Intravenous fibrinolysis is an established, validated, and efficient treatment for acute cerebral stroke. In severe neurologic deficits, there is usually occlusion of a major cerebral artery. In these cases, the prospect of rapid recanalization by intravenous therapy alone is low. In multicenter, controlled, and randomized trials, endovascular therapy, which can achieve mechanically rapid and high rates of recanalization of large occluded basilar cerebral arteries, has been shown to result in better clinical outcomes for patients when combined with systemic lysis than intravenous therapy alone. The time factor remains decisive. Patients with stroke should be treated as soon as possible and transferred to specialized centers (stroke centers). In patients in whom lysis is contraindicated (e.g., patients on Marcoumar® therapy), mechanical thrombectomy is possible and is a good alternative.
Our aim in this article is to provide an update on endovascular stroke therapy, taking into account recent studies demonstrating its efficacy in combination with intravenous therapy.
In recent years, the tools for endovascular revascularization for high-grade intracranial stenosis and vascular occlusion have improved considerably. Micro-stents and very flexible suction systems now allow intraluminal clots in the basal cerebral arteries to be removed within a very short time. Recanalization rates by such mechanical maneuvers are significantly higher than after intravenous or intra-arterial drug lysis therapy alone. From a pathophysiologic perspective, the timing of reperfusion plays the greatest role in the patient’s prognosis.
Recently published controlled randomized trials have shown that immediate mechanical revascularization for occlusion of a large basilar cerebral artery in combination with intravenously initiated lysis therapy immediately after exclusion of hemorrhage results in significantly better patient clinical outcome than intravenous lysis therapy alone. This means that a patient with cerebral stroke and occlusion of a major cerebral artery should be transferred urgently and as quickly as possible to a stroke center where this combined therapy is offered.
Acute cerebral stroke is ischemic in approximately 80% of cases. Brain strokes are the third leading cause of death in Switzerland as well as the most common reason for permanent disability. Pathophysiologically, an ischemic stroke is defined by acute occlusion of a brain-supplying artery at the cervical level or intracranially. If the occlusion leads to a critical undersupply of the brain parenchyma, acute neurological deficits result, depending on the territory affected. The nature and extent of the deficit depend on the extent and localization of the perfusion deficit.
The most common cause of ischemic stroke in the anterior circulation is cardiac embolism, followed by arterio-arterial thromboembolism. In the posterior circulation, secondary thromboembolism is the more common cause of vascular occlusion in the presence of underlying stenosis. Artherosclerotic stenoses are the underlying pathomechanism in approximately 60% of basilar artery thromboses.
Possible consequences of circulatory impairment range from a transient ischemic attack (TIA) only, to mild to severe permanent neurologic and disabling deficits, to death.
Intracranial vascular occlusion involves several pathophysiologic aspects that influence the patient’s prognosis. Some parameters are crucial for the course in vascular occlusion:
- Extent of the underperforming resp. non-perfused brain area, this depending on the size of the occluded artery and the collateral vessel supply
- Duration of ischemia
- Occurrence of complications (e.g., intracranial hemorrhage as hemorrhagic infarct transformation or consequence of treatment).
Better prognosis with successful recanalization
A meta-analysis by Rha et al. from 2007 [1] shows that successful recanalization is the most important determinant of favorable outcome. This analysis included 53 studies involving 2066 patients and concluded that there was a strong correlation between recanalization and functionally good outcome and reduced mortality. It also became clear that recanalization depends on the type of treatment. Recanalization occurred spontaneously in 24.1% of patients, after intravenous fibrinolysis in 46.2%, after intra-arterial fibrinolysis in 63.2%, after combined use of drug intravenous and -arterial lysis in 67.5%, and after mechanical approach in 83.6%.
The largest stroke trial, NINDS, demonstrated that intravenous fibrinolysis showed significantly better results compared with placebo if therapy was started within the first three hours after symptom onset. However, the study also showed that severely affected patients with an NIHSS >16 did not appear to benefit from intravenous lysis. Intravenous fibrinolysis (ECASS III) still produces a significantly better outcome within 4.5 hours of symptom onset compared with placebo, but is more often associated with symptomatic bleeding.
