greatest challenges in cardiology practice. Current research shows that traditional indicators such as left ventricular ejection fraction (LVEF) are often insufficient to reliably identify high-risk patients or exclude low-risk patients. A comprehensive analysis of the PROFID cohorts, comprising more than 140,000 patients, has examined this issue in more detail and provides new insights that suggest a fundamental reassessment of current strategies.
(red) PHT accounts for around 20% of all deaths worldwide and often affects patients with a history of MI. It usually results from life-threatening ventricular arrhythmias such as ventricular fibrillation or ventricular tachycardia. The implantable cardioverter defibrillator (ICD) is considered the gold standard in prevention, as it is able to detect and treat such arrhythmias at an early stage. However, the decision to implant is traditionally based on LVEF, which has been used as the main criterion for the risk of PHT for decades.
Despite this established practice, recent data show that LVEF alone is often insufficient. While it is a useful guideline for some patients with severely reduced LVEF (<35%), a significant proportion of PHT cases in patients with moderately reduced or preserved LVEF go unrecognized. At the same time, many ICDs are implanted in patients with LVEF ≤35% who ultimately never require ICD therapy. This highlights the need for improved risk stratification that optimizes both patient safety and the efficiency of medical resources.
Aim of the PROFID analysis
The aim of the PROFID analysis was to improve the prediction accuracy for PHT after MI and to develop better criteria for ICD implantation. The focus was on two central questions:
- Identification of low-risk patients: Can patients with severely impaired LVEF who do not require an ICD be identified because their risk of PHT is low?
- Identification of high-risk patients: Can patients with moderately reduced or preserved LVEF who would benefit from targeted ICD therapy be identified?
Individual patient data from 20 international cohorts were pooled and analyzed. The analysis included various predictive models, including flexible parametric survival models and random forest models, to maximize predictive accuracy.
Methodology
The analysis included data from 140,204 patients who were divided into three main groups according to MI:
- ICD patients: Patients with LVEF ≤35% who had received an ICD implantation for primary prevention.
- Non-ICD patients with LVEF ≤35%.
- Non-ICD patients with LVEF >35%.
The predictive performance of LVEF and other parameters was investigated with regard to the risk of PHT and the frequency of ICD therapy (in ICD patients). Data on clinical characteristics, biomarkers, echocardiographic parameters and, in some cases, cardiac MRI were analyzed.
Primary endpoints
The primary endpoints were:
- Sudden cardiac death (in non-ICD patients): Defined according to the Hinkle-Thaler classification.
- Appropriate ICD therapy (for ICD patients): Measured as antitachycardia pacing or shock delivered by the ICD.
Statistical analysis
Predictive performance was assessed by systematic internal and external cross-validation. C-statistics (as a measure of discriminatory ability) and model calibration were calculated to assess predictive accuracy.
Results
1. limited predictive power of LVEF
LVEF was found to be a weak predictor of the risk of PHT, regardless of whether it was severely reduced, moderately reduced or preserved. The C-statistic for LVEF was close to 0.50 in all groups, indicating low discriminatory power:
- ICD patients: 0.50 (95% confidence interval: 0.49-0.51).
- Non-ICD patients with LVEF ≤35%: 0.53.
- Non-ICD patients with LVEF >35%: 0.56.
2. additional parameters did not improve the prediction
The integration of additional parameters such as clinical characteristics, biomarkers or electrocardiographic data did not lead to any significant improvement in predictive accuracy. The analysis of MRI data, including scar tissue and gray areas, also showed no significant additional benefit.
3. low event rates in patients with preserved LVEF
In patients with LVEF >35%, the overall risk of PHT was very low, so identifying high-risk patients in this group remains difficult. At the same time, the rates for ICD therapies were significantly higher in patients with LVEF ≤35%, suggesting a possible overestimation of risk in this group.
Limitations of current practice
The results of the PROFID analysis highlight the weaknesses of current practice, which relies heavily on LVEF. Although LVEF is a proven marker of global cardiac function, it does not reflect the specific mechanisms that lead to PHT. Particularly problematic is the inability of LVEF to distinguish between PHT and non-sudden deaths.
Challenges in risk stratification
Sudden cardiac death is the result of a complex interaction of several dynamic factors that are difficult to capture with one-off measurements. In addition, variations in the classification of causes of death and the heterogeneity of the cohorts studied make it difficult to generalize the results.
Future prospects
The results of the PROFID analysis have important implications for cardiology practice:
- Re-evaluation of ICD criteria: Routine ICD implantation in patients with LVEF ≤35% should be critically scrutinized in light of declining PHT rates and improved drug therapies.
- Focus on new biomarkers: Future research should concentrate on dynamic and multivariate models that can better reflect the complex mechanisms of PHT.
- Personalized prevention: Innovative technologies such as artificial intelligence and big data could help to determine individual risk profiles more precisely and optimize prevention.
- Cost-benefit analysis: Given the high costs and potential complications of ICDs, a stronger focus on the efficiency of resource utilization is required.
Conclusion
The PROFID analysis shows that LVEF alone does not provide a sufficient basis for risk stratification after myocardial infarction. Neither LVEF nor additional parameters were able to achieve satisfactory predictive accuracy. These results emphasize the urgent need to develop new approaches for risk stratification and prevention of sudden cardiac death. Future strategies should be based on multidimensional models that integrate clinical as well as genetic and biometric data to enable more precise and personalized care.
Source:
- Peek N, Hindricks G, Akbarov A, et al: Sudden cardiac death after myocardial infarction: individual participant data from pooled cohorts. Eur Heart J 2024 Nov 14; 45(43): 4616-4626. doi: 10.1093/eurheartj/ehae326. PMID: 39378245; PMCID: PMC11560274.
CARDIOVASC 2024; 23(4): 28-29