For the first time, the current guidelines focus on chronic coronary syndrome instead of the previously commonly used term stable coronary artery disease. In addition, new data once again support the importance of lifestyle as the basis for successful drug therapy. However, in addition to basic therapy, novel therapeutic approaches may also be considered in treatment. These may play a central role in addition to myocardial revascularization.
Clinical practice has shown that “stable” coronary artery disease (CAD) is often a progressive disease with recurrent cardiovascular events. Therefore, a new terminology has been officially introduced in the updated guidelines of the European Cardiology Society: Chronic coronary syndrome (CCS). CCS is a dynamic process consisting of increasing deposition of atherosclerotic plaques as well as functional changes in coronary circulation. Both aspects can be influenced by lifestyle changes, pharmacological therapy, or revascularization so that stabilization or regression of the disease can be achieved [2].
Indications for revascularization
The decision for revascularization by percutaneous coronary intervention (PCI) or coronary artery bypass is based on the clinical picture (symptom control) and previous documentation of ischemia (ischemic cardiomyopathy with left ventricular ejection fraction (LVEF) <35%). In the absence of ischemia, the indication for revascularization depends on invasive assessment of the degree of stenosis or prognostic indications, which include stenosis >90% or evidence of fractional flow reserve (FFR) <0.8. Performing an FFR in patients with chronic coronary syndromes has been shown to provide a prognostic advantage and to determine the prognosis and effect of PCI [3,4].
Optimal medical therapy
A healthy lifestyle (healthy diet and weight, physical activity, and smoking cessation) is the basis of successful therapy for chronic coronary syndrome. Drug therapy aims to minimize event rates and symptom progression. The mainstays of this therapy include statins, acetylsalicylic acid, and ACE inhibitors and AT1 antagonists. Data to date on chronic coronary syndrome show that the effect for ACE inhibitors correlates with LV function, ie, the worse the ventricle the better the mortality reduction by RAS inhibition in acute coronary syndrome. For beta-blockers, on the other hand, there is a reassessment. Similar to hypertension, beta-blockers are always indicated in chronic coronary syndrome when there are no symptoms but there are problems with the left ventricle, such as in patients with heart failure or after myocardial infarction. If the ventricle is unremarkable and there is no myocardial infarction, studies have shown no prognostic effect for the beta-blocker. Furthermore, there is no prognostic effect for antianginal therapeutic strategies such as nitrates, ranolazine, or ivabradine in the indication of chronic coronary syndrome.
Novel therapeutic approaches
According to Prof. Dr. Ulrich Laufs, Medical Faculty and University Hospital Leipzig (D), Clinic and Polyclinic for Cardiology, in addition to basic therapy, novel therapeutic approaches in the area of atherothrombosis, inflammation, metabolism, and lipoproteins can reduce cardiovascular risk and help in the treatment of chronic coronary syndrome (Fig. 1) [1,5].
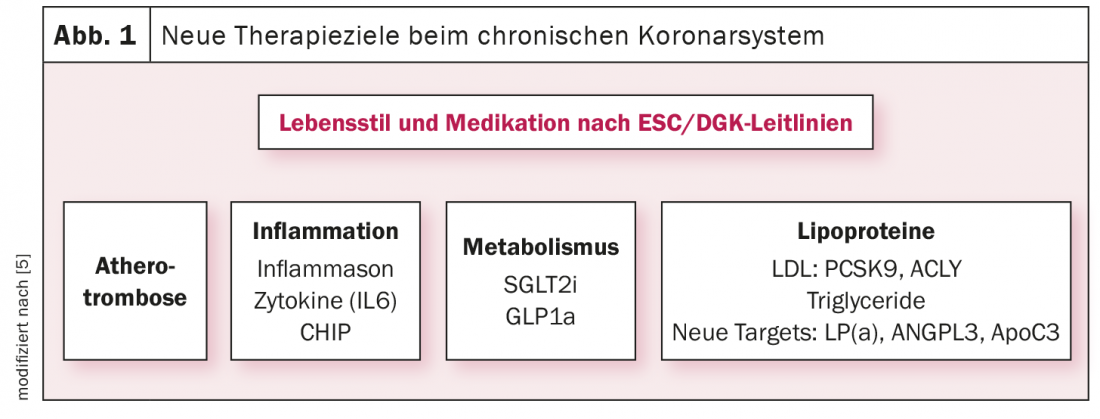
Atherothrombosis: In patients at high risk for an ischemic event and without a high risk of bleeding, a second antithrombotic agent should be considered in addition to aspirin for long-term secondary prevention (e.g., ASA + rivaroxaban 2.5 mg bid [6]).