Because NIHSS correlates with the size of the occluded artery, especially in acute cerebral stroke due to occlusion of a large cerebral artery, alternative treatment measures such as mechanical clot extraction are very significant. Meanwhile, recently published case series show recanalization rates of more than 90% when newer mechanical procedures are used for embolectomy.
Recent controlled, randomized multicenter trials confirm a benefit of mechanical embolectomy in combination with intravenous lysis therapy compared with intravenous therapy alone. For example, the MR CLEAN trial (Multicenter Randomized Clinical trial of Endovascular Treatment in the Netherlands) [2] showed a better clinical outcome 90 days after stroke in the interventional arm in patients with vascular occlusion in the anterior cerebral circulation and treatment within the first six hours after symptom onset. All secondary outcome parameters (NIHSS at 24 hours and at 1 week, recanalization, and final infarction) were significantly better in the interventional group.
Based on these results, some trials were stopped, e.g., SWIFT PRIME (Solitaire™ With the Intention For Thrombectomy as PRIMary treatment for acute ischemic strokE) [3] and EXTEND IA (EXtending the time for Thrombolysis in Emergency Neurological Deficits with Intra-Arterial therapy) [4], because an interim analysis confirmed the benefit of the combined approach.
Advantages and disadvantages of endovascular therapy
The endovascular approach has several advantages. Intra-arterial fibrinolysis therapy achieves a higher drug concentration locally at the site of arterial occlusion than intravenous administration. This reduces the systemic dose and reduces potential complications. A combination of fibrinolysis and mechanical clot mobilization increases the target for interaction of the applied drug with the clot. Another option for recanalization is direct mechanical clot removal by local suction or mechanical extraction.
Potential disadvantages of endovascular therapy are vessel injury and clot migration with occlusion of initially unaffected arteries.
Devices for mechanical recanalization
The various devices for mechanical recanalization differ in principle.
Some systems must first be advanced through the occluded vessel segment and then capture and retrieve the clot during retraction (clot retriever). So-called retrievable stent retrievers are inserted via a microcatheter that must first pass through the occluded vessel segment. If the open vessel section distal to the clot is reached, the stent with its distal portion can be placed or released and opened at this point, which – depending on the thrombus material – often leads to a very rapid reopening of the vessel. The stent retriever is subsequently removed including the captured clot.
