The 23rd World Congress of Dermatology was held in Vancouver in June. In addition to the large, prominently placed studies, various smaller studies were also convincing with their interesting approaches and research questions. We present some such results from the subject area “scalp and hair”.
An Australian research group conducted a retrospective study to determine how melanomas on the scalp present clinically and histologically. They drew on data from a Melbourne clinic over the past 20 years. On the one hand, the aim was to better define the subgroup so that detection and treatment could be carried out more quickly in the future, and on the other hand, the collected characteristics were compared with those of other melanomas of the head and neck region. According to the current literature, these have a worse prognosis overall than those on the rest of the body. Melanomas of the scalp are considered particularly aggressive and characteristic, yet few studies have examined this subgroup as a separate entity.
After collecting clinical and histopathologic data from 1469 primary cutaneous head and neck melanomas, the researchers subdivided the cases by site of the finding: face, neck, ear, and scalp, respectively. The latter group included 304 melanomas. Compared with the other head and neck melanomas, these were significantly less likely to be in situ carcinomas (20.8 vs. 41.4%). In addition, invasive scalp melanomas differed significantly with respect to tumor subtype: there were more desmoplastic (12.9 vs. 4.3%) and nodular (26.6 vs. 16.1%) subtypes, but fewer lentigo-maligna (34.4 vs. 42.2%) and superficial spreading melanomas (24.5 vs. 34.6%). Mean Breslow thickness was higher at the scalp than elsewhere (3.6 vs. 2.1 mm, p<0.01).
Significant differences were found not only related to the appearance of the melanomas themselves, but also related to their carriers: patients with scalp melanomas were older (67 vs. 61.1 years) and more often men (79.6 vs. 54%).
Given the numerous unique features, the authors conclude that it is worth characterizing scalp melanomas as a distinct subgroup.
Alopecia accompanying therapy
Nowadays, once a tumor has been diagnosed (be it melanoma or another type of cancer), it is often followed by targeted cancer therapy with agents that target oncogenic signaling pathways and/or proteins at the molecular level. Such approaches, in turn, not infrequently have an impact on the (head) skin or hair. Although such changes exert a decisive influence on quality of life, they receive little attention in research. This is in contrast to other dermatologic conditions such as rashes, pruritus, and mucositis, which can limit the dosage of targeted anticancer therapy. Since alopecia and other changes in hair have rarely been clinically recorded in such studies, much is still unclear in this area.
At the World Congress of Dermatology, U.S. researchers now presented results of a structured review describing the effects of a total of 35 different targeted cancer therapies on hair. Data sources were Pubmed, Web of Science, and the ASCO annual meetings abstracts’ database. The review included 82 case reports and case series describing hair changes and/or alopecia in the course of cancer therapy. According to the authors, this is currently the best available evidence on the topic.
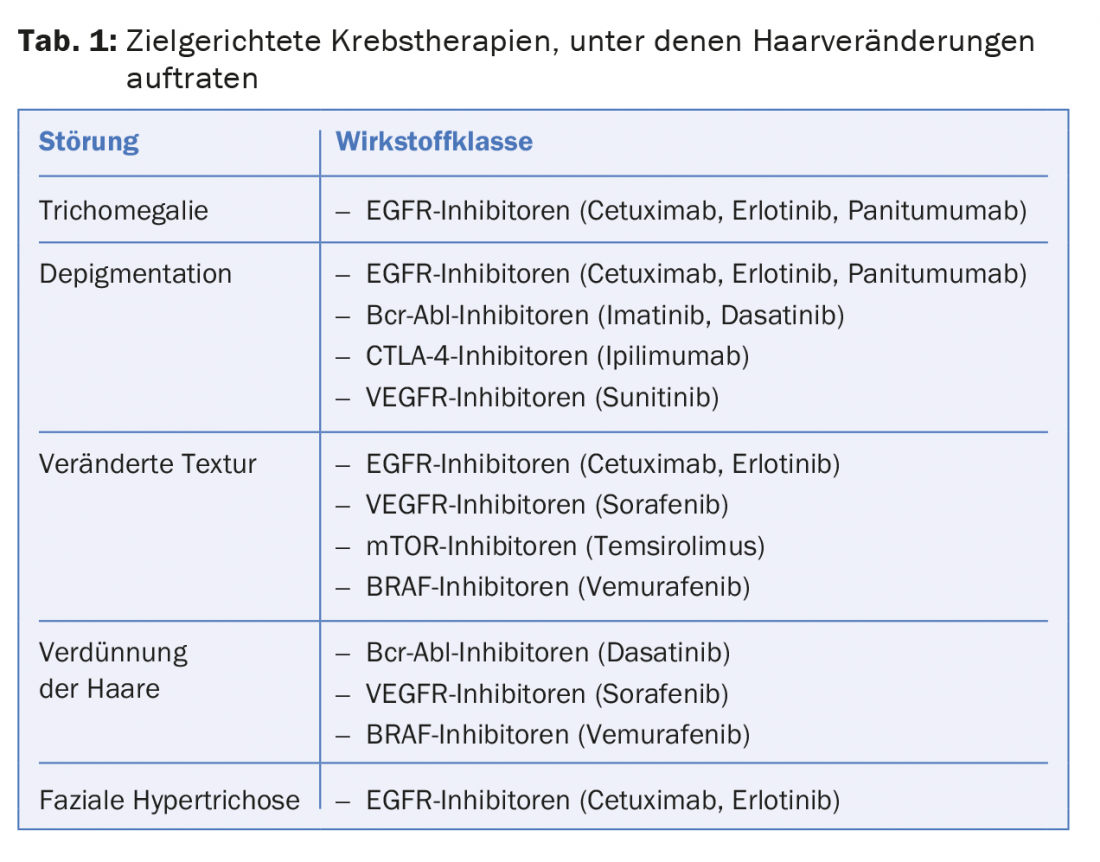