Inflammation: independent of other cardiovascular risk factors, inflammation is amenable to prognosis with the right strategy. Interleukin-6 (IL-6), for example, is predictive and specific in addition to other risk factors. Currently, the ZEUS study is testing specific interleukin-6 inhibition in patients in secondary prevention with renal failure.
Metabolism: In patients with diabetes and manifest atherosclerosis, it is recommended to start with SGLT2 inhibitor or GLP1-RA rather than metformin, because neither positive meta-analyses nor positive placebo-controlled trials of metformin exist for this population. From a secondary prevention perspective, obesity may also become a new therapeutic target in the next two to three years.
Lipoproteins: LDL cholesterol levels for prevention of cardiovascular disease should be <1.4 mmol/L (<55 mg/dL). Non-HDL cholesterol and apo B represent secondary targets because the evidence in this regard from randomized trials is weaker than for LDL cholesterol. In patients with “atherosclerotic cardiovascular disease” (ASCVD) who experience a second vascular event (not necessarily of the same type as the first event) within 2 years while receiving maximally tolerated statin-based therapy, it is recommended to lower LDL cholesterol to <1.0 mmol/L (40 mg/dL) [7].
Theses for improvement
A study has shown that low-density lipoproteins (LDL) cause atherosclerotic cardiovascular disease (ASCVD). Atherosclerosis is one of the diseases that is preventable. Thus, if LDL is lowered by 50% for life, much of the atherosclerosis could be prevented [8]. Lauf’s first suggestion for improvement is therefore to introduce child screening for LDL-C at U9. To begin with, every 250. Child to discover that has a homozygote familial hypercholesterolemia and then reverse the families of that child to identify. And second, to bring LDL to the awareness of all of us. Lauf’s second suggestion is to use early combination therapy [9] and to use a fixed dose of combination drugs [10]. The third and final proposal involves considering new health policies. For example, the U.K. health system and the manufacturer of Inclisiran (ALN-PCSsc), a long-acting RNA interference (RNAi) therapeutic that inhibits the synthesis of proprotein convertase subtilisin kexin type 9 (PCSK9), have signed a world-leading agreement to bring Inclisiran to 300,000 patients with high cholesterol and a history of cardiovascular disease over the next three years at an affordable and cost-effective price. [11].
Take-Home Messages
- Indication for revascularization: angina, hemodynamically relevant stenoses, ICM.
- Basic therapy: healthy lifestyle; pronostic: ASA, statins, ACEi/ARB in HTN; symptomatic: BB, nitrates, ranolazine, ivabradine.
- New therapeutic targets: Atherothrombosis, inflammation, metabolism, lipoproteins.
Literature:
- Prof. Dr. Ulrich Laufs: Drug therapy and revascularization in chronic coronary syndrome, DGIM Management des chronischen Koronarsyndroms, 30.04.2022.
- Knuuti J, et al: 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal 2020; https://doi.org/10.1093/eurheartj/ehz425.
- Völz S, et al: Survival of Patients With Angina Pectoris Undergoing Percutaneous Coronary Intervention With Intracoronary Pressure Wire Guidance. JACC 2020; doi: 10.1016/j.jacc.2020.04.018.
- Sud M, et al: Association Between Adherence to Fractional Flow Reserve Treatment Thresholds and Major Adverse Cardiac Events in Patients With Coronary Artery Disease. JAMA 2020; doi: 10.1001/jama.2020.22708.
- Reiner Z, et al: The year in cardiology 2018: prevention. European Heart Journal 2021; https://doi.org/10.1093/eurheartj/ehy894.
- Eikelboom JW, et al: Rivaroxaban with or without aspirin in Stable Cardiovascular Disease. N Engl J Med 2017; doi: 10.1056/NEJMoa1709118.
- Mach F, et al: 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). European Heart Journal 2019; https://doi.org/10.1093/eurheartj/ehz455.
- Ference BA, et al: Low-density lipoproteins cause atherosclerotic cardiovascular disease. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. European Heart Journal 2017; https://doi.org/10.1093/eurheartj/ehx144.
- Ray KK, et al: Combination lipid-lowering therapy as first-line strategy in very high-risk patients. European Heart Journal 2022; https://doi.org/10.1093/eurheartj/ehab718.
- Katzmann JL, et al: Non-statin lipid-lowering therapy over time in very-high-risk patients: effectiveness of fixed-dose statin/ezetimibe compared to separate pill combination on LDL-C. Clin Res Cardiol 2022; doi: 10.1007/s00392-020-01740-8.
- NHS cholesterol-busting jab to save thousands of lives. NHS England 2021. www.england.nhs.uk/2021/09/nhs-cholesterol-busting-jab-to-save-thousands-of-lives
Congress: DGIM Management of Chronic Coronary Syndrome
CARDIOVASC 2022; 21(3): 20-21