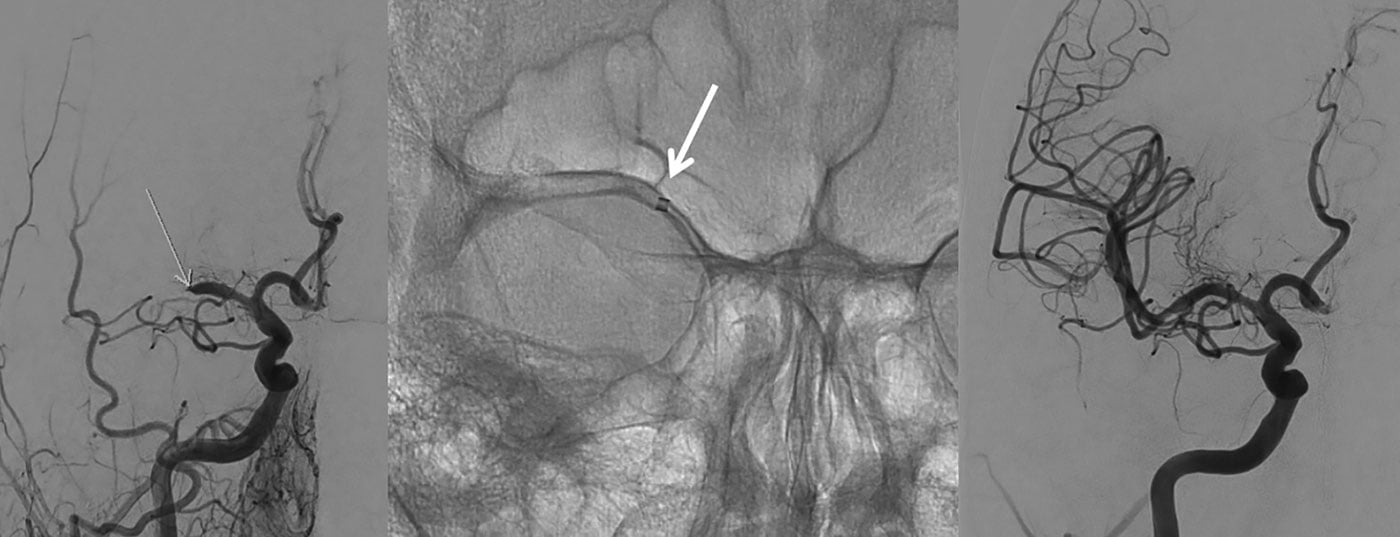
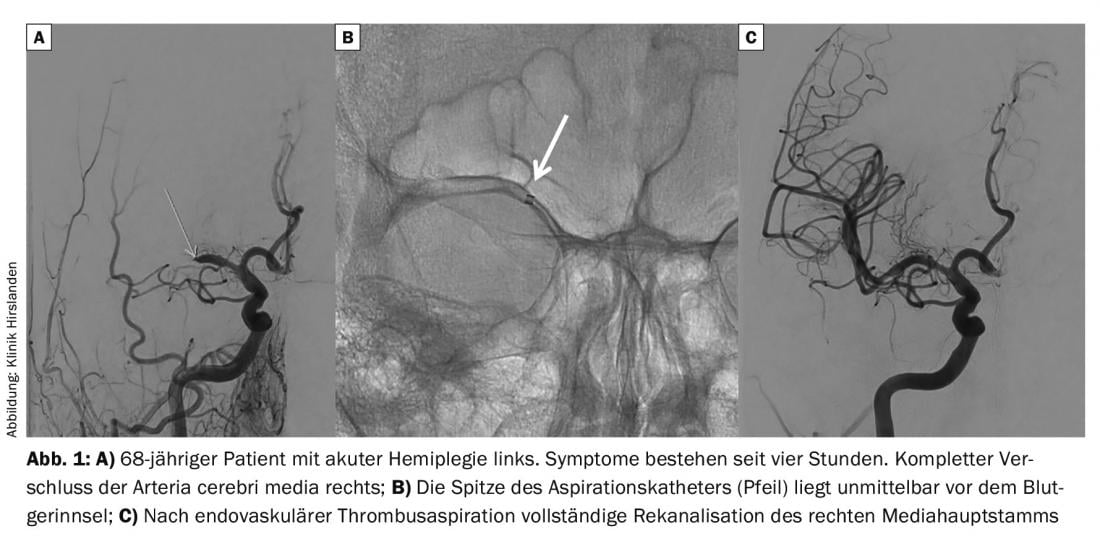
Another principle for recanalization of an occluded vessel section is successive removal of the thrombotic material from proximally by guiding a suction system to the site of occlusion. The suction system is a now very flexible, large-lumen catheter with which the clot is aspirated and removed under aspiration (i.e., with continuous negative pressure) when the suction catheter is removed (Fig. 1) . This system allows quite rapid removal of the clot or larger parts of the thrombus, especially if they are soft. The system is not efficient for very hard and/or calcified clots.
The corresponding systems are now extremely flexible, which is the prerequisite for superselective probing of intracranial arterial vessel sections.
Overall, the success of endovascular therapy depends on several factors, such as vessel anatomy (elongation), vessel diameter, or clot condition. In our experience to date, a “fresh” clot can be removed better with a suction system than an older organized clot, for which a retriever may be better suited for extraction. Since the cause of a vascular occlusion is not always known or obvious, the primary system used does not always lead to success. Sometimes two systems have to be combined or used one after the other. Also, if any vascular stenoses are present, they can be addressed and corrected endovascularly via the access route.
Literature:
- Rha JH, Saver JL: The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 2007; 38: 967-973.
- Berkhemer OA, et al: A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11-20.
- Saver JL, Goyal M, Diener HC, SWIFT PRIME Investigators: Stent-Retriever Thrombectomy for Stroke. N Engl J Med 2015 Sep 10; 373(11): 1077.
- Campbell BC, et al, EXTEND-IA Investigators: Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015 Mar 12; 372(11): 1009-1018.
Further reading:
- Grech R, Schembri M, Thornton J: Stent-based thrombectomy versus intravenous tissue plasminogen activator in acute ischaemic stroke: A systematic review and meta-analysis. Interv Neuroradiol 2015 Oct 21. pii: 1591019915609133 [Epub ahead of print].
InFo NEUROLOGY & PSYCHIATRY 2015; 13(6): 4-6.