Chemotherapy (CT) is the standard treatment for non-resectable, locally advanced pancreatic cancer. The CONKO-007 study investigated the role of sequential CT and chemoradiotherapy (CRT). The first results have now been presented.
In the randomized, multicenter Phase 3 study, resectability was assessed by an independent surgical board. Patients received three months of induction chemotherapy (3 cycles of gemcitabine [gem, 1000 mg/m², on days 1, 8, 15, q4w] or FOLFIRINOX [6 cycles, q2w]). After induction, patients without progression were randomized to either continue CT for another three months or to receive CRT (cumulative dose of 50.4 Gy, single dose 1.8 Gy + Gem 300 mg/m² weekly, followed by one cycle of Gem 1000 mg/m² on days 1, 8, 15).
The primary endpoint of the study was overall survival (OS) since the start of induction chemotherapy (IC). A total of 830 patients were to be included and 590 patients randomized. Due to delayed patient recruitment, the primary endpoint was changed to the rate of R0 resections, resulting in an estimated sample size of 525 patients.
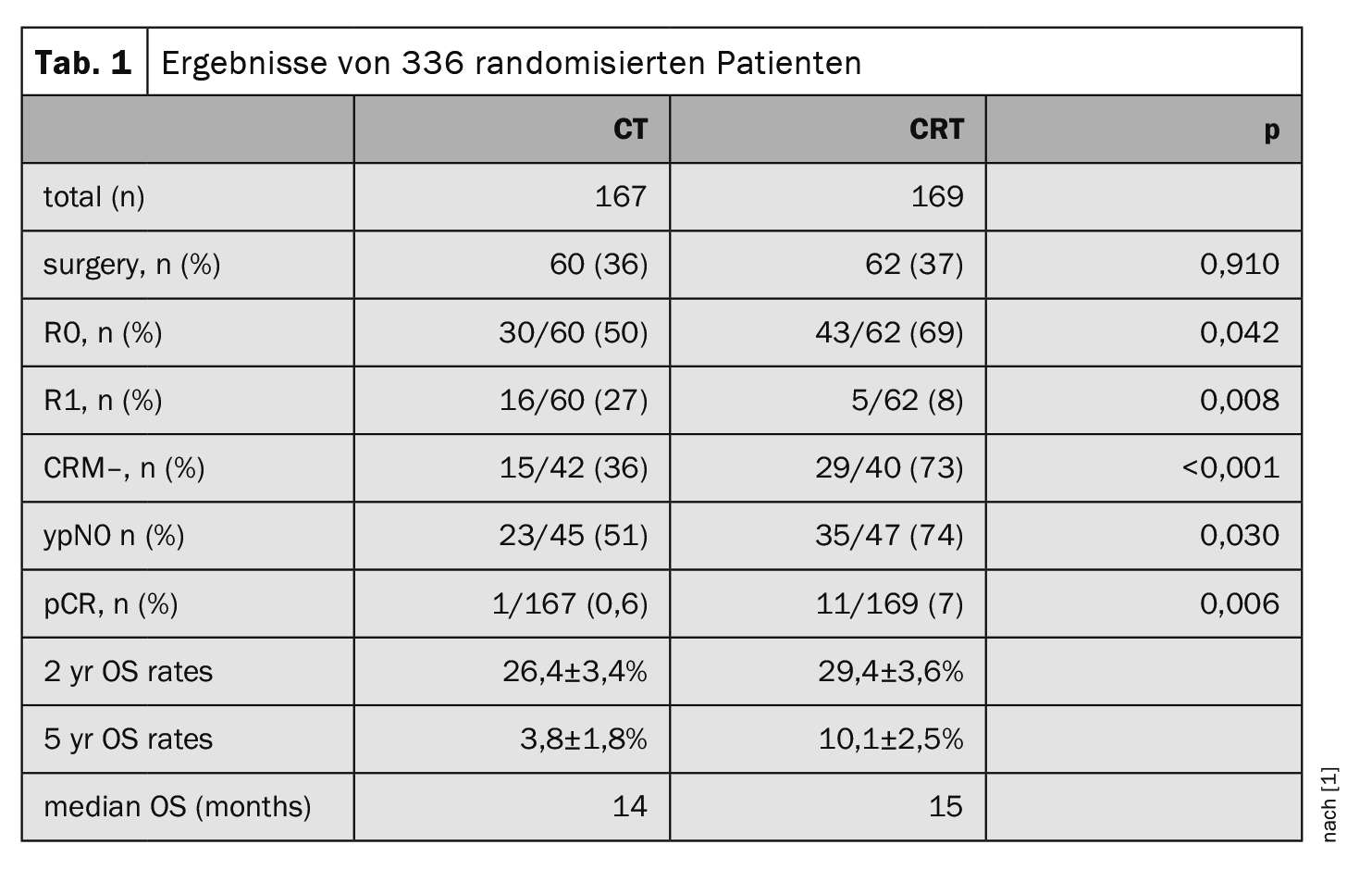
Between 04/2013 and 02/2021, 525 patients were recruited in 47 centers. 402 patients received IC with FOLFIRINOX and 93 patients with Gem. After IC, 159 patients were excluded due to progression or toxicity and 336 were randomized (Table 1) . Their median FU was 16 months. The hematologic toxicities were significantly increased with CRT, the non-hematologic toxicities were comparable.
R1 resections significantly more frequent
The evaluation of the study group led by Prof. Dr. Robert Grützmann, Department of Surgery, University Hospital Erlangen, showed that R0 resections, CRM resections and pCR rates were significantly higher in the CRT group. R1 resections occurred significantly more frequently in the CT group. The OS rates (HR 0.936; 95% CI 0.747-1.174, p=0.567) did not differ significantly in the two arms, but the 5-year OS rates showed a 2.7-fold survival benefit in the CRT arm. The OS rates for R0 resection were significantly higher (p<0.01) at 49.9 ± 5.9% (2 years) and 27.6 ± 6.0% (5 years) than for R1 resection at 23.8 ± 9.3% (2 years) and 11.9±7.6% (5 years) and for patients with no or incomplete surgery at 21.6 ± 2.7% (2 years) and 0% (5 years).
The addition of radiotherapy after IC improves the resection outcome (R and CRM status) as well as the pCR rate without significantly improving the survival data, the scientists conclude. Patients with R0 resections had a better prognosis than patients with R1 resections, incomplete or no surgery.
Congress: Viszeralmedizin 2023
Source:
- Grützmann R: Vortrag «Randomized phase III trial of induction chemotherapy followed by chemoradiotherapy or chemotherapy alone for non-resectable locally advanced pancreatic cancer: First results of the CONKO-007 trial»; Sitzung «Pankreaskarzinom 2023 – Update: Risikofaktoren, Bildgebung, Endosonographie, (Radio)Chemotherapie und Resektabilität»; Viszeralmedizin 2023, Hamburg, 14.09.2023; Z Gastroenterol 2023; doi: 10.1055/s-0043-1771692.
GASTROENTEROLOGIE PRAXIS 2023: 1(2): 32
InFo ONCOLOGY & HEMATOLOGY 2023; 11(6): 36