The alopecias that occurred during targeted cancer treatment mostly involved the scalp and were sometimes diffuse in appearance, sometimes localized/irregular patchy, and rarely scarring. Most frequently, scarring alopecia or folliculitis decalvans was found concomitant with treatment with EGFR inhibitors (erlotinib n=3; gefitinib n=2). Other hair changes are described in Table 1. Overall, the researchers concluded that targeted therapies may be associated with a variety of different hair changes. More precise findings on the extent to which the molecules act on hair follicles would be exciting in this context. In order not to unnecessarily compromise patients’ quality of life, the authors recommend appropriate counseling prior to therapy and prompt recognition of such problems or referral to a dermatologist.
Lichen planopilaris – New subtype?
The most common form of non-scarring hair loss is androgenetic alopecia (AGA). However, one should not be hasty in assuming this diagnosis, sometimes other diseases mimic its appearance. One such case was presented at the congress: According to the authors, it is a new, hitherto little-known subtype of lichen planopilaris (LPP).
In a cross-sectional study, the researchers reviewed how many of the 650 patients included with the appearance of AGA actually had lichen planopilaris. Two-thirds of the participants were male. Overall, 58 patients (8.9%), 52 of them women, showed pathologic evidence of lichen planopilaris (perifollicular fibrosis, lichenoid infiltration around the infundibulum of miniaturized hairs). The authors conclude that this is a new subtype of lichen planopilaris that presents clinically as follows: Predominant terminal hair with significantly decreased vellus hair, loss of follicular ostia, perifollicular erythema, and multiple tiny punctate scars. Overall, the appearance resembles an AGA. Another LPP subtype that also occurs in the areas of AGA is the so-called “fibrosing alopecia in a pattern distribution” (FAPD). The tiny punctate scars without progressive scarring alopecia of the central scalp clinically distinguishes the new form from FAPD.
Therefore, the investigators recommend that a biopsy be performed in the clinical finding of diffuse hair loss with the same distribution as in AGA, sparse vellus hair, and predominant terminal hair.
Dutasteride against hair loss
The question of whether dutasteride is more effective than finasteride against androgenetic alopecia was also raised at the Congress. An open-label randomized controlled trial compared the effect of 0.5 mg dutasteride with that of 1 mg finasteride daily for 24 weeks in 90 men with AGA (18-40 years). The dose of dutasteride was thus equivalent to that used in benign prostatic hyperplasia, the actual indication for the drug. By phototrichogram, hair density and thickness were collected at baseline and after 24 weeks. General photographic inventories, assessed by a blinded and a nonblinded investigator, and subjective assessment by patient questionnaire supplemented the evaluation.
Compared with finasteride, the dutasteride group showed a significant increase in total hair density and the number of thick hairs, accompanied by a decrease in the number of thin hairs, at the approximately 1 cm2 shaved area studied after 24 weeks. General photographic inventory also showed a significant benefit with dutasteride, while side effect profiles (including sexual dysfunction) were comparable.
Source: 23rd World Congress of Dermatology, June 8-13, 2015, Vancouver.
DERMATOLOGIE PRAXIS 2015; 25(5): 40-